Medicaid → Implementation→ National DPP Lifestyle Change Program Delivery Options
National DPP Lifestyle Change Program Delivery Options
When covering the National Diabetes Prevention Program (National DPP) lifestyle change program, state Medicaid agencies and Medicaid managed care organizations (MCOs) have several options for program delivery. These options include contracting with CDC-recognized organizations that offer the program:
- In-person. Yearlong lifestyle change program delivered 100% in person for all participants by trained Lifestyle Coaches; meaning, participants are physically present in a classroom or classroom-like setting. Lifestyle Coaches may supplement in-person sessions with handouts, emails, or reminder texts. Organizations that conduct make-up sessions online, via some other virtual modality, or over the phone are still considered to be delivering the program in-person. Note: some health systems that are Medicaid enrolled providers may already offer the program.
- Online. Yearlong lifestyle change program delivered 100% online for all participants; meaning, participants log into course sessions via a computer, laptop, tablet, or smart phone. Participants also must interact with Lifestyle Coaches at various times and by various communication methods, including online classes, emails, phone calls, or texts.
- Distance Learning. Yearlong lifestyle change program delivered 100% by trained Lifestyle Coaches via remote classroom or telehealth (i.e., conference call or Skype) where the Lifestyle Coach is present in one location and participants are calling or video-conferencing in from another location.
- Combination. Yearlong lifestyle change program delivered as a combination of any of the previously defined delivery modes (1 – 3 above) by trained Lifestyle Coaches.
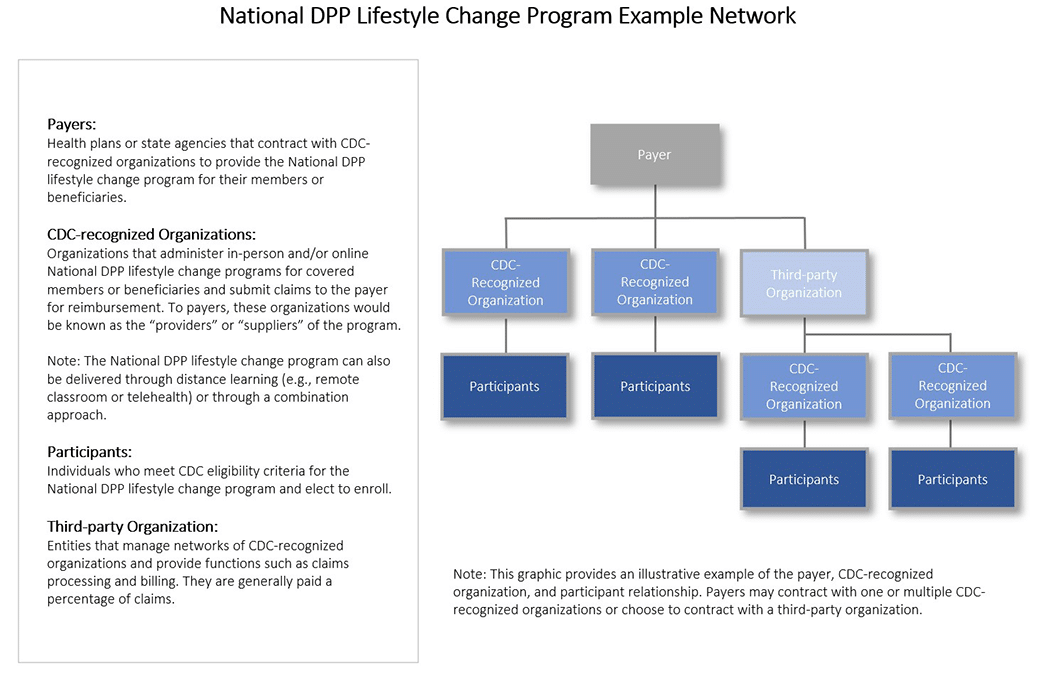
- (For MCOs) – Contract with a third-party organization, such as an umbrella hub arrangement (UHA), to create a network of CDC-recognized organizations that provide the National DPP lifestyle change program.
- (For MCOs) – Seek CDC recognition and offer the program themselves. Organizations interested in offering the program can use the American Medical Association’s National DPP Lifestyle Change Program Budget Considerations Tool to estimate the cost implications of offering the program.
Click here for a list of CDC-recognized organizations in your state. For a map comparing the availability of National DPP lifestyle change program classes from organizations with full or pending CDC-recognition status, click here.
The CDC developed the Find a Program tool and the Find a Program fact sheets as resources for program participants and CDC-recognized organizations. The Find a Program tool provides new and returning National DPP participants an on-demand list of available lifestyle change programs offered in a specified area. The Find a Program fact sheet for CDC-recognized organizations provides information to navigate the Diabetes Prevention Recognition Program (DPRP) Data Submission Portal to update their organization’s public class information.
When determining what types of CDC-recognized organizations to include in their network, state Medicaid agencies and MCOs should consider Medicaid rules and authorities, current delivery system structures, network adequacy, credentialing, other contracting standards and the needs of their Medicaid population.
Provider Status and Other Medicaid Program Considerations
One issue for Medicaid agencies to consider is the process for CDC-recognized organizations to obtain Medicaid provider status. To learn more about this process, please visit the Determining the Medicaid Enrolled Provider Type page.
For CDC-recognized organizations to be able to bill the Medicaid agency for services provided, they must be a Medicaid enrolled provider. While the National DPP lifestyle change program relies on the use of both health professionals and non-licensed personnel to serve as Lifestyle Coaches, non-licensed personnel typically fall outside of a state’s clinical licensure system. In these cases, state Medicaid agencies may need to create a new provider type in order for CDC-recognized organizations to be reimbursed for services provided to Medicaid beneficiaries. Sometimes a state can leverage a provider type that is already covered by the state Medicaid program to serve as a Lifestyle Coach, such as a community health worker (CHW). For more information about using an existing provider type and creating a new provider type, visit the Determining the Medicaid Enrolled Provider Type page of the Coverage Toolkit.
A state will need to create a new provider type to allow CDC-recognized organizations to enroll in Medicaid even if it is only offering the National DPP lifestyle change program through managed care. The current Medicaid managed care rule requires all MCO-contracted providers to enroll as Medicaid providers, even if they do not deliver services to Medicaid fee-for-service beneficiaries. Maryland and Pennsylvania are examples of states that created a new provider type for CDC-recognized organizations participating in the states’ Medicaid managed care programs.
As Medicaid enrolled providers, CDC-recognized organizations will need to comply with Medicaid program integrity rules such as confidentiality, screening, and disclosure standards. While these organizations have experience with meeting CDC’s DPRP standards, many of these organizations are community-based, will be new to the Medicaid program, and may not understand Medicaid program standards and requirements. As a result, state Medicaid agencies may need to leverage existing internal and external resources (e.g., state health departments, national partners, etc.) to conduct extra trainings to help these organizations comply with Medicaid safety, quality, and provider enrollment requirements.
National DPP Lifestyle Change Program Example
CDC-Recognized Organizations Offering In-Person Lifestyle Change Programs
In-person National DPP lifestyle change programs are offered by a variety of organizations, including but not limited to hospitals, health plans, YMCAs, diabetes self-management education and support (DSMES) programs, pharmacies, Cooperative Extension Centers, local health departments, community-based organizations, and faith-based organizations.
Note: Some health systems that are Medicaid enrolled providers may already offer the program. Medicaid agencies should review the list of CDC-recognized organizations in their state to determine if potential partnerships already exist.
Click here for a list of CDC-recognized organizations in your state.
Working with Community-Based Organizations
Partnering with community-based organizations to provide the National DPP lifestyle change program has the potential to activate individuals to be more engaged in their care and enable providers to better address clinical issues by leveraging the expertise and skills that exist in the human services industry.
The Partnership for Healthy Outcomes studied over 200 community partnerships between community-based organizations and health care organizations. The resulting report indicated the following core components of community partnerships:
- Develop unified goals
- Determine a common understanding of where on the integration spectrum the partnership lies: communicating, coordinating, collaborating, or integrating.
- Create a formal agreement
- Establish a funding model
- Maintain a level of data sharing
- Cultivate mutual trust
Challenges
Some of the greatest challenges that may exist within partnerships with community-based organizations, as indicated by the Partnership for Healthy Outcomes and the Illinois Public Health Institute, are:
- program funding and sustainability,
- data sharing and submission, and
- inexperience with health industry processes.
Many community partnerships found that covering their full, ongoing costs is a primary challenge. Even with insurance reimbursement, many must still subsidize costs through other funding sources, such as grants. Calculating and documenting true program costs is one key to informing return-on-investment calculations, developing a sustainable funding model, and building trust between partners.
Technology challenges exist for both health/insurance organizations and community-based organizations when working together. For instance, many claims systems are not configured to receive claims-based codes from non-traditional providers. This limits the payment and process models that may be used when implementing the National DPP with community-based organizations. In addition, some community-based organizations may have limited technological capability to share various levels of data, to abide by the Health Insurance Portability and Accountability Act (HIPAA), or to efficiently assess results. Health care organizations, including payers, may consider providing data and analytical support to mitigate some of these challenges or contract with a third-party organization that can manage and provide some of these needed data functions for the community-based organizations.
Most community-based organizations have very little experience with many of the processes used in the health care industry and may need some guidance in carrying them out. Some of these processes may include enrolling as a Medicaid provider, submitting claims or invoices, negotiating contracts with payers, understanding data security protocols, or receiving referrals from and working with providers.
Partnership Assessment
The Partnership for Healthy Outcomes also developed a Partnership Assessment Tool (accessed here) to help you identify strengths, gaps, challenges, and opportunities and help guide your conversations to ensure a strong and effective partnership.
CDC-Recognized Organizations Offering Online or Distance Learning Lifestyle Change Programs
Several organizations have experience providing the National DPP lifestyle change program online or via a distance learning platform and, like in-person programs, understand program requirements, quality standards, and data reporting. For example, in Montana, Medicaid reimburses for the National DPP lifestyle change program at the same rate for both in-person visits and those is offered via live interactive audio and visual teleconferencing using a secure connection.
Offering the National DPP lifestyle change program online or through distance learning may increase access to the program, particularly in rural areas. Additionally, a recent study found that participants who received the National DPP lifestyle change program through telehealth videoconferencing (distance learning) had similar rates of participation and achieved similar weight loss as participants who attended the program in-person. It is important to note, however, that CDC-recognized organizations that provide the program online often use a smart-phone or tablet-based platform, which may not work well for Medicaid beneficiaries who have limited or no access to the internet. That said, smart phone use is broadening among Medicaid beneficiaries.
As with in-person organizations, online or distance learning CDC-recognized organizations need to comply with HIPAA and Medicaid rules and regulations. Specifically, they will need to comply with Medicaid rules and regulations regarding the remote provision of services.
Click here for a list of online, or combination in-person/online CDC-recognized organizations in your state. Click here for a list of evidence on the effectiveness of in-person and online delivery of the National DPP lifestyle change programs.
CDC has developed a Virtual Recruitment Toolkit in response to the COVID-19 pandemic. Virtual recruitment has become increasingly important as a result of the public health emergency and as digital technology and the internet have become universal tools to communicate with people. The toolkit offers guidance on how to recruitment program participants in a virtual or remote environment. Concurrently, CDC developed a published Guidance for Virtual Delivery of the National DPP, available here.
Seeking CDC Recognition
Medicaid Agencies
State Medicaid agencies can encourage Medicaid managed care organizations (MCOs) or other organizations they want to work with to apply for CDC recognition and meet the DPRP standards.
To ensure high quality and impact, CDC’s DPRP plays a critical role in assuring that organizations can effectively deliver the evidence-based lifestyle change program with quality and fidelity. For more information, see the Standards for CDC Recognition.
MCOs
MCOs can become CDC-recognized themselves, which may simplify network development and contracting.
Organizations can apply for CDC recognition if they meet CDC’s Diabetes Prevention Recognition Program (DPRP) standards. To ensure high quality and impact, CDC’s DPRP plays a critical role in assuring that organizations can effectively deliver the evidence-based lifestyle change program with quality and fidelity. CDC only recognizes programs that meet standards such as using a CDC-approved curriculum, which helps participants meet intensity and duration requirements to achieve the 5‒7% weight loss goal.
The DPRP, along with some state and local public health departments, also provides technical assistance to organizations to help them achieve and maintain program recognition.
- For more information on standards for CDC recognition, click here.
- For the DPRP application form, click here.
CDC-recognized organizations are regularly monitored and evaluated. They must track results and send data to CDC to show that they are meeting the recognition standards. CDC reviews these data and provides feedback to the program on their recognition status in addition to help in troubleshooting potential problems that could be keeping the organization from achieving recognition.
Third-Party Organizations
Some MCOs may choose to work with a third-party organization to assist with program delivery. Third-party organizations can manage networks of CDC-recognized organizations and can provide functions such as claims processing and billing. They may be paid a percentage of claims. Third-party organizations acting in this capacity have been called a number of terms, including UHA, third-party administrator (TPA), provider integrator, or management service organization (MSO), all of which connect organizations with health care payment systems to pursue sustainable reimbursement for the National DPP lifestyle change program.









