Cost & Value
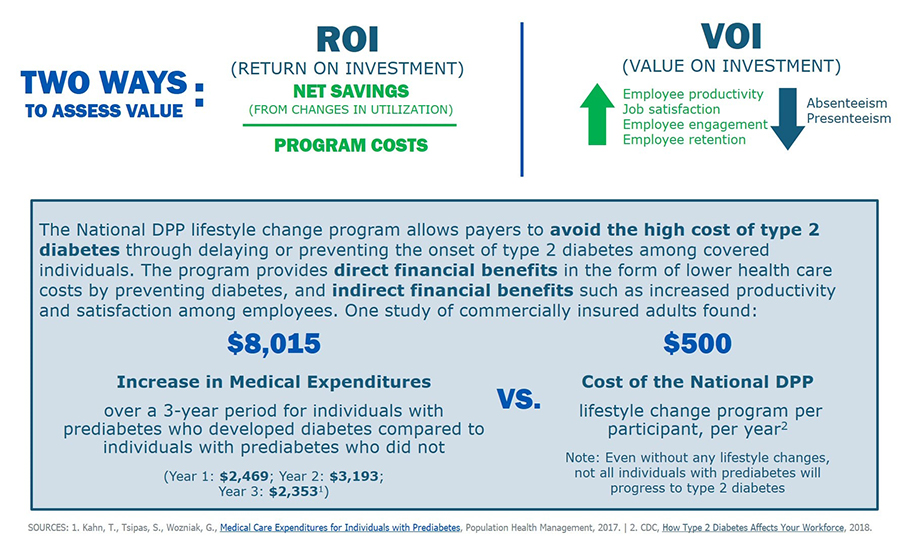
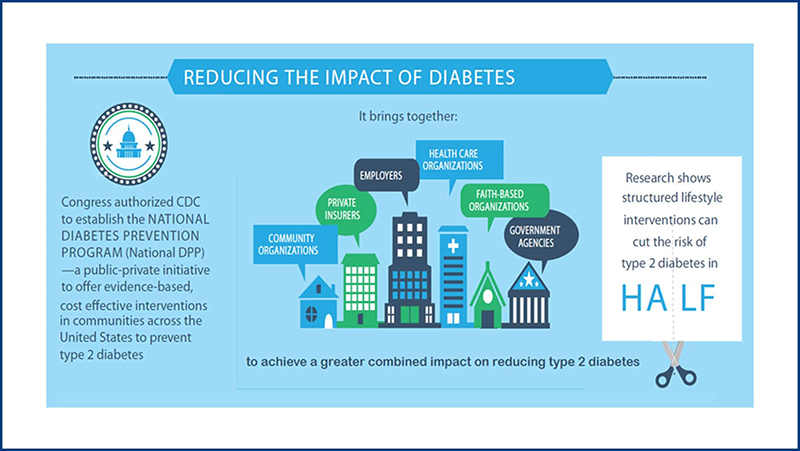
The image above summarizes some key cost and value considerations when covering the National DPP lifestyle change program. To learn more, see the following topics on this page:
- Analyzing Costs of Covering the National DPP Lifestyle Change Program
- Return on Investment vs. Value on Investment
- Costs Associated with Type 2 Diabetes
- Evidence Supporting the Cost Effectiveness of Prevention
- National DPP Lifestyle Change Program Costs
- Budget and Impact Tools
- All Payer Model
Analyzing Costs of Covering the National DPP Lifestyle Change Program
When considering coverage of the National Diabetes Prevention Program (National DPP) lifestyle change program, many public and private payers weigh the economic impacts of covering the program for their employees, clients, or public assistance beneficiaries. The impact of the National DPP lifestyle change program on health care costs can vary across populations and program types and can be affected by differences in how medical and non-medical costs are interpreted and applied, and by how the benefits of preventing or delaying type 2 diabetes are assessed.
Frequent concepts applied to analyzing overall costs of covering the National DPP lifestyle change program include return on investment (ROI), value on investment (VOI), cost-benefit analysis, cost-effectiveness, cost savings, and cost avoidance.
- Return on investment (ROI) measures the cost of an investment against the direct economic benefits it produces (i.e., gain or loss relative to the amount of money invested).
- Value on investment (VOI) is a broader financial analysis of all the benefits and costs of an investment for all impacted stakeholders. VOI includes variables that are more difficult to quantify such as quality of life, productivity, satisfaction, engagement, etc.
- Cost-benefit analysis compares the costs of running a program with the overall benefits accrued from that program’s outcomes.
- Cost-effectiveness is similar to a cost-benefit analysis, yet is a more general term that refers to the overall extent to which something is effective or beneficial in relation to its cost.
- Cost savings identifies a quantifiable reduction in expenses related to a specific input; also referred to as “hard cost savings” that impact a company’s bottom line.
- Cost avoidance refers to actions taken to avoid potential future expenses.
These concepts may be applied in various ways to help payers analyze the costs of covering the National DPP lifestyle change program against a wide range of benefits, including lowered (or avoided) medical costs, increased quality and/or years of life, chronic disease prevention, reduced absenteeism, etc.
Return on Investment vs. Value on Investment
Entities considering coverage for the National DPP lifestyle change program often begin by considering their bottom line: what will this cost my organization? This can be a challenging question to answer, given numerous factors such as expectations for future cost reduction, the extended timeline of chronic disease prevention, and questions of how to identify and calculate indirect benefits. This section provides key information to help stakeholders consider the costs and value of the program from various angles and differentiates between the return on investment (ROI) mathematical equation vs. a more inclusive value on investment (VOI).
Return on Investment (ROI)
Calculating Return on Investment
The ROI measures the cost of an investment against the direct economic benefits it produces. The calculation can be simple or complex depending on how it is being used and how exact the user wishes to be, but its core purpose is to determine whether savings will result from or are a result of a specified change. The ROI can be forecasted prior to implementing a change or a policy, or it can be calculated after implementation. The ROI is one of many factors an organization may consider when choosing to initiate or continue coverage of the National DPP lifestyle change program.
ROI Formula
Using this formula outlined below, the returns generated from the National DPP lifestyle change program are greater than the program costs if the ROI is greater than 1. If the ROI is between 0 and 1, the returns generated are not enough to recoup the program costs.
One of the most important factors when calculating the ROI relates to determining which costs are tied directly to the intended audience. Only savings and costs to the intended audience (in this case the payer) should be included. For example, if the ROI is being calculated for a state Medicaid agency that is covering the National DPP lifestyle change program, it would not be necessary to include costs incurred by the CDC-recognized organizations to incentivize participation in the program.
Another consideration is how quickly the ROI is achieved. The time value of money means that currently available money is worth more than the identical sum in the future, because of its earning potential and inflation. For example, if two programs both generate the same ROI, but one achieves the ROI in three years while the other achieves the ROI in five years, the three-year ROI is worth more because the savings are realized sooner.
ROI Resources
Below are resources from multiple stakeholders and perspectives that are intended to guide the process of calculating an ROI. When calculating an ROI for information or decision-making purposes, individual companies should consult with a finance expert within their organization.
- ROI Toolkit: A Guide for Conducting a ROI Analysis of your Community Health Worker Program
- Conducting a Program Cost Analysis for Medicaid-Public Health 6|18 Prevention Programs
- Toolkit for Using the AHRQ Quality Indicators: Return on Investment Estimation (for hospitals)
- The Medicaid Return on Investment Template
Value on Investment (VOI)

The benefits received from the National DPP lifestyle change program extend beyond direct financial benefits. There are many other benefits, such as improved quality of life or higher employee engagement, that are more difficult to quantify. VOI is another type of financial analysis that attempts to capture the broader impact that the National DPP lifestyle change program can have, including benefits and costs to both the intended audience (such as the payer) and additional impacted stakeholders. For example, the graphic below shows some of the many benefits employers may receive or produce from covering the National DPP lifestyle change program that extend beyond the direct financial benefits.
VOI has gained traction in the employee wellness space, and the concept is applicable to other payers as well. For example, the National DPP lifestyle change program’s goals of 5-7% weight loss and maintenance of regular physical activity may likely help to prevent or improve symptoms of other chronic conditions or diseases, and improve overall quality of life (for more information on these secondary health outcomes, visit the Evidence page of the Coverage Toolkit).
Another potential benefit of covering the National DPP lifestyle change program is tied to the overall satisfaction of participants. Studies, such as the evaluation from the Medicaid Coverage for the National DPP Demonstration Project, indicate high levels of satisfaction with the program from those who have completed it. Another recent study published in the Journal of Clinical Medicine assessed the outcomes and perceptions of 89 adults who participated in a lifestyle modification program modeled after the National DPP lifestyle change program. The majority perceived high benefits and low barriers to program participation, including: helpful interaction with health coach or program leader (73%), improved lifestyle modification due to the program (65%), and satisfaction with the program (75%). Additionally, responses from an internal Omada Health (an online CDC-recognized organization) survey given to their National DPP lifestyle change program participants between December 2016 – December 2018 found that 42% of respondents indicated that participating in the program significantly increased their employer or health plan appreciation (another 24% indicated a moderate increase and 12% a slight increase). While it may be difficult to quantify the economic benefits associated with the high levels of satisfaction of individuals participating in the National DPP lifestyle change program, beneficiaries and employees may be more likely to stay with a health plan or an employer that offers quality and satisfactory programs.
VOI Resources
- ROI vs. VOI: Which Is Better For Evaluating Your Wellness Program?
- Move From ROI to VOI (Value on Investment) – Includes tips on how to communicate the VOI
- Beyond ROI: Building employee health & wellness value of investment – A research study that explored whether employers are offering health and wellness programs for reasons beyond health care cost savings
Costs Associated with Type 2 Diabetes
A brief background on the costs of treating and managing type 2 diabetes in adults is central to discussions on the economic value of prevention. Currently, it is estimated that over 38 million people in the U.S. have type 2 diabetes (diagnosed or undiagnosed). Another 97.6 million adults (or approximately 38% of the adult population) are estimated to have prediabetes, which puts them at high risk for developing type 2 diabetes in the absence of intervention.
The costs of treating and managing diabetes is high and continues to grow. In 2022, the total cost associated with people with diagnosed diabetes in the U.S. was $412.9 billion. Medical expenditures constituted $306.6 billion of that total, and reduced productivity was estimated at $106.3 billion. Approximately one in four health care dollars is spent on people with diagnosed diabetes in the U.S., 61% of which is attributable to diabetes. The costs associated with diabetes have also accelerated in recent years. Economic costs of diabetes increased 26% from 2012 to 2017 due to a higher prevalence of the disease and increased costs of treatment. In 2022, the overall estimated prevalence of diabetes remains relatively stable in comparison to 2017; however, the actual number of people with diabetes has grown and contributes to increased health care expenditures, especially on inpatient hospital stays and prescription medications.
On an individual level, the incremental rise in costs of diabetes are shown to begin at least 5 years before diagnosis of the disease and accelerate immediately after diagnosis. People with diagnosed diabetes incur an annual average of $19,736 in medical expenses ($12,022 of which are attributable to diabetes) – about 2.6 times more than a person without diabetes. One study of commercially insured adults found that health care costs for an individual with prediabetes that is subsequently diagnosed with diabetes is $8,015 more in the first 3 years after diagnosis than individuals with prediabetes who are not subsequently diagnosed with diabetes. People with diabetes are also at higher risk for other serious health problems, including heart attack, stroke, blindness, kidney failure, and amputation of toes, feet, or legs.
References for the information offered in this section:
- American Diabetes Association, The Cost of Diabetes
- American Diabetes Association, Economic Costs of Diabetes in the U.S. in 2022
- Centers for Disease Control and Prevention, National Diabetes Statistics Report, 2022
- Population Health Management, Medical Care Expenditures for Individuals with Prediabetes
- American Diabetes Association, Statistics by State
Evidence Supporting the Cost Effectiveness of Prevention
A number of studies apply the various constructs of cost-benefit analysis, ROI, cost savings, and cost avoidance in assessing the economic impact of the National DPP lifestyle change program. These and other reports are included on the Evidence page of the Coverage Toolkit.
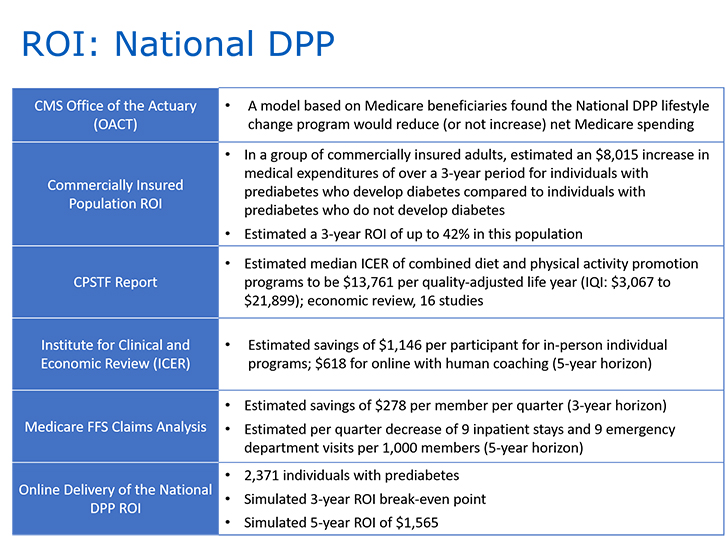
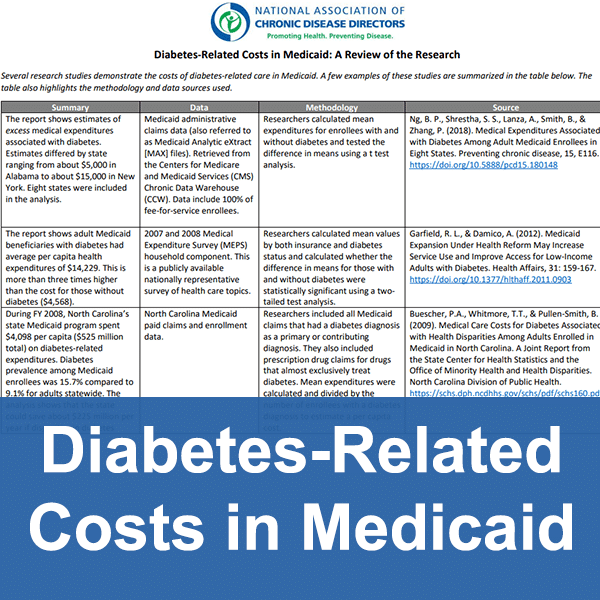
Additional information about the studies in the graphic above can be found in the tabs below.
CMS OACT Certification Report
CMS Office of the Actuary (OACT) released a certification report for expansion of the Y-USA National DPP lifestyle change program in March 2016. It reviewed results from the first two years of the Y-USA National DPP lifestyle change program implementation, the original DPP clinical trial, and a subset of lifestyle change programs recognized by the CDC.
The report confirmed the results and certified that an expansion of the National DPP lifestyle change program in the Medicare population would reduce (or not increase) net-Medicare spending using an actuarial analysis of Medicare beneficiaries. This was the impetus for Medicare to establish coverage for the Medicare DPP (MDPP) effective April 2018.
The analysis showed a slight cost to the Medicare program if potential reduced mortality and additional years of Medicare coverage are considered. However, the certification report did not require the mortality information.
Commercially Insured Population ROI
In 2017, researchers published a study in the journal Population Health Management in which they conducted a cohort analysis of commercially insured adults and illustrated how reducing the risk of developing diabetes by participating in an evidence-based lifestyle could yield both positive net cost-savings on medical care expenditures and ROI. The study estimated an $8,015 increase in medical expenditures over a 3-year period for individuals with prediabetes who develop diabetes compared to individuals with prediabetes who do not develop diabetes. This study also estimated a three-year ROI for the National DPP lifestyle change program of up to 42% in this population, based on an estimated $450 per person cost for the National DPP lifestyle change program.
CPSTF Report
The Community Preventive Services Task Force conducted an economic review of 28 studies (January 1985 – April 2015) and found that combined diet and physical activity promotion programs (such as the National DPP lifestyle change program) for people at increased risk for type 2 diabetes are cost-effective. Twenty-one of the reviewed studies assessed the cost-effectiveness of these interventions by estimating incremental cost-effectiveness ratios (ICERs) from the health system perspective (using only direct medical costs, including costs associated with program delivery and medical costs averted from preventing or delaying type 2 diabetes and its complications). For these studies, the Task Force found the median ICER of combined diet and physical activity promotion programs per quality-adjusted life year (QALY) was $13,761. (IQI: $3,067 to $21,899; 16 studies). The variation in ICERs was explained by variation in cost and effectiveness of the programs, program delivery modes, patient follow-up times, and delivery settings.
ICER Report
The Institute for Clinical and Economic Review report used a potential budget impact model and estimated cost savings of $1,146 per participant for in-person classes and $618 for online (over a five-year horizon). For private payers, the report recommended that the National DPP lifestyle change program be covered using a pay-for-performance model across all lines of business and products, and that payers should encourage their clinical networks to support active outreach and screening for prediabetes.
The potential budget impact was modeled based on the assumption of 1.9 million individuals from across the nation, ages 18 and older, across all payer types, participating in the National DPP lifestyle change program in the first year. The estimated program costs used did not include start-up costs.
Medicare FFS Claims Analysis
A 2017 study used claims analysis to evaluate the total medical costs for fee-for-service Medicare beneficiaries participating in the National DPP lifestyle change program administered by the YMCA of the USA. Participants were enrolled in lifestyle change programs across the country in seventeen YMCAs. The study used regression analysis to examine the average quarterly savings per member associated with participation in the National DPP lifestyle change program. Medical costs of program participants were evaluated against a matched comparison group of nonparticipants over a three-year period. Using a weighted average, per member per quarter savings were found to be $278 over a three-year intervention period.
The study also found the National DPP lifestyle change program to be associated with decreases in inpatient admissions and emergency department (ED) visits. Analysis of the full sample indicated that the intervention was associated nine fewer inpatient stays and nine fewer ED visits per 1,000 participants per quarter.
Online Delivery ROI
A study entitled “Return on Investment for Digital Behavioral Counseling in Patients with Prediabetes and Cardiovascular Disease” looked at 2,371 individuals with prediabetes, and/or who were at risk for cardiovascular disease. The participants enrolled in a one-year online program (an enhanced version of the National DPP lifestyle change program) through Omada Health between 2012 and 2014. The study used a Markov-based model to simulate clinical and economic outcomes annually over 10 years. The model included a constructed population across all payer types with an average age of 49.8 years. The simulated ROI break-even point was three years for both individuals with prediabetes and individuals with high cardiovascular disease risk, with a simulated five-year ROI of $1,565 for the prediabetes population. These findings suggest that online delivery of prevention programs can have a positive return on investment.
National DPP Lifestyle Change Program Costs
Program costs are an important part of the equation when calculating an ROI or VOI. It could be useful to benchmark program costs by using the most current CMS Calendar Year MDPP Payment Rates, which are updated annually for inflation. In addition to the per participant cost of delivering the program, it may cost as much as an additional $500 per participant for program costs related to removing barriers to participation, providing program supports, addressing health-related social needs, etc. Organizations interested in offering the program can use the American Medical Association’s National DPP Lifestyle Change Program Budget Considerations Tool to estimate the cost implications of offering the program.
Activities that drive program costs include facility fees and direct program delivery costs such as staffing costs. Some of these delivery costs may be higher in a Medicaid context than in other populations. For example, because the population can be more transient, it may be more time- and labor-intensive to reach potential participants and determine their eligibility. In addition, transportation is more likely to be a barrier to participation and program retention than for other populations, and Lifestyle Coaches may need to spend more time outside of actual classes to follow up with participants and to ensure that they continue to participate.
Program Costs in Practice
Montana
A program manager from the Montana Department of Public Health and Human Services (Montana DPHHS) indicated the following about their reimbursement rate relative to actual cost:
“The $500 covers the basic education, the facility cost, and interactions between the coach and the participants. It may not cover some extra services which may be financed by in-kind contributions or donations. A lot of the DPP provider organizations add different value-added services such as a gym membership. Montana Medicaid has a benefit so that a beneficiary can call to get a ride or can secure reimbursement for gas. To address child care needs, we have not yet found a universal solution, but some facilities have onsite child care (e.g., YMCA). A few sites have provided incentives.”
Direct medical costs for the original DPP clinical trial were $2,780 per participant over three years. However, this featured an individual (rather than group) coaching model facilitated by case managers.
Medicaid Demonstration
During the Medicaid Coverage for the National DPP Demonstration Project, a cost study of state agency, managed care organization (MCO) or coordinated care organization (CCO), and CDC-recognized organization costs were completed. A breakdown of the percentage of costs that were associated with administrative, recruitment, retention, data collection, and delivery activities for the National DPP lifestyle change program can be found here. The average cost to established CDC-recognized organizations to deliver the program was $1,529 per program participant and the average cost to new CDC-recognized organizations was $1,704 per program participant. The average cost to online CDC-recognized organizations to deliver the program was $556 per program participant
YMCA
The YMCA program fee is $429 for the yearlong program. Consumers pay in a variety of ways, and YMCAs work with them if financial assistance is needed. Some payers pay a flat $429 fee regardless of how much of the program a participant completes. For claims-based reimbursement, a performance-based fee schedule is used, and payers pay claims based on the achievement of specific milestones. Average cost for the program are comprised of fixed and variable costs. When there are more participants in the program to absorb the fixed costs, the average cost can be substantially lower, but volume is key.
Denver Health
The Community Epidemiology and Program Evaluation Group conducted a cost analysis of the National DPP lifestyle change program at Denver Health in 2015, which was compiled in a report prepared for the State of Colorado. Micro-costing and program information for the Denver Health National DPP lifestyle change program was provided by Denver Health for costs incurred from October 2012 to the end of calendar year 2014. Nearly half of the program participants were Medicaid beneficiaries. Component costs included the following:
- Community health worker (CHW)/lifestyle coach staffing
- Program management and supervision
- Other program support staff
- Training
- HR costs
- Other direct costs
- Facility and other indirect costs
- Program development costs
The evaluation authors estimated that costs equaled $552 per participant who attended at least one session, and $1,428 per participant who attended at least nine sessions. About 50% of the cost was attributable to coach staffing, and another 19% to program management and supervision. The remaining 25% was attributable to facility and other indirect costs. Program development costs constituted a relatively small percentage.
Budget and Impact Tools
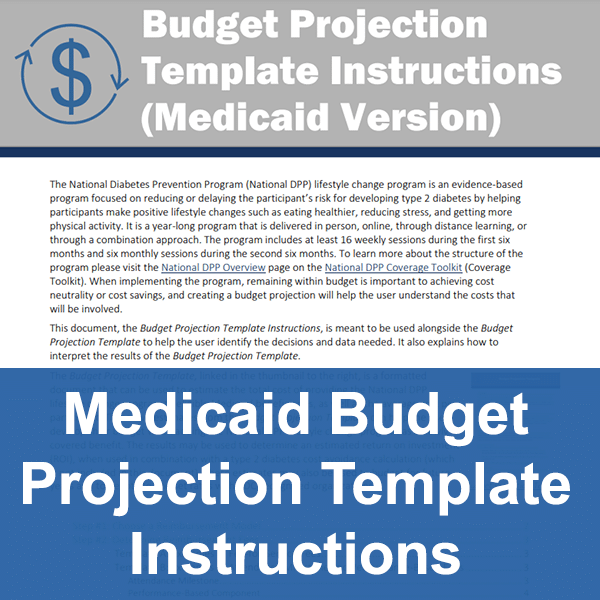
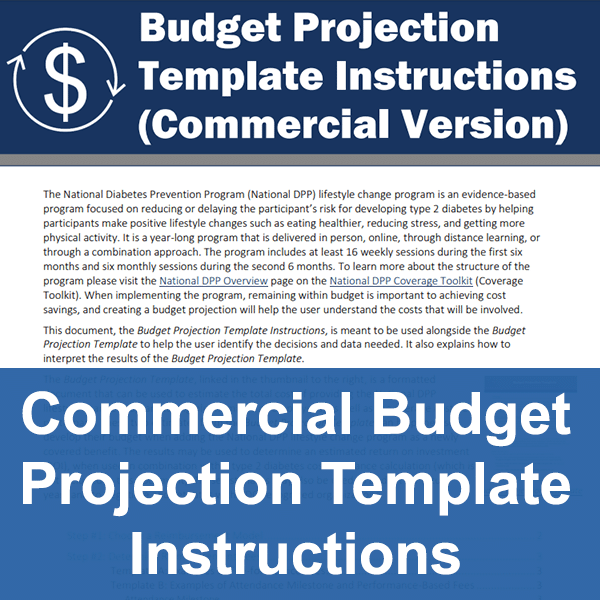
A number of different tools are available to help payers assess costs while considering and planning for coverage of the National DPP lifestyle change program.
Budget Projection
Impact Toolkit
- Additional information on the Impact Toolkit and the Cost Savings Calculator can be found here.
State Burden Toolkit
All Payer Model
Another consideration for determining the advantages of coverage is that the National DPP lifestyle change program is structured around an all payer model. Since the inception of the National DPP in 2012, the Centers for Disease Control and Prevention (CDC) and its partners have continued to focus on expanding the reach and coverage of the program so that all payers are involved – Medicare, Medicaid, state employee benefit plans, commercial health plans, and employers. Medicare started covering the program in 2018, a growing number of state Medicaid agencies offer coverage, and so do an increasing number of commercial and employer payers. In time, all covered lives at high risk for type 2 diabetes may have access to the National DPP lifestyle change program. To see which public and private payers are covering the program please visit the Participating Payers page.
The realization of an all payer model would also address the issue of turnover, or “churn,” in a covered population. This concern relates to scenarios in which a payer may cover the cost of the National DPP lifestyle change program only to have the program participants change plans, thus transferring the long-term savings or cost avoidance to another payer. In an all payer system, the risk of paying for a program without realizing the benefits would be minimized since the covered population at high risk for diabetes would have access to the program regardless of insurance plan.