Medicare → MDPP Implementation Resources
Medicare Diabetes Prevention Program (MDPP) Implementation Resources
The following tools, webinars and resources were developed as part of technical assistance for MDPP suppliers through funding and support by the Centers for Disease Control and Prevention (CDC) and implemented by the National Association of Chronic Disease Directors (NACDD). Some of the webinars and resources were developed in collaboration with the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA). Webinar and resource topics include referrals and recruitment, marketing, promoting the MDPP, working with Medicare Advantage (MA) plans, and billing and claims.
To find more information about the MDPP and additional resources, visit our MDPP Basics page or CMS MDPP page.
This page contains the following topics:
- NACDD’s MDPP Business Tools
- MDPP Webinars and Resources
- MDPP and State Health Departments
- MDPP and Health Care Providers
NACDD’s MDPP Business Tools
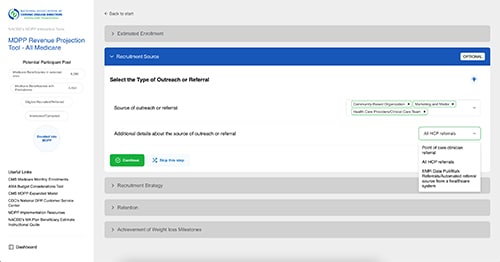
Access the NEW MDPP Revenue Projection Tool on DPPBusinessTools.org.
Through funding from CDC, NACDD is working with CreateApe, a digital product and website design company, to develop DPPBusinessTools.org, a website that will host MDPP Business Tools, developed through feedback from over 60 MDPP suppliers and other partners during NACDD’s MDPP Enrollment Project. These tools are designed to assist potential and existing MDPP suppliers to increase successful implementation of the MDPP.
MDPP Revenue Projection Tool |
MDPP Supplier Capacity Assessment Tool |
MDPP Planning Tool |
| ACCESS WEB-BASED VERSION NOW | WEB-BASED VERSION COMING SOON | WEB-BASED VERSION COMING SOON |
|
|
|
This interactive MDPP Revenue Projection Tool is designed to help an existing or potential MDPP supplier:
|
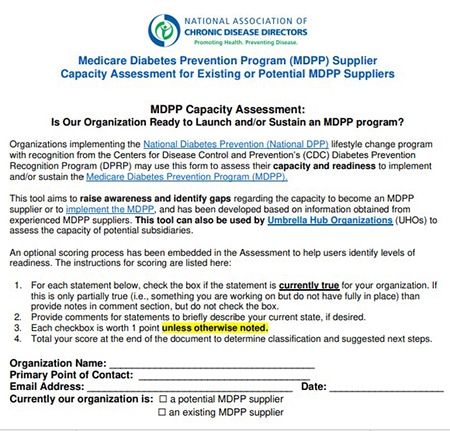
The MDPP Capacity Assessment Tool was developed in 2023 with input from experienced MDPP suppliers. This tool is designed to help CDC-recognized organizations assess their capacity and readiness to become an MDPP supplier and to implement a successful MDPP. Existing MDPP suppliers can use this tool to see areas where they might have gaps and need to increase capacity to be more successful and sustainable. This tool can also be used by umbrella hub organizations (UHOs) to assess the capacity of potential subsidiaries. To learn more about UHOs and subsidiaries, please visit the Umbrella Hub Arrangements pages of the Coverage Toolkit. |
The MDPP Enrollment Planning Template was developed in 2023 with input from experienced MDPP suppliers. This tool is intended to help MDPP suppliers create individualized program plans to increase beneficiary enrollment including plotting out types and timing of initiatives and launching of cohorts. This template can also be used to set and track referral and enrollment goals, and to engage leadership around needed support and future planning.
This tool can also be used by UHOs for assessment and planning of potential subsidiaries. To learn more about UHOs and subsidiaries, please visit the Umbrella Hub Arrangements pages of the Coverage Toolkit. |
MDPP Webinars and Resources
CDC, CMS, AMA, NACDD, and other partners have worked collaboratively to host various informational webinars and learning opportunities geared towards promoting the MDPP. Please note that the resources below were developed for a specific technical assistance opportunity and often include titles and dates associated with that purpose; however, they can and should be used by any MDPP supplier interested in learning more about how to be successful offering the MDPP.
The table below is organized by topic and lists the webinars with accompanying resources for each category.
Overarching Resources
Resources:
- NACDD’s MDPP Enrollment Project Overview – From November 2020 to August 2023, NACDD’s Coverage Team focused efforts to increase Medicare beneficiary enrollment into the MDPP through the MDPP Enrollment Project. This project worked with over 60 MDPP suppliers in 27 states, and the planning and technical assistance team included NACDD, CDC, the AMA, Welld Health, and MDPP supplier peer mentors.
- MDPP All Project Call and Summary – On June 26th, 2023, NACDD hosted a call that promoted the sharing of best practices from various MDPP technical assistance offerings available to state health departments and MDPP suppliers. Participants provided an overview of successful initiatives to increase enrollment to and payment for the MDPP, and NACDD consultants reviewed available MDPP resources. CDC provided perspective on the program, and CMS joined to answer MDPP supplier’s questions.
- MDPP Enrollment Project Small Team TA Summary (2023) – As part of the MDPP Enrollment Project (please visit the NACDD MDPP Technical Assistance page to learn more about this project), NACDD selected a few MDPP Enrollment Project supplier awardees to serve as mentors and lead small group technical assistance calls, called “Small Team Technical Assistance (TA).” This summary resource describes the information that was shared during the Small Team TA meetings, and provides resources and solutions discussed in relation to each barrier. Information is categorized by topic area.
- Spotlight on the Oregon Wellness Network: Partnership Development – Developed in the spring of 2023 from an interview with an MDPP supplier, the Oregon Wellness Network (OWN), that participated in the MDPP Enrollment Project (please visit the NACDD MDPP Technical Assistance page to learn more about this project), this resource provides information on how OWN works with partners and builds lasting relationships that further diabetes prevention efforts in the state of Oregon.
- MDPP Capacity Assessment – Developed in the spring of 2023 with input from experienced MDPP suppliers, this tool is designed to help CDC-recognized organizations assess their capacity and readiness to become an MDPP supplier or to implement the MDPP. This tool can also be used by umbrella hub organizations (UHOs) to assess the capacity of potential subsidiaries (to learn more about UHOs, please visit the Umbrella Hub Arrangements pages of the Coverage Toolkit).
- MDPP Enrollment Plan Template – Developed in 2023 with input from experienced MDPP suppliers, this tool is intended to help MDPP suppliers create an individualized MDPP implementation plan to increase beneficiary enrollment. This template can also be used to set and track goals, and to engage leadership around needed supports and future planning. This tool can also be used by umbrella hub organizations (UHOs) to assess the capacity of potential subsidiaries (to learn more about UHOs, please visit the Umbrella Hub Arrangements pages of the Coverage Toolkit).
Billing and Claims
Webinars:
- Lifecycle of an MDPP Claim – On November 16th, 2023, CDC and NACDD hosted a webinar focused on the lifecycle of an MDPP claim, allowing attendees to explore what happens after a claim is sent to a payer for processing. The goal of this webinar was to give MDPP suppliers a better understanding of the claims submission process and how they might interact with MDPP claims along that journey. Some highlights of the webinar included how to find, interpret, and resolve common rejection and denial codes, partial or non-payment issues, and coverage validation issues. The webinar was presented by Welld Health and was data system agnostic.
- MDPP Supplier Learning Series Billing Workshop Part 1 – On September 22nd, 2021, CDC, CMS, and NACDD hosted part 1 of a 2-part webinar series focused on increasing general knowledge about the MDPP billing and claims processes. Part 1 specifically looked at how MDPP enrollment and the PECOS application processes impact billing.
- MDPP Supplier Learning Series Billing Workshop Part 2 – On November 10th, 2021, CDC, CMS, and NACDD hosted part 2 of a 2-part webinar series focused on increasing general knowledge about the MDPP billing and claims processes. Part 2 specifically looked at the process for submitting a successful MDPP claim to CMS.
Resources:
- Lifecyle of an MDPP Claim Summary: Developed from a webinar NACDD and CDC hosted on November 16th, 2023, this resource details best practices for following the three stages of the lifecycle of an MDPP claim: claim creation, adjudication, and revenue cycle management.
- Working with a Billing Vendor to Refine Electronic Health Record (EHR) Billing Processes for MDPP – Developed in the fall of 2022 from interviews with MDPP suppliers who were also participating in the MDPP Enrollment Project (please visit the NACDD MDPP Technical Assistance Offering Page to learn more about this project), this resource provides information on how MDPP suppliers can work with third-party billing vendors to improve EHR billing processes.
- Working with MACs – Developed from presentations during an informational webinar held on January 19th, 2022, where discussions focused on the basic functions and operations of a Medicare Administrative Contractor (MAC) and how they work with MDPP suppliers. This resource details what a MAC is along with the services they offer, best practices for working with a MAC, and resources to utilize when working with a MAC.
- MDPP Barriers and Potential Solutions – Developed from presentations during an informational webinar held on December 8th, 2021, where MDPP suppliers shared learnings on how to overcome challenges encountered when implementing and sustaining the MDPP. This resource details strategies shared to overcoming barriers with billing and claims, addressing differences between MDPP and the Diabetes Prevention Recognition Program (DPRP) standards, switching between delivery modalities, addressing administrative burdens, and sustainability.
- MDPP Billing Workshop FAQ – Developed from a 2-part webinar series focused on increasing general knowledge about the MDPP billing and claims processes on September 22nd, 2021, and November 10th, 2021. This resource details attendee questions and answers from the webinar series.
- MDPP Enrollment Preparation Guide – Developed by CMS, this resource outlines the steps that organizations with preliminary or full CDC DPRP recognition status can follow to become an MDPP supplier.
Referrals
Webinars:
- Creating Electronic Medical Records (EMR) Referral Pathways for the MDPP Informational Webinars (Part 1 and Part 2) – On February 10th and 17th 2023, NACDD and Welld Health hosted a two-part series focused on how MDPP suppliers can create new referral pathways for the program, including creating a referral pathway through an EMR system. Part 1 focuses on how to establish and grow a referral network, and Part 2 focuses on designing and implementing referral pathways with clinical partners.
- AMA Referrals Technical Assistance Informational Webinar – On February 23rd, 2021, CDC and NACDD hosted an informational webinar where AMA presented on increasing referrals into the MDPP.
- Beneficiary Recruitment and Referral Informational Webinar – On October 20th, 2020, CMS, CDC, and NACDD hosted an informational webinar where various presenters shared best practices and strategies to overcoming barriers for recruitment and referral efforts.
Resources:
- Creating EMR Referral Pathways for MDPP Summary – Developed from a two-part informational webinar series held on February 10th and 17th, 2023, this resource describes how MDPP suppliers can create new referral pathways for the program, including creating a referral pathway through an EMR system.
- Preventing Diabetes in Your Medicare Population Video – The AMA Ed Hub™ created a 4-minute overview for healthcare providers that explains Medicare DPP services, beneficiary eligibility, and the benefits of referring patients to the program.
- MDPP Beneficiary Recruitment Summary – Developed from an informational webinar held on October 20th, 2020, this resource details strategies to increase recruitment into the MDPP. Various presenters shared information regarding targeted outreach campaigns, outreach to senior centers, identifying a clinical champion, and hosting an orientation or session zero. This resource was processed through CMS clearance and appears different from the other resources on this page.
- MDPP Beneficiary Referrals Summary – Developed from an informational webinar held on October 20th, 2020, this resource details strategies shared by various presenters on how to increase referrals into the MDPP. Ideas include building relationships with health care providers, optimizing your electronic health record (EHR), utilizing community advisory boards and community partnerships, and conducting primary care provider (PCP) letter campaigns. This resource was processed through CMS clearance and appears different from the other resources on this page.
- MDPP Referrals Breakout Sessions Summary – Developed from breakout sessions during an informational webinar held on May 18th, 2021, where MDPP suppliers discussed together how to generate referrals into the MDPP. This resource details strategies shared to overcoming barriers with patient identification, referrals, and clinical team engagement.
- Turning Referrals into Enrollment Summary – Developed from breakout sessions during an informational webinar held on October 4th, 2021, this resource details various best practices shared between MDPP suppliers for turning referrals into enrollment as well as possible solutions to barriers preventing an increase in enrollment.
Marketing
Webinars:
- CDC Marketing Technical Assistance Informational Webinar – On January 26th, 2021, CDC and NACDD hosted a webinar where CDC presented on marketing strategies for the MDPP.
Resources:
- Partnership Development to Increase MDPP Referrals and Marketing – Developed in the spring of 2023 from interviews with MDPP suppliers who were also participating in the MDPP Enrollment Project (please visit the NACDD MDPP Technical Assistance Offering Page to learn more about this project), this resource provides information on how MDPP suppliers can partner with and market to other organizations within their community to increase referrals and enrollment into their programs.
- Marketing the MDPP to Medicare Part B Beneficiaries – Find resources specific to marketing the Medicare DPP to Medicare Part beneficiaries and their health care providers from CDC.
Populations of Focus
Webinars:
- Scaling the MDPP with Populations of Focus Informational Webinar: Men, Dual Eligible, and People Living with Disabilities – On March 8th, 2023, CDC, CMS, and NACDD hosted a webinar which explored marketing and delivery strategies designed to engage men in the program as well as a presentation about the creation of inclusive adaptations of the program for people living with disabilities. Finally, CMS presented information about the dual eligible population (i.e., individuals who receive both Medicare and Medicaid benefits).
- Scaling the MDPP with Populations of Focus Informational Webinar: Hispanic, Latino/a, and Spanish-origin Populations – On November 8th, 2022, CDC, CMS, and NACDD hosted a webinar which featured presentations from two MDPP suppliers about their experiences in obtaining referrals for the Hispanic, Latino/a, and Spanish-origin populations they serve as well as their efforts to provide community and culturally appropriate delivery of the MDPP.
- Scaling the MDPP with Populations of Focus Informational Webinar: Asian and African American Populations – On May 10th, 2022, CDC, CMS, and NACDD hosted a webinar which featured presentations from two MDPP suppliers about their experiences in obtaining referrals for African American and Asian American populations as well as their efforts to provide community and culturally appropriate delivery of the MDPP.
Resources:
- Scaling the MDPP with Populations of Focus Summary: Men, Dual Eligible, and People Living with Disabilities – Developed from an informational webinar held on March 8th, 2023, this resource includes information shared by various presenters about ways to engage men, dual-eligible beneficiaries, and people living with disabilities in the MDPP.
- Scaling the MDPP with Populations of Focus Summary: Hispanic, Latino/a, and Spanish-origin Populations – Developed from an informational webinar held on November 8th, 2022, this resource includes information shared by various presenters about ways to engage Hispanic, Latino/a, and Spanish-origin participants in the MDPP.
- Scaling the MDPP with Populations of Focus Summary: Asian and African American Populations – Developed from an informational webinar held on May 10th, 2022, this resource includes information shared by various presenters about ways to engage populations of focus, including African Americans and Asian Americans, in the MDPP.
Working with MA Plans
Webinars:
- MDPP and MA Plans Webinar – On December 15th, 2022, on behalf of NACDD, Welld Health presented a webinar focused on increasing general knowledge about MA plans and the different ways to work with them to successfully bill for MDPP services.
- Working with MA Plans Informational Webinar – On April 28th, 2021, CDC, CMS, and NACDD hosted a webinar which provided an overview of MA plans and the MDPP as well as tips for contracting with and billing MA plans, and offered ways to address challenges when working with MA plans from experienced MDPP suppliers.
Resources:
- MDPP Guide for Medicare Advantage Plans – This document provides an overview and value proposition for the MDPP for an MA plan audience and could be used to introduce an MA plan to the benefits of offering the MDPP. It summarizes key aspects of the MDPP benefit such as how the program is structured, administered, delivered, and certified, and it addresses how MA plans can work and contract with MDPP suppliers to offer the program to their members.
- MA Plan Finder and Beneficiary Estimation Instruction Guide – To seek reimbursement from MA plans, MDPP suppliers may need to contract with a specific plan and may be paid a negotiated payment rate for their services. This guide was developed to help programs find out 1) which MA plan(s) are in their geographic region and 2) approximately how many beneficiaries are enrolled in each plan.
- MDPP and MA Plans Summary – Developed from an NACDD-hosted informational webinar on December 15th, 2022, during which Welld Health discussed MA plans and the different ways to work with them to successfully bill for MDPP services.
- Working with MA Plans Summary – Developed from an informational webinar held on April 28th, 2021, this resource includes eight sections that detail information shared by various presenters including what MA is and how MDPP suppliers can contract and work with MA plans to increase MDPP enrollment. This resource was processed through CMS clearance and appears different from the other resources on this page.
MDPP During the PHE
Webinars:
- Navigating Your MDPP During the PHE Informational Webinar – On January 19th, 2021, CDC, CMS, and NACDD hosted a webinar where various presenters shared approaches to offering the MDPP while navigating the Public Health Emergency (PHE).
Resources:
- CMS announced November 2, 2023, that it will extend the rule that allows all MDPP suppliers to use specific MDPP COVID-19 PHE flexibilities, including the optional virtual delivery of the MDPP set of services through distance learning. The extension of the specified PHE flexibilities will run through December 31, 2027. Additional information regarding the final rule can be found in the Federal Register notice. Questions may be submitted through the MDPP Supplier Support Portal.
- Navigating Your MDPP During the PHE Summary – Developed from an informational webinar held on January 19th, 2021, various presenters shared how they have continued to offer the MDPP during the PHE. This resource details options for transitioning to virtual delivery, adapting to a new normal, and how to thrive not just survive during the PHE. This resource was processed through CMS clearance and appears different from the other resources on this page.
CMS Physician Fee Schedules (PFS)
Resources:
- CMS Calendar Year MDPP Payment Rates – The current MDPP payment rate include both fee-for-service payments for attendance and performance-based payments for meeting weight loss incentive requirements. The rates are updated periodically and go through public commenting period before finalization.
- CMS Calendar year 2024 MDPP PFS Fact Sheet – On November 2, 2023, CMS issued the Calendar Year (CY) 2024 MDPP PFS Fact Sheet that describes the finalized changes to the MDPP expanded model beginning on January, 1, 2024.
Potential New MDPP Suppliers
The resources and tools listed below are for organizations considering becoming an MDPP supplier or for new MDPP suppliers.
- Coverage Toolkit MDPP Basics Page – This page of the Coverage Toolkit gives a brief overview of the MDPP. It includes information about MDPP services and eligibility for beneficiaries and MDPP suppliers. Additionally, details about reimbursement for the MDPP, beneficiary incentives, and Medicare Advantage (MA) are included.
- CMS MDPP Page – This page describes the background of the MDPP and displays an interactive map of current MDPP supplier locations. CMS evaluation reports on the MDPP are provided along with an extensive list of links to CMS-developed resources to assist with MDPP orientation, CDC recognition for MDPP suppliers, and MDPP services.
- MDPP Orientation Video – Provides an overview of the MDPP for organizations interested in becoming suppliers.
- CMS MDPP Enrollment Tutorial Video – The MDPP Enrollment Video is targeted at potential MDPP suppliers to help them complete their MDPP Medicare enrollment. The video is a step-by-step tutorial of a fictional organization completing the PECOS application.
- MDPP Enrollment Preparation Guide – Developed by CMS, this resource outlines the steps that organizations with preliminary or full CDC DPRP recognition status can follow to become an MDPP supplier.
- MDPP Capacity Assessment Tool – This tool can help CDC-recognized organizations assess their capacity and readiness to implement and/or sustain the MDPP. The capacity assessment aims to raise awareness and identify gaps regarding capacity of becoming an MDPP supplier.
- MDPP Supplier Learning Series Billing Workshop Part 1 – On September 22nd, 2021, CDC, CMS, and NACDD hosted part 1 of a 2-part webinar series focused on increasing general knowledge about the MDPP billing and claims processes. Part 1 specifically looked at how MDPP enrollment and the PECOS application processes impact billing.
MDPP and State Health Departments
Successful implementation of the MDPP is a priority for state health departments (SHD). It is important for MDPP suppliers to know the roles of SHDs and learn more about how SHDs can support both suppliers and beneficiaries in their state. Please find the SHD Roles for Supporting MDPP Suppliers document, which reviews the ways in which SHDs can support the MDPP.
With support from CDC, NACDD helps increase access to and utilization of the MDPP by providing technical assistance to CDC-recognized organizations and SHDs. As part of this technical assistance, NACDD supports CDC-recognized organizations becoming Medicare suppliers, enrolling participants, and submitting claims. NACDD also supports SHD staff and national organization staff who in turn support the CDC-recognized organizations in their state. Visit the NACDD MDPP Technical Assistance page to learn more.
For those who would like an introduction to the MDPP or would like help with specific activities such as presenting the MDPP to leadership, onboarding new staff, or working with Medicare Advantage plans, below is a quick (~10 minute) video that reviews the basics of MDPP.
MDPP and Health Care Providers
These videos were developed to encourage health care teams to work together and with their patients to identify prediabetes and increase referrals to the National DPP lifestyle change program. These videos were created by NACDD in collaboration with the AMA and through support from the CDC, Division of Diabetes Translation.Team-Based Care: Clinical Care Management and the National DPP
This video, based in a hospital, highlights the responsibility of care management in implementing and sustaining effective diabetes prevention strategies by health care providers, including referrals to the National DPP lifestyle change program.
Timing: 3:18 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Team-Based Care: Clinical Care Team Roles and Responsibilities for Diabetes Prevention
This video, based in a clinical setting, explores the different roles health care team members can play in identifying patients with prediabetes and providing care and follow-up, including referrals to the National DPP lifestyle change program.
Timing: 4:05 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Clinical Care: Prediabetes Identification and Treatment
This video illustrates how health care providers can help their patients address prediabetes through referral to the National DPP lifestyle change program.
Timing: 4:18
Audience: Clinical Care team (physician, nurse practitioner, physician’s assistant, nurse, medical assistance, care manager, care coordinator, etc.)