Medicaid → State Stories of Medicaid Coverage → Pennsylvania
Pennsylvania’s State Story of Medicaid Coverage
Establishing Coverage
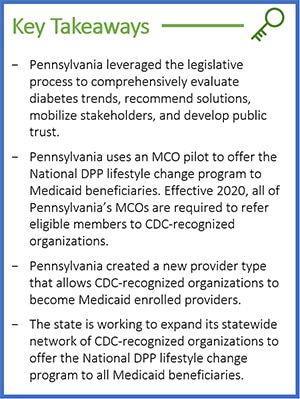
Pennsylvania currently offers the National Diabetes Prevention Program (National DPP) lifestyle change program to Medicaid beneficiaries. Effective 2020, all of Pennsylvania’s managed care organizations (MCOs) are required to offer the National DPP lifestyle change program to their beneficiaries.
Initial Steps Towards Medicaid Coverage
- 2014: The Pennsylvania Department of Health (PADOH) was awarded a CDC Preventive Health and Health Services Block Grant (PHHSBG) of $915,000. PADOH worked in four under-served and/or rural regions (South West, South Central, South East, North East) and during subsequent years expanded statewide to provide technical assistance support to organizations obtaining their CDC recognition. Through the work of the CDC PHHSBG funding the number of CDC-recognized organizations grew from 13 in 2015 to 54 in 2017, and to 69 in 2018. In addition to technical assistance support for organizations seeking their CDC recognition, the PHHSBG also funded Lifestyle Coach trainings and certified four master trainers until 2018, when PADOH began supporting the Lifestyle Coach trainings solely with 1815 Grant funds.
- 2015: PADOH provided a cost benefit analysis for diabetes prevention to the Pennsylvania Medicaid Director. PADOH and the Pennsylvania Department of Human Services (PADHS) (Medicaid) continued collaborations and incrementally added information about the National DPP to quarterly Medicaid MCO meetings.
- 2016: The Pennsylvania legislature mandated that the Joint State Government Commission complete an ongoing study of the public health challenges and financial burden related to increased diabetes rates. The Commission recommended that the General Assembly support mandates related to coverage for diabetes prevention and management programs in the state regulated insurance plan. To learn more about the legislation that mandated this study, see the Pennsylvania example on The Role of the State Legislature in Medicaid Coverage page of the Coverage Toolkit.
- 2017: The PADHS Medical Director committed to a statewide National DPP Medicaid MCO pilot at the Pennsylvania National DPP State Engagement Meeting (this meeting was supported through funding from CDC and technical assistance from NACDD).
- 2017: The PADHS Medical Director committed to a statewide National DPP Medicaid MCO pilot at the Pennsylvania National DPP State Engagement Meeting (this meeting was supported through funding from CDC and technical assistance from NACDD).
- 2018: The two-year Pennsylvania Managed Care Diabetes Prevention Program pilot began.
- 2019: PADHS created a new provider type that allows CDC-recognized organizations to enroll in Medicaid.
- 2020: The Pennsylvania Managed Care Diabetes Prevention Program pilot ended, and the National DPP lifestyle change program was integrated into the HealthChoices agreement between Pennsylvania Medicaid and Pennsylvania Medicaid MCOs as a required program.
Piloting the National DPP Lifestyle Change Program through MCOs
In January 2018, PADHS launched a two-year pilot requiring all MCOs in the state to provide a diabetes prevention offering to their Medicaid enrollees. Because over 93% of Pennsylvania Medicaid beneficiaries are enrolled in managed care, this pilot captured most of the Medicaid population. During the pilot, federal Medicaid matching funds were not claimed for reimbursement of the program. Initially in the pilot, the diabetes prevention offering was not mandated to be delivered through CDC-recognized organizations. However, when Pennsylvania incorporated language in its 2020 managed care contracts, it required MCOs to refer eligible members to CDC-recognized organizations only.
Pennsylvania chose to pursue a pilot initially, rather than requiring coverage of the National DPP lifestyle change program for all Medicaid enrollees, to ensure that enough CDC-recognized organizations were available to deliver the program throughout the state. PADHS created a new provider type for CDC-recognized organizations to enroll in Medicaid, which allows the state to map where CDC-recognized organizations are located.
Adding the National DPP Lifestyle Change Program to Medicaid MCO Contracts
In 2020, the language in the HealthChoices agreement between Pennsylvania Medicaid and Pennsylvania Medicaid MCOs was updated to include the National DPP lifestyle change program as a required program. The contract language states, “Include and refer members who are identified as pre-diabetic to programs that addresses prevention of diabetes mellitus. The programs must be recognized by the Centers for Disease Control [and Prevention] (CDC) or be enrolled in the Medicare program as a Medicare Diabetes Prevention Program.” Pennsylvania Medicaid MCOs are required to include and refer members who are identified as having prediabetes and other risk factors.
Technical Assistance Webinars
PADOH and PADHS implemented a webinar in 2020, with an accompanying FAQ document, for National DPP partners, including CDC-recognized organizations, MCOs, and Lifestyle Coaches, to share information about the National DPP lifestyle change program. This interactive webinar covered how CDC-recognized organizations can enroll in the Pennsylvania Medicaid program, contracting between MCOs and CDC-recognized organizations, network adequacy, and considerations for successfully recruiting, enrolling, and retaining Medicaid beneficiaries. Webinars such as these provide a way for partners to interact and to disseminate information on the program; they also serve as a way to engage key partners and build new or strengthen existing relationships between the individuals and organizations who implement the program.
Implementing Coverage
Benefit Breakdown
| Delivery Methods | CDC-recognized organizations offering the National DPP lifestyle change program through in-person, online, distance learning, and combination delivery options can enroll in Medicaid. |
| Participant Eligibility | Medicaid beneficiaries may need to have a referral from a physician to be eligible for the National DPP lifestyle change program. Each MCO determines whether a referral is required. |
| Lifestyle Coaches | A Lifestyle Coach may be a licensed health professional, a community health worker, or an unlicensed individual trained in the CDC curriculum. |
| Eligible Providers | Pennsylvania has created a new provider type that allows CDC-recognized organizations to be enrolled in Medicaid. The CDC-recognized organization must have preliminary or full recognition, or be a Medicare Diabetes Prevention Program (MDPP) Supplier. |
| Program Parameters | National DPP lifestyle change program services are provided over a 12-month period. They are not limited to once in a lifetime for Medicaid beneficiaries. |
| Reimbursement, Coding, and Billing | MCOs receive a per-member-per-month payment from Pennsylvania Medicaid; however, Pennsylvania Medicaid is not determining reimbursement rates for the National DPP lifestyle change program. Instead, because the MCOs are paying the Medicaid enrolled CDC-recognized organizations, the MCOs are determining the reimbursement rate for this program. |
Program Features Unique to Pennsylvania
Creating a New Provider Type
In 2019, PADHS created a new provider type that allows CDC-recognized organizations to enroll in Medicaid. Pennsylvania’s MCOs must contract with Medicaid-enrolled CDC-recognized organizations. Pennsylvania released a bulletin for CDC-recognized organizations that explains how to enroll and includes federal resources, enrollment procedures, and requirements. To learn more about why a state would create a new provider type, visit the Determining the Medicaid Enrolled Provider Type page of the Coverage Toolkit.
Lessons Learned
Pilot Before Required Coverage
To set the National DPP lifestyle change program up for success in Pennsylvania, the state chose to first pursue a pilot within the Medicaid managed care program. Pennsylvania’s pilot of the National DPP lifestyle change program had several advantages. First, it allowed Medicaid to evaluate the network adequacy of its CDC-recognized organizations. Second, by initially requiring the MCOs to provide diabetes prevention services—but not mandating that those services be delivered through CDC-recognized organizations—PADHS allowed the MCOs time to prepare. Finally, it allowed PADHS to provide support to CDC-recognized organizations. For example, shortly after PADHS created the new provider type, Pennsylvania asked CDC-recognized organizations in a survey about their knowledge of the new provider type, the challenges with enrolling in Medicaid, and their technical assistance needs. The technical assistance webinar content addresses the needs identified in the survey findings.
Additional Resources
Pennsylvania CDC-recognized Organization Enrollment in Medicaid Bulletin
Pennsylvania Technical Assistance Webinar, October 2020
Pennsylvania Technical Assistance FAQ, October 2020
PADHS: Electronic Portal Instructions for Enrollment of Diabetes Prevention Program (DPP) Providers









