Umbrella Hub Arrangements → Umbrella Hub Arrangement Overview
Umbrella Hub Arrangement Overview
Umbrella hub arrangements (UHAs) connect community-based organizations (CBOs) with health care payment systems to pursue sustainable reimbursement for the National Diabetes Prevention Program (National DPP) lifestyle change program. CBO is a broad term for community-based organizations delivering the National DPP lifestyle change program and could include, but is not limited to, Federally Qualified Health Centers (FQHCs), tribal organizations, Area Agencies on Aging (AAA), pharmacies, local health departments, faith-based organizations, extension programs, small social service agencies, and/or other small health care providers. Throughout the Coverage Toolkit, CBOs delivering the National DPP lifestyle change program and participating in a UHA will be referred to as subsidiary organizations.
Each UHA is administered by an umbrella hub organization (UHO, or occasionally, “hub”), which is the lead organization in the arrangement. Some examples of organization types currently serving as UHOs include:
- Primary care associations
- Universities
- Community-based organizations
- Non-profit organizations or corporations
- Area Agencies on Aging
- Foundations
- National organizations (e.g., recipients of CDC cooperative agreement grants, pharmacy and provider associations, etc.)
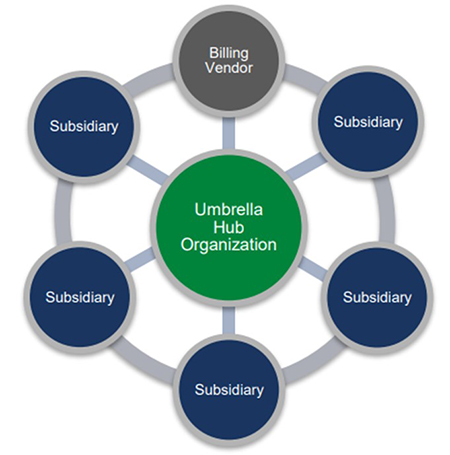
UHA is the overarching term that refers to the entire group, inclusive of the UHO, subsidiary organizations, and the billing platform used to submit claims. The UHA may also operate with the support of external partners, including but not limited to, referral networks, health plans, and state health departments. This page provides guidance for organizations interested in becoming a UHO or supporting the operation of a UHA.
This page is divided into six sections:
- What is an Umbrella Hub Arrangement?
- Why Create an Umbrella Hub Arrangement?
- Umbrella Hub Basics Webinar
- The Umbrella Hub Demonstration
- Building Blocks to Operationalize a UHA
- UHA Resource Guide and UHA Resources at a Glance
For guidance on becoming a UHO and to access the application, please visit the National DPP Umbrella Hub Arrangements Guidance and Application page on CDC’s National DPP Customer Service Center.
What is an Umbrella Hub Arrangement?
UHAs are a business approach to connect CBOs with health care payment systems for delivery of the National DPP lifestyle change program, a year-long, evidence-based program to prevent type 2 diabetes.
In a UHA, a UHO serves as the sponsoring organization for a group of subsidiary organizations. These CDC-recognized subsidiary organizations are organizations that deliver the National DPP lifestyle change program and have met the quality standards set by CDC’s Diabetes Prevention Recognition Program (DPRP). Just as a hub connects all the tire components in a wheel to the rest of the vehicle, the UHO connects a group of CDC-recognized organizations to health care payment systems, as depicted in the figure below.
For a one-page overview on UHAs and a guide to UHA terminology, please see the UHA One-Pager and the UHA Terminology Guide.
The UHA Frequently Asked Questions (FAQ) document addresses common questions about the structure, roles and responsibilities, and reimbursement considerations of the UHA. It is intended to support state health departments, organizations, and partners considering, supporting, or directly involved in a UHA.
Why Create an Umbrella Hub Arrangement?
UHAs provide administrative support to subsidiary organizations in accessing health care reimbursement, which is the primary benefit of participating in this arrangement and a key factor in achieving program sustainability. Additional benefits of UHAs include the following (also referred to as the “value propositions” and “key assets and processes” of the UHA on the Business Model for Umbrella Hub Arrangements page):
Operate as One MDPP Supplier
Operate as one Medicare Diabetes Prevention Program (MDPP) supplier: In a UHA, the UHO is the MDPP enrolled supplier and subsidiary organizations do not separately enroll as MDPP suppliers. The subsidiary organizations participating in the UHA access Medicare reimbursement through the UHO’s MDPP supplier status.
Pursue Sustainability
Pursue sustainability and achieve economies of scale: Participation in a UHA can help the subsidiary organizations work together to pursue sustainability and achieve economies of scale. In the context of a UHA, sustainability refers to subsidiary organizations receiving long-term reliable reimbursement from public and private payers rather than short-term funding from sources such as federal grants. Benefits of scale and network adequacy occurs as more subsidiary organizations join the UHA. This collective impact makes the network more attractive to health care payers.
Streamline Support
Streamline billing, claims, and administrative support: Many CDC-recognized organizations face challenges in successfully billing Medicare and other health care payers to receive reimbursement. A key element of a UHA is a single billing and claims submission platform used by all subsidiary organizations. For example, the billing and claims platform can either be an existing in-house platform used by the UHO that all subsidiary organizations can access, or it can be a contracted third-party platform.
Share CDC Recognition
Share CDC-recognition status: To join a UHA, each subsidiary organization must have pending, preliminary, or full recognition; however, while participating in the arrangement, all subsidiary organizations assume the recognition status of the UHO. This shared recognition status has several benefits, including enabling subsidiary organizations that entered the UHA with pending recognition to access Medicare reimbursement through the UHO’s collective recognition status. Additionally, once a UHA achieves full plus recognition, it will be allowed to maintain that status indefinitely as long as it continues to submit data.
Promote Health Equity
Promote health equity: UHAs support partners in activating and advancing goals related to health equity. The UHA provides a mechanism for the UHO, subsidiary organizations, convening partners, referral sources, and community-based entities to screen and address unmet health-related social needs (HRSN) that contribute to health disparities. Conversations about how UHAs can support health equity may begin with a clear understanding of the terms related to health equity. Definitions related to health equity are outlined in the following table. Additional information and resources are available on the Defining Health Equity page of the Coverage Toolkit.
- Health Equity: the state in which everyone has a fair and just opportunity to attain their highest level of health.
- Health Disparities: a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage.
- Social Determinants of Health (SDOH): the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality of life outcomes and risks.
- Health-Related Social Needs (HRSN): immediate individual or family needs impacted by social and economic conditions (i.e., housing insecurity, food insecurity, or lack of reliable transportation).
UHA Role in Understanding SDOH and Addressing HRSN
Individuals are impacted by SDOH in different ways. Understanding how individuals are affected by SDOH and addressing their HRSN can reduce health disparities and improve an individual’s health outcomes. The yearlong National DPP lifestyle change program provides multiple touchpoints with participants that can be used to provide resources to address HRSN. For information on how the National DPP lifestyle change program can be leveraged to improve health equity, visit the Addressing HRSN Through the National DPP Lifestyle Change Program page of the Coverage Toolkit.
The CDC SDOH framework, in the figure below, illustrates the six pillars of improving health equity through understanding and addressing HRSN. These pillars include policy and law, data and surveillance, evaluation and evidence building, partnerships and collaboration, community engagement, and infrastructure and capacity. The UHA can support health equity by addressing each of these pillars.
Hover over the green plus signs ![]() on the image below to learn more.
on the image below to learn more.

UHOs and conveners are encouraged to serve priority populations, identify resources, and develop goals which incorporate health equity principles when establishing a UHA. Having these conversations early in the UHA planning process is vital to the sustainability of the UHA. This process may include assessing regional prediabetes rates or HRSN data to define priority populations, educating partners on social and economic history of the community they are serving, understanding payment mechanisms in the state to inform partnerships, or identifying organizations in the region that currently offer the National DPP lifestyle change program or other evidence-based programs. Consideration of these elements early in the planning process can help to streamline goals and expectations during the operationalization of the UHA. For more guidance on this topic, please see the Landscape Analysis for UHAs. Additional guidance on how the UHA may support health equity goals can be found on the Business Model for Umbrella Hub Arrangements, Sustaining Umbrella Hub Arrangements, and Health Equity and the National DPP pages of the Coverage Toolkit.
Additionally, organizations interested in serving as the UHO are encouraged to become familiar with the purpose and requirements for UHOs and to review the UHA-related sections of the CDC DPRP Guidance Document. Certain actions required to set up a UHA must be completed in order; for example, subsidiaries must be identified before an organization can apply to become a UHO. Other actions may happen concurrently or in a different order than outlined by the DPRP Guidance Document. UHAs are encouraged to consider sustainability throughout the process. For additional information on sustainability, please see the Sustaining Umbrella Hub Arrangements page of the Coverage Toolkit.
CDC is currently accepting applications for UHAs. For more information on becoming a subsidiary in a UHA, please contact your state health department. For additional details on establishing a UHA, please see the UHO Checklist, which is intended to help UHOs develop a work plan for completion of the administrative activities. The UHO Capacity Assessment was developed to gauge an organization’s interest, capacity, ability, and willingness to serve as a UHO, and the Tips for Identifying Potential UHOs document can be used to identify whether an organization may be a candidate to serve as a UHO. If you are interested in a UHA but are unsure of what role you might play or your capacity to participate in a UHA, please see the document titled UHA Questionnaire for CDC-Recognized Organizations, which assesses an organization’s familiarity and interest in the UHA model.
Umbrella Hub Basics Webinar
The webinar below introduces viewers to UHAs and provides basic information about the who, what, and why of UHAs. Information is provided on the role of state health departments in supporting the development of UHAs.
The chapter descriptions below map to the blue dots along the bottom of the video window. Please note webinar loading times may vary depending on the user.
- “Opening Comments” (4:32) describes how and why the concept of UHAs emerged, and at a high level, some of the lessons learned, challenges, and opportunities for those considering forming a UHA.
- “Why are UHAs Needed” (15:20) provides information about the benefits of a UHA, readiness attributes of UHA partners, and highlights the Umbrella Hub Demonstration, funded by CDC.
- “Who is Involved?” (21:50) gives an overview of the key players in a UHA.
- “What is an Umbrella Hub Arrangement?” (24:34) shares the purpose of a UHA and shares an illustration of a hub and spoke model for the UHA.
- “How Does a UHA Work?” (26:52) explains the legal agreements and contracts that bind UHAs together and gives an overview of the reimbursement process.
- “How Can It Be Sustained?” (39:30) reviews a UHO business model, and a phased approach to achieving financial sustainability. This chapter provides considerations on ways to retain and increase subsidiaries and participants.
- “UHA Resources” (58:54) describes a UHA learning lab, gives examples of how state health departments and others can support the development of UHAs, and provides UHA resources.
- “Questions and Answers” (1:08:53)
The Umbrella Hub Demonstration
The overall purpose of the Umbrella Hub Demonstration (Demonstration) is to connect CBOs delivering the National DPP lifestyle change programs to health care payment systems. In 2019, CDC began to fund three organizations to operationalize UHAs through the Demonstration. One goal of the Demonstration is to share learnings from operationalizing a UHA, particularly around submitting claims and receiving reimbursement from the Centers for Medicare and Medicaid Services (CMS) on behalf of subsidiary organizations delivering the Medicare Diabetes Prevention Program (MDPP). UHOs may also submit claims and reimbursement from other payers for the National DPP lifestyle change program. Hawaii Primary Care Association (HPCA), Health Promotion Council of Southeastern Pennsylvania (HPC), and Marshall University were selected as the three initial Demonstration UHOs. Additionally, a technology vendor, Welld Health, was selected as the billing and claims vendor to support the UHOs in data aggregation and claims submission for reimbursement. In 2023, three additional UHOs, The Association of Asian Pacific Community Health Organizations (AAPCHO), American Pharmacists Association (APhA) Foundation, and the YMCA of Metropolitan Milwaukee were added to the Demonstration. The organizations participating in the Demonstration are some of the first organizations to become UHOs and share learnings on operationalizing a UHA. For information on additional UHOs that have been approved by CDC, please visit the CDC DPRP Registry website. Other organizations have started their UHO journey through the CDC-funded Medicaid Beneficiary Enrollment Project, designed to increase coverage of and access to the National DPP lifestyle change program for individuals enrolled in Medicaid.
The shared learnings from the Demonstration and other UHA-related work have helped to inform the considerations and resources found on these Umbrella Hub Arrangement pages. The Umbrella Hub Demonstration is ongoing, and additional learnings and resources will be added to the Coverage Toolkit as they become available. To learn more about the shared successes and challenges faced by the original Demonstration UHOs, as well as general guidance on establishing a UHO, please see the document titled Learnings from the Umbrella Hub Demonstration. This document captures the learnings of the three original organizations that participated in the Demonstration and serves as a reference for organizations interested in becoming a UHO or supporting the operation of a UHA. Additionally, learnings from Demonstration and other UHAs were presented during the Umbrella Hub Arrangement Summit 2022, a 1.5-day convening in which emerging UHAs gathered for peer-to-peer discussion and sharing of successful strategies to operationalize a UHA.
For ease of reference, the Learnings from the Umbrella Hub Demonstration document has been divided into four separate documents:
- Learnings from the Umbrella Hub Demonstration – Overview
- Learnings from the Umbrella Hub Demonstration – Business Model and Contracts
- Learnings from the Umbrella Hub Demonstration – Reimbursement
- Learnings from the Umbrella Hub Demonstration – Sustainability
These documents correlate with the content on the six UHA pages on the Coverage Toolkit.
Learnings from the Umbrella Hub Demonstration specifically related to this Coverage Toolkit page are in the document titled, Learnings from the Umbrella Hub Demonstration – Overview.
Umbrella Hub Organizations of the Umbrella Hub Demonstration

HPCA is a statewide network of 15 community health centers (CHCs), the term used for FQHCs in Hawaii) that provides technical assistance and advocacy support to improve the health of communities in need. HPCA supports health centers that provide the National DPP lifestyle change program in many ways. This includes training to support lifestyle coaches, direct technical assistance, data support, educational materials, quality improvement projects, and reimbursement support.

HPC is a Pennsylvania-based non-profit whose mission is to promote health and prevent and manage chronic disease among vulnerable populations through community-based outreach, education, and advocacy. HPC fulfills this mission in three primary ways: direct services and programming; training, technical assistance, and capacity building; and policy and systems change. In partnership with the Pennsylvania Department of Health, HPC has been building capacity of the National DPP in Pennsylvania since 2014.

Marshall University is based in West Virginia and offers a variety of evidence-based programs across Appalachia and eight states. Through the Appalachian Diabetes Control and Translation project Marshall University prevents and controls diabetes by developing and providing direct technical assistance to coalitions delivering the National DPP lifestyle change program in under-resourced and rural counties throughout the Appalachian region.
AAPCHO was formed to create a national voice to advocate for the unique and diverse health needs of Asian American and Native Hawaiian/Pacific Islander communities and the community health providers. This includes collaborating with community members and trusted subject matter experts to adapt the National DPP lifestyle change program curriculum and training to incorporate health beliefs and cultural approaches specific to the Native Hawaiian and Pacific Islander communities they serve.

The APhA Foundation is an affiliate of APhA and serves as a source of research demonstrating how pharmacists can improve health care. The mission of the APhA Foundation is to improve health by inspiring philanthropy, research, and innovation that advances pharmacists’ patient care services, including care for and prevention of chronic conditions such as diabetes through the National DPP lifestyle change program.

The YMCA of Metropolitan Milwaukee has been a part of the lives of the greater Milwaukee area’s kids and families since 1858. The YMCA of Metropolitan Milwaukee offers a variety of in-person and virtual evidence-based programs like the National DPP lifestyle change program to support residents along the health and well-being journey, led by caring staff who provide participants with the knowledge, skills, and support to live a happy and healthy life.
Building Blocks to Operationalize a UHA
The UHO performs a wide variety of functions that are critical to the UHA’s success. Below are seven building blocks for the UHO to operationalize the UHA: (1) Align the Core Mission and Vision of the UHA, (2) Develop a Workplan to Operationalize the UHA, (3) Develop or Contract with a Billing and Claims Platform, (4) Evaluate Business Acumen Required to Operate a UHA, (5) Create a Financial Sustainability Plan, (6) Establish UHA Communication and Coordination Protocols, and (7) Identify and Recruit Subsidiaries. Each element is followed by related insights from the Demonstration UHOs.
1. Align Mission and Vision
Align the Core Mission and Vision of the UHA
The UHA aims to increase the capacity of organizations to deliver the National DPP lifestyle change program. Core mission alignment between the UHO and subsidiaries is essential to the foundation of the UHA and should be addressed prior to development of the UHA. Mission alignment can streamline development of the UHA, build trust between UHA partners, and strengthen the organizational capacity to provide a unified direction for all involved. For example, communicating a broader vision for the UHA—such as lowering the incidence of type 2 diabetes in a specific community—can help strengthen organizational commitment to operationalize the UHA.

- Focus on the UHA’s mission: Keeping overall goals in mind (e.g., supporting subsidiary organizations in their efforts to deliver the National DPP lifestyle change program to prevent type 2 diabetes) helped the Demonstration UHOs navigate the challenges of starting a new business arrangement. Documenting goals and mission statements helped the organizations define shared objectives. To learn how Demonstration UHOs used charters to define the UHA’s mission, see the charters section of the Business Model for Umbrella Hub Arrangements page and refer to sample charters (charter example 1 and charter example 2) developed by UHOs.
2. Develop a Workplan
Develop a Workplan to Operationalize the UHA
Potential UHOs are encouraged to inventory their internal resources such as staffing, administrative capacity, and financial status, and compare those resources to the resources necessary to operationalize a UHA. Additionally, UHO staff should have a detailed understanding of the National DPP lifestyle change program. This will facilitate the UHO’s ability to operationalize the UHA and provide support for subsidiary organizations. The UHA Project Planning Template can be used to assist organizations with the planning phases of a UHA. The template can serve as a guide for organizing thoughts and tracking efforts related to UHA planning and can be adapted to fit unique organizational needs or goals. While the UHA Project Planning Template was originally developed to assist UHAs interested in enrolling in Medicaid and/or contracting with managed care organizations, content can be adjusted to fit organizations interested in prioritizing Medicare Diabetes Prevention Program (MDPP) enrollment and/or commercial payer partnerships.
Additionally, the UHA Modifiable Slide Deck can be utilized to guide organizations through efforts to implement sustainable UHA partnerships and processes. It is recommended that organizations serving as the UHO or participating in a convener role modify the deck as needed and use it in initial conversations with partners to educate them and/or to help make the case for participation in a UHA. You can learn more about the UHA Modifiable Slide Deck and how to use it, by reading through the accompanying UHA Modifiable Slide Deck – Introduction.

- Understand the time commitments required to operationalize the UHA: Demonstration UHOs found the start-up phase took between 6-12 months. This included gathering the necessary documents and requirements for the MDPP application, meeting with subsidiary organizations to explain the details of the UHA, determining and explaining how the UHO would distribute claims payments to subsidiary organizations, and meeting with senior leadership to discuss decisions about the UHA. Information on start-up costs associated with these activities are available on the Business Model for Umbrella Hub Arrangements page.
- Develop a work plan: Demonstration UHOs found that a work plan helped identify the key tasks, timeline, staff, and resources needed to operationalize the UHA. A detailed work plan can help UHOs stay on track with actions such as recruiting subsidiary organizations, completing CDC’s UHA application, executing contracts with subsidiary organizations, enrolling in Medicare, adding subsidiary organizations to a Medicare enrollment, and establishing accounting processes for claims reimbursement distribution. The UHA Project Planning Template can be used to create a work plan.
3. Establish Billing and Claims
Develop or Contract with a Billing and Claims Platform
A function of a UHA is to submit claims to public (Medicare and Medicaid) and commercial health care payers on behalf of the subsidiary organizations. It is recommended that organizations seeking to serve as a UHO assess their willingness and capacity to work with a billing and claims vendor or determine whether they have an in-house platform to submit claims that all subsidiary organizations could easily access and use. The billing and claims vendor may be able to create multiple efficiencies for subsidiary organizations including streamlining the referral and enrollment process, simplifying participant data entry, recording attendance and weight loss milestones, and submitting data to CDC and claims to health care payers.
When selecting a billing vendor, UHOs are encouraged to consider their budget, personnel, resources, and the cost of the billing platform relative to the payer reimbursement rate and any administrative fees the UHO may charge subsidiary organizations. CDC’s UHA guidance document, found on the National DPP UHA Guidance and Application page on their National DPP Customer Service Center, states that start-up costs and/or ongoing operational costs associated with the use of billing platform or vendor are handled between the UHO and the subsidiary organizations and CDC will not review these business arrangements. However, CDC has developed guidance for CDC-funded recipients on purchasing billing and delivery platforms, available here.

- Build a strong and lasting relationship with a billing vendor: The UHOs that participated in the Demonstration contracted with a vendor to submit claims. Demonstration UHOs and their billing vendor, Welld Health, fostered a strong working relationship. Welld Health has provided technical assistance to the Demonstration UHOs as they operationalize and continues to provide ongoing trainings, maintenance, and payer updates for the Demonstration UHOs.
- Schedule training sessions with subsidiary organizations: Demonstration UHOs scheduled training sessions for subsidiary organizations to help them feel comfortable using the platform to submit claims and to understand the extent of its capabilities.
- Define and communicate the roles, responsibilities, and timelines for the UHO, the subsidiary organizations, and the billing platform: UHOs should educate subsidiary organizations on the roles and required timelines for data entry in the billing platform. Claims denied because of inaccuracies can be costly and time consuming, so it is incumbent on the UHO and subsidiary organizations to work together to ensure submitted claims are accurate and on time.
4. Evaluate Business Acumen
Evaluate the Business Acumen Required to Operate a UHA
The UHA relies on the UHO to handle reimbursements and make business related decisions for the UHA. It is recommended that potential UHOs assess their readiness to engage in all business and financial requirements associated with UHA participation. For additional resources to evaluate an organization’s capacity to serve as a UHO, please reference the UHO Capacity Assessment and Tips for Identifying Potential UHOs tools.

- Determine if the UHO has sufficient infrastructure to handle reimbursements: UHOs are tasked with receiving reimbursement payments from CMS and other health care payers and distributing them to subsidiary organizations. Consider whether the UHO has the experience or adequate resources to handle reimbursement payments. For example, one Demonstration UHO had concerns with directly receiving claims reimbursements and then redistributing the reimbursements to their subsidiary organizations who provided the services. It took several conversations to resolve these concerns and to formulate a plan on how to accomplish these tasks.
- Develop a business model: Demonstration UHOs developed business models to support the UHO and the subsidiary organizations. The Business Models encompass four major areas of business categories, each deserving attention. These include how to appeal to customers, how to identify revenue sources, and how to understand costs. To learn more about UHA business models, see the Business Model for Umbrella Hub Arrangements page.
- Inventory data management capabilities: Demonstration UHOs developed data management and storage protocols and implemented security measures to meet Health Insurance Portability and Accountability Act (HIPAA) standards.
5. Create Sustainability Plan
Create a Financial Sustainability Plan
The UHO is responsible for the long-term financial sustainability of the UHA. Per CDC’s UHA guidance, found on the National DPP UHA Guidance and Application page of the National DPP Customer Service Center, UHOs are required to activate an agreement with at least one payer within two years of submitting their UHA application. Because of this, UHOs are encouraged to enroll as a MDPP supplier and in state Medicaid programs (where applicable), and to contract with Medicaid managed care organizations (MCOs), Medicare Advantage (MA) plans, commercial health plans, and self-insured employers. For more information about financial sustainability and potential health care payers, see the Reimbursement for Umbrella Hub Arrangements page. Other factors that contribute to the overall sustainability of the UHA can be found in Sustaining Umbrella Hub Arrangements page.

- Evaluate the organization’s ability to operate as an MDPP supplier: The Demonstration UHOs were not MDPP suppliers prior to becoming UHOs. The process to become a MDPP supplier can take several months and involves dedicated staff time and persistence. Demonstration UHOs experienced some unexpected delays, particularly with their MDPP enrollment application, which contributed to extended timelines and added costs. For more information about becoming a MDPP supplier, see the UHO MDPP Supplier Enrollment Guide.
- Consider additional revenue sources: At least two Demonstration UHOs aspire to have Medicaid MCOs or other commercial health care payers help fund the UHA to minimize what subsidiary organizations must pay to participate in the UHA. These talks with commercial health care payers remain ongoing as of March 2022. To learn more about UHA revenue sources, see the Reimbursement for Umbrella Hub Arrangements page.
6. Establish Protocols
Establish UHA Communication and Coordination Protocols
UHAs involve internal coordination with subsidiary organizations and external coordination with partners, including health care payers, referral partners, state partners, and possibly a billing and claims vendor. Potential UHOs are encouraged to assess their capacity for ongoing communication and coordination with UHA partners. Resources, such as the UHA Modifiable Slide Deck, which has been designed to support such relationship building efforts, can be used to assist UHOs in developing marketing and communication strategies for their UHA. Specifically, it is recommended that organizations serving as the UHO or participating in a convener role modify the deck as needed and use it in initial conversations with partners to educate them and/or to help make the case for participation in a UHA. You can learn more about the UHA Modifiable Slide Deck and how to use it, by reading through the accompanying UHA Modifiable Slide Deck – Introduction.

- Educate partners: As early adopters, Demonstration UHOs educated key partners—such as commercial health care payers, state Medicaid agencies, and their state health departments—on the basic components and purpose of a UHA. As UHAs become more prevalent the need for education should decrease; however, new UHOs are wise to expect the need for some level of education for the key partners in their arrangement.
- Engage in ongoing communication with subsidiary organizations: Demonstration UHOs held regular meetings with the subsidiary organizations and the billing and claims vendor to maintain or establish strong relationships with all UHA participants. Open communication and transparent decision making helped UHA participants understand the goals of the arrangement.
7. Identify Subsidiaries
Identify and Recruit Subsidiaries
The UHA can benefit from economies of scale as the number of subsidiary organizations increases. The following are considerations when onboarding new subsidiary organizations into the UHA.
- Willingness to partner in an innovative program: Potential subsidiary organizations will need to be familiar with the commitments and requirements of participating in a UHA. These may include a willingness to educate partners on the Business Model for Umbrella Hub Arrangements, a willingness to enter into contractual agreements, including business associate agreements (BAAs) and data use agreements, and a willingness to contribute to the UHA’s financial strategy.
- Need for billing and administrative assistance: Assessing the administrative capacity and needs of subsidiary organizations are important factors for subsidiary retention and UHA sustainability. UHOs should develop an understanding of the subsidiary organization’s current billing and administrative needs and the resource commitment that will be required from the UHO to meet these needs.
- Ability to reach priority populations: One goal of the UHA can be to advance equity and access to the National DPP lifestyle change program. UHOs may consider recruiting subsidiary organizations that serve priority populations, have beneficial relationships with health care providers, or that serve a new geographic area.
The Subsidiary Onboarding and Engagement Checklist was developed to help UHOs engage with potential subsidiary organizations, obtain commitment from subsidiary organizations to participate in the UHA, and orient subsidiary organizations to their roles and responsibilities. This checklist outlines the potential workflow between the UHO and subsidiary organizations and is intended to serve as a guide for the onboarding and engagement processes with subsidiary organizations. While the Subsidiary Onboarding and Engagement Checklist provides guidelines and time estimates for the onboarding process, it may not reflect all timelines or steps needed for every UHA. UHOs are encouraged to make adjustments to fit their unique needs.
To assess an organization’s familiarity and interest in joining the UHA as a subsidiary, review the UHA Questionnaire for CDC-Recognized Organizations.

- Understand the value proposition of the UHA and needs of individual subsidiary organizations: While identifying and recruiting subsidiaries, Demonstration UHOs developed the value propositions described above and adapted recruitment strategies to align with individual organizational needs.
- Use the UHO’s network as a starting point: Demonstration UHOs had strong relationships with each of their original subsidiary organizations. These strong relationships allowed for trust between the UHOs and their subsidiary organizations, which was valuable given the novelty of the UHA concept and the unknowns inherent in participating in the Demonstration.
- Maintain consistent outreach and recruitment efforts: The sustainability of the UHA is increased as additional subsidiary organizations join the arrangement. Demonstration UHOs regularly discuss the benefits of UHA participation with potential subsidiary organizations. Demonstration sites also report engaging potential subsidiary organizations during other projects or meetings to maintain communication and build relationships.
- Recognize the reasons a potential subsidiary organization may not want to join the UHA: In addition to understanding and communicating the value proposition of the UHA, knowing the reasons a potential subsidiary organization chooses not to join the UHA can help the UHO target future outreach. For example, Demonstration UHOs found that some potential subsidiary organizations were concerned about the costs of participating in the UHA or already had billing and claims submission capabilities.
- Identify additional ways UHOs can help increase subsidiary organizational capacity: Demonstration UHOs are currently exploring and implementing ways to provide additional support to their subsidiary organizations. This includes training and retention of Lifestyle Coaches and reviewing expectations of Lifestyle Coaches to provide services in a UHA (e.g., obtain an NPI).
UHA Resource Guide and UHA Resources at a Glance
The UHA Resource Guide was developed to assist those interested in or in the process of planning for, developing, or operationalizing a UHA. The UHA Resource Guide includes a comprehensive listing of available UHA resources, including guidance on the use of these resources and suggestion on resource utilization for various stages of UHA development. For a brief 3-page listing of UHA resources, review the UHA Resources at a Glance document. The UHA Resources at a Glance document lists each resource, the purpose of the resource, who should use it, and when it is recommended to be used. For an explanation of various UHA components and topics in addition to a more detailed explanation of UHA resources, review the UHA Resource Guide. Readers may elect to search for specific terms in the UHA Resource Guide and navigate directly to the related section.
Resources for Umbrella Hub Arrangements