Medicaid → Medicaid Coverage → Determining the Medicaid Enrolled Provider Type
Determining the Medicaid Enrolled Provider Type
State Medicaid agencies must determine what provider types can deliver the National Diabetes Prevention Program (National DPP) lifestyle change program, including who or what entities enroll in Medicaid as National DPP providers, and who or what entities bill Medicaid for delivering the services.
Example Medicaid Provider Types for the National DPP Lifestyle Change Program
While Medicaid provider rules vary by state, three examples of how Medicaid provider types are structured for the National DPP lifestyle change program are provided below.
1. The CDC-Recognized Organization is the Medicaid Enrolled Provider
CDC-recognized organizations enroll in Medicaid as National DPP providers and bill Medicaid for the services provided by their lifestyle coaches. Individual lifestyle coaches must be associated with a Medicaid enrolled CDC-recognized organization to provide services to Medicaid beneficiaries, but they are not required to formally enroll in Medicaid as providers. Instead, the CDC-recognized organization attests that its lifestyle coaches are in compliance with the CDC Diabetes Prevention Recognition Program’s (DPRP) rules regarding training and other program requirements. The CDC-recognized organization’s National Provider Identifier (NPI) is used for billing and reimbursement purposes. This type of structure works well with the National DPP lifestyle change program given that CDC does not require certification or credentialing for lifestyle coaches. As such, a lifestyle coach is typically not a provider type that is currently recognized by state Medicaid agencies as billing or rendering providers.
Some states may require that individual lifestyle coaches attain an NPI for tracking purposes (like the Medicare DPP, MDPP) and others may not. For example, it is not required by Maryland Medicaid that lifestyle coaches obtain an individual NPI (although it is recommended). Alternatively, California does requires lifestyle coaches to have and maintain an NPI.
2. There are Different Billing and Rendering Providers
Some states may choose to utilize different billing and rendering providers to support National DPP lifestyle change program delivery. Billing providers are reimbursed by Medicaid and rendering providers are typically licensed, credentialed, or other designated Medicaid enrolled provider types that do not have the authority to bill Medicaid but can facilitate National DPP lifestyle change program sessions under the supervision of the billing provider. For example:
- The billing provider could be a health system (health clinic or hospital) and the rendering provider could be a CDC-recognized organization.
- The billing provider could be a physician or practice and the rendering provider could be a community health worker (CHW) or other licensed, credentialed, or designated Medicaid enrolled personnel trained to facilitate National DPP lifestyle change program curriculum. For example, in Minnesota, CHWs are the rendering provider and must work under the supervision of a physician or other qualified provider type (the billing provider) to be reimbursed by Medicaid for delivering National DPP services.
In these examples, both the billing and rendering provider will need to be enrolled in Medicaid and have an NPI.
3. An Existing Medicaid Enrolled Provider is the Program Provider
Some states use an existing provider type that becomes, or affiliates with, a CDC-recognized organization. An example of this could be a physician, advance practice registered nurse (APRN), or other practitioner who is eligible to bill and render Medicaid services. For example:
- In Montana, physicians, mid-level practitioners, and registered dieticians (who also hold a current Montana license as a nutritionist), are approved, among a list of other provider types, to receive Medicaid reimbursement for providing National DPP services.
- In Wyoming Medicaid pilot of the National DPP lifestyle change program, lifestyle coaches can only be registered dieticians who are Medicaid enrolled providers.
Existing vs. New Provider Types
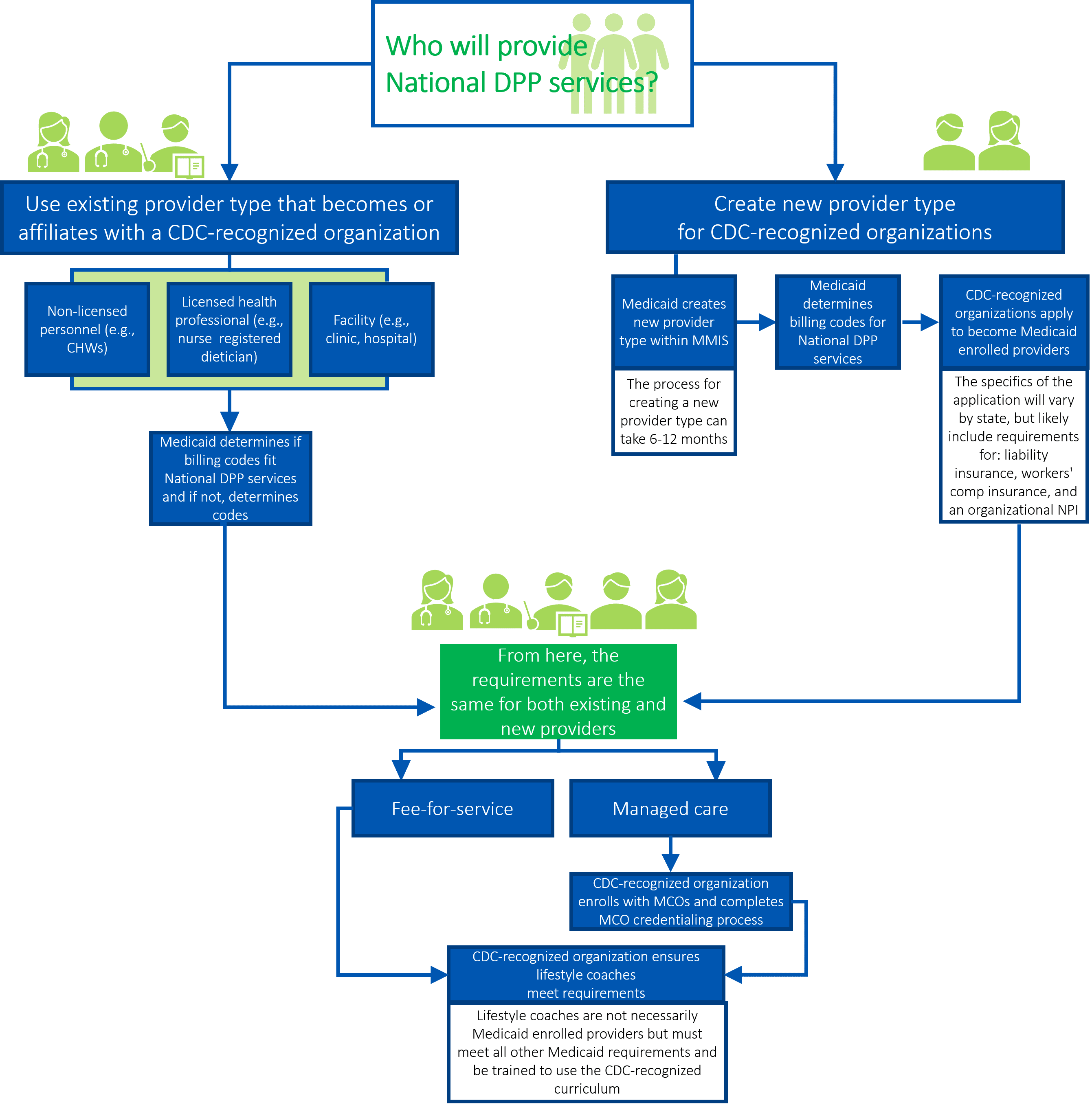
As outlined in the examples above, states can either use an existing provider type to deliver the program or they can create a new provider type. It is possible for states to pursue both options at the same time or to pursue one approach first and another approach at a later date. The graphic below depicts some key decisions involved in using an existing provider type and/or creating a new provider type.
Please note that regardless of whether Medicaid is using an existing provider type or creating a new provider type, the Medicaid agency will have to determine the mode of delivery for the National DPP lifestyle change program: in-person, online, distance learning, and/or combination.
Click a button below to learn more about using an existing provider type or creating a new provider type. Please download this summary document to understand the pros and cons of using an existing provider type and creating a new provider type.
Content last updated: May 20, 2021











