Health Equity → Health Equity and the National DPP → Connecting SDOH and HRSN to Prediabetes and Type 2 Diabetes
Connecting SDOH and HRSN to Prediabetes and Type 2 Diabetes
Research shows consistent and significant disparities in diabetes outcomes across populations. Many studies have shown that diabetes impacts racial and ethnic minority and low-income adult populations disproportionately as evidenced by a higher risk of type 2 diabetes and higher rates of diabetes complications and mortality. This high risk is largely related to social determinants of health (SDOH) and health-related social needs (HRSN).1 This page summarizes how SDOH and HRSN relate to prediabetes and type 2 diabetes, and is divided into the following sections:
- Research Shows a Strong Connection Between SDOH, HRSN, and Diabetes
- The Value of Understanding Diabetes-Related Health Disparities
Research Shows a Strong Connection Between SDOH, HRSN, and Diabetes
Many studies over the last several decades have shown disparities in diabetes outcomes across populations with different SDOH. For example, populations with higher education and income levels have more access to care and preventive services, better health behaviors and control, better cardiometabolic outcomes, and a longer life expectancy when compared to those with lower socioeconomic status (SES).2,3,4,5 This research indicates that diabetes is largely influenced by broader social context.6
The table below summarizes the connection between diabetes and SDOH. Note that some research specifies the type of diabetes (type 1 or type 2), whereas other research refers to diabetes generally and may include type 1 and type 2. When type 2 diabetes is specified in the research, it is noted accordingly on this page. For a detailed review of the connection between SDOH and diabetes, please see the publication Social Determinants of Health and Diabetes: A Scientific Review.
The Connection Between SDOH and Diabetes
Economic Stability
Many studies show a clear association between diabetes prevalence and complications and economic stability. Individuals with lower SES are more likely to have type 2 diabetes, experience complications, and die sooner than those with a higher SES.7,8
Individuals with prediabetes who live in areas associated with lower income, lower educational attainment, and high reliance on Supplemental Nutrition Assistance Program (SNAP) benefits also show a higher risk for developing type 2 diabetes.9 Adults with type 2 diabetes living below the federal poverty level have a risk of diabetes-related mortality that is twice as high as those with the highest family income levels.10 An inverse association between income and HbA1C levels has also been observed among adults with type 2 diabetes.11
Occupational factors have also been linked with prediabetes and/or type 2 diabetes including:
- High job insecurity12
- Unemployment13
- Exposure to shift work (vs. normal day time schedules)14
- Long work hours15
A U.S. population-based survey on diabetes and occupation found the highest prevalence of diabetes among transportation workers and the lowest prevalence of diabetes among physicians.16,17
Food Security
Food security is associated with economic stability and has been shown to impact type 2 diabetes prevalence. About 20% of patients with diabetes report food insecurity in their households. Food security improves diabetes management and type 2 diabetes outcomes.18,19,20,21,22 Studies have shown that higher access to food (particularly grocery stores and full-service restaurants) is associated with lower type 2 diabetes rates in both metro and non-metro U.S. counties.23
Education Access and Quality
Educational attainment has been associated with type 2 diabetes prevalence.24 Adults with a college education have the lowest odds of developing type 2 diabetes.25 The risk of diabetes-related mortality is also associated with educational attainment. Individuals with less than a high school education are associated with a diabetes-related mortality rate two times higher than those with a college degree.26 Lower educational attainment is also associated with higher HbA1c levels.27 Additionally, health literacy has been shown to be significantly associated with lower HbA1c levels and increased diabetes knowledge.28
Health Care Access and Quality
Access, affordability, and quality of health care are associated with diabetes prevalence and outcomes. These metrics are also highly associated with race/ethnicity, SES, and geography in the United States.29 The average health care costs of individuals with diabetes are 2.3 times greater than individuals without diabetes.30 Approximately 14-20% of adults with diabetes report reducing or delaying medication due to cost.31,32,33 Adults with lower household incomes (less than $50,000) and uninsured adults are also more likely to engage in health care cost-related nonadherence (CRN).34 Individuals with lower incomes, persons of color, and women have been shown to experience disparities in quality of diabetes care.35,36
Health insurance coverage has been shown to be the strongest predictor of whether adults with diabetes have access to diabetes care.37 Adults without insurance are more likely to have undiagnosed diabetes than those who are insured.38 Geographic availability of health care providers varies substantially in the United States with lower access in areas associated with high diabetes rates and socioeconomic disadvantage.39,40 Individuals who are uninsured and without a usual source of care have 3‒5 times lower odds of receiving HbA1c screenings, blood pressure tests, or access to needed urgent care.41
Neighborhood and Built Environment
The precise prevalence of diabetes among U.S. adults experiencing housing insecurity is not known; however, one study of individuals receiving care from community health centers found that about 37% of individuals with diabetes reported housing insecurity. These individuals were also more likely to report having an emergency department visit or being hospitalized for diabetes.42
Additional research has also connected housing insecurity to worse health outcomes and less access to care.43,44,45,46,47,48 Qualitative research has shown that unstable housing makes it more difficult to engage in self-care, follow self-management routines, afford needed medications and supplies, and eat healthy foods.49,50 Unstable housing has been identified as a key barrier to diabetes care among low-income individuals.
Results from several studies show that living in a neighborhood with better walkability and access to greenspace is consistently associated with lower risk of type 2 diabetes.51,52,53,54 Populations more exposed to air pollution are disproportionately at risk for developing type 2 diabetes and evidence from several studies show an increased diabetes risk in populations exposed to environmental chemicals.55,56,57,58,59,60,61 Environmental exposures also increase susceptibility to cardiovascular disease (CVD) in people with diabetes.62.63 Air pollution exposure is related to increased risk of stroke mortality, increased vascular reactivity, and inflammation in those with diabetes compared to those without.64,65,66
Social and Community Context
High levels of social cohesion (measured through trust, shared values, and willingness to help neighbors) was associated with a 22% lower incidence of type 2 diabetes.67 Additional studies show higher social support is associated with better glycemic control and improved quality of life.68,69,70,71,72 Moreover, lack of social support has been associated with diabetes-related mortality complications.73
Some research suggests that social capital, cohesion, and support may influence (or be influenced by) structural racism. One study showed that women with the most exposure to everyday racism had a 31% higher risk of diabetes than those with the lowest exposure; though this association was mediated by BMI.74 That said, additional research is needed to understand the intersection between social environment and inequities in diabetes outcomes.75
The Value of Understanding Diabetes-Related Health Disparities
Several resources indicate the value of understanding diabetes-related health disparities and how it can inform prevention and control efforts.
- CDC’s U.S. Diabetes Surveillance System: CDC has expanded the U.S. Diabetes Surveillance System with a new SDOH module to help identify under-resourced areas of the United States and assess the potential impact of health disparities on diabetes burden and risk factors.
- The Connection between COVID-19 and Type 2 Diabetes: In August 2021, NACDD released a white paper on the connection between COVID-19 and type 2 diabetes underscoring the need for chronic disease prevention and management. The paper includes state examples that visually highlight the connection between COVID-19 severity and diabetes prevalence along with socioeconomic status, social vulnerability, and race/ethnicity at the regional or county level.
- CDC’s Social Vulnerability Index: CDC’s Social Vulnerability Index (SVI) indicates the relative vulnerability of various counties allowing stakeholders to understand broad social context at a local level. It comprises four aggregated themes and 15 individual variables. The four CDC SVI themes include Socioeconomic Status, Household Composition & Disability, Minority Status & Language, and Housing Type & Transportation. Social vulnerability scores for each of these themes are derived from normalized percentile ranks for each CDC SVI variable.
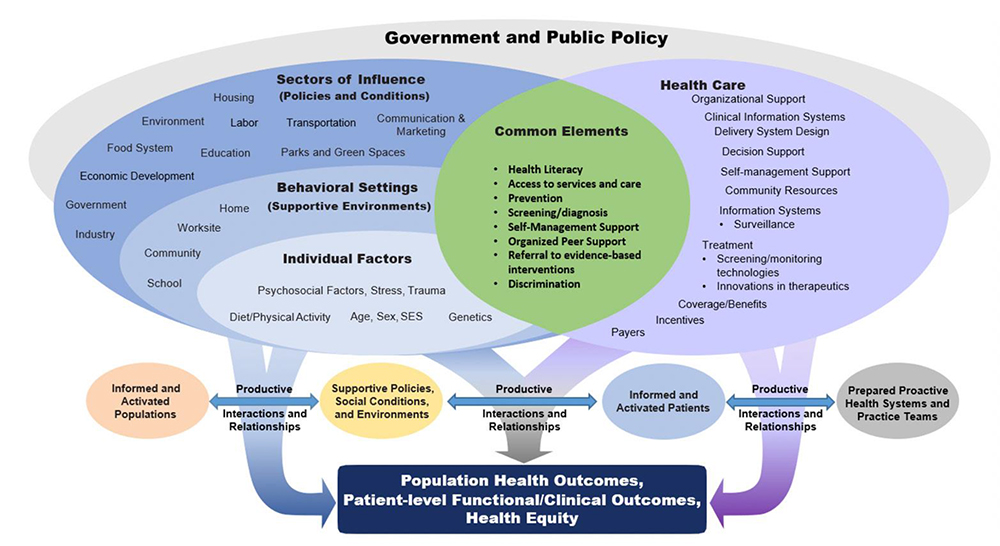
- National Clinical Care Commission Framework for Diabetes Prevention and Control: The National Clinical Care Commission released a report to congress that provides a framework for diabetes prevention and control. This framework shows the complexity of population health outcomes and health equity in relation to diabetes. It demonstrates that a holistic view of complex processes and social context is needed to prevent diabetes and improve health equity. The report states the logic of the framework as follows:
“Diabetes can be prevented or controlled only through supportive policies, social conditions, and environments and by promoting more prepared, proactive health systems and practice teams that enable informed and activated patients. The intended outcomes of these structures and processes include improved clinical outcomes and quality of life for individuals at risk for or with diabetes; better diabetes-related population health; and greater diabetes-related health equity.”
As noted in the framework above, addressing SDOH and HRSN is critical to reducing diabetes-related health disparities. The connection between the National Diabetes Prevention Program (National DPP) lifestyle change program and addressing HRSN is addressed on the Coverage Toolkit page titled, Addressing HRSN Through the National DPP Lifestyle Change Program.
References for sources cited on this page can be viewed here.









