Commercial Payers → Implementation → Screening and Identification for Commercial Payers
Screening and Identification for Commercial Payers
Commercial health insurance plans and employers can identify prospective participants for the National Diabetes Prevention Program (National DPP) lifestyle change program based on participant eligibility criteria.
This page contains the following topics:
- Eligibility Requirements for the National DPP
- Medical Claims or Electronic Health Records
- Tracking Eligibility Through a Claims System
- Identification by Providers
- Wellness Events
Eligibility Requirements for the National DPP
To be eligible for referral to a CDC-recognized lifestyle change program, patients must meet the following requirements:
- All of a program’s participants must be 18 years of age or older. The program is intended for adults at high risk of developing type 2 diabetes.
- All of a program’s participants must have a body mass index (BMI) of ≥25 kg/m2 (≥23 kg/m2, if Asian American).
- All of a program’s participants must be considered eligible based on either:
- A blood test result within one year of participant enrollment. Blood test results may be self-reported for CDC recognition purposes. Participants enrolled in the Medicare Diabetes Prevention Program (MDPP) cannot self-report blood test results; lab results must be provided. Blood test results must meet one of the following specifications:
- Fasting glucose of 100 to 125 mg/dl (Centers for Medicare and Medicaid Services-CMS- eligibility requirement for MDPP participants is 110 to 125 mg/dl);
- Plasma glucose of 140 to 199 mg/dl measured 2 hours after a 75 gm glucose load;
- HbA1C of 5.7 to 6.4; or,
- Clinically diagnosed gestational diabetes mellitus (GDM) during a previous pregnancy (allowed for CDC recognition and may be self-reported; not allowed for MDPP participants); or
- A positive screening for prediabetes based on the Prediabetes Risk Test online. Note: The risk test is not an option for eligibility for MDPP participants.
- A blood test result within one year of participant enrollment. Blood test results may be self-reported for CDC recognition purposes. Participants enrolled in the Medicare Diabetes Prevention Program (MDPP) cannot self-report blood test results; lab results must be provided. Blood test results must meet one of the following specifications:
- Participants cannot have a previous diagnosis of type 1 or type 2 diabetes prior to enrollment.
- Participants cannot be pregnant at time of enrollment.
- A health care professional may refer potential participants to the program, but a referral is not required for participation in a CDC-recognized program.
To be eligible for the National DPP lifestyle change program, individuals must have one of the blood test results described above, be previously diagnosed with gestational diabetes, or score positive for prediabetes on the CDC/ADA Prediabetes Risk Test. The CDC Diabetes Prevention Recognition Program (DPRP) standards require that at least 35% of a program’s participants be diagnosed with prediabetes through blood testing (or have a history of gestational diabetes). The remaining participants in the group can be considered eligible for the program based on their scores on the CDC/ADA Prediabetes Risk Test. The CDC/ADA Prediabetes Risk Test is a brief seven question survey that allows one to gauge their risk of having prediabetes. Regularly scheduled biometric screenings may be an opportunity to determine if an individual is eligible.
Health Plan A
One health plan contracts with an online CDC-recognized organization to provide the program to many of its members. With this provider, a multi-step screening method is used to identify eligible participants for the program.
Members may first receive an email or other invitation from their employer’s communication campaign inviting them to take a screening test on the CDC-recognized provider’s website. Once the member has completed the initial screening and is identified as potentially being at risk for diabetes, the member is invited to take a more in-depth screening that assesses the member’s health and readiness to change. The CDC-recognized provider reviews the assessment and decides whether to invite the member to participate in the program.
Medical Claims or Electronic Health Records
Some organizations have leveraged electronic health record data and/or medical claims data to proactively identify individuals who are, or may be, eligible for the program. For instance:
- The Kentucky Employees’ Health Plan identifies potentially eligible individuals through a post-visit claims review. Algorithms detect members who potentially have prediabetes. These individuals are contacted by phone and email and connected to the nearest CDC-recognized organization to enroll in the program.
- Another health plan also identifies individuals for the program by mining EHR data for persons who meet program criteria, after which physicians are notified for referral.
- Some health systems, health insurance plans, and employers identify eligible members through lab-confirmed A1C levels that place them in the prediabetes range.
Querying a Medical Claims Database or EHR
There are several billing and procedure codes that could be pulled from a medical claims database or EHR to identify potentially eligible individuals. For example, a query could be set up to pull information required for program eligibility. In instances where a specific lab value is required for inclusion, the actual lab value should be pulled. The program eligibility criteria for the National DPP lifestyle change program are listed below, with potential codes and other query-able elements listed in the columns to the right of each criteria. The presence of an x at the end of the code indicates there are multiple code modifiers or options for each of those codes.
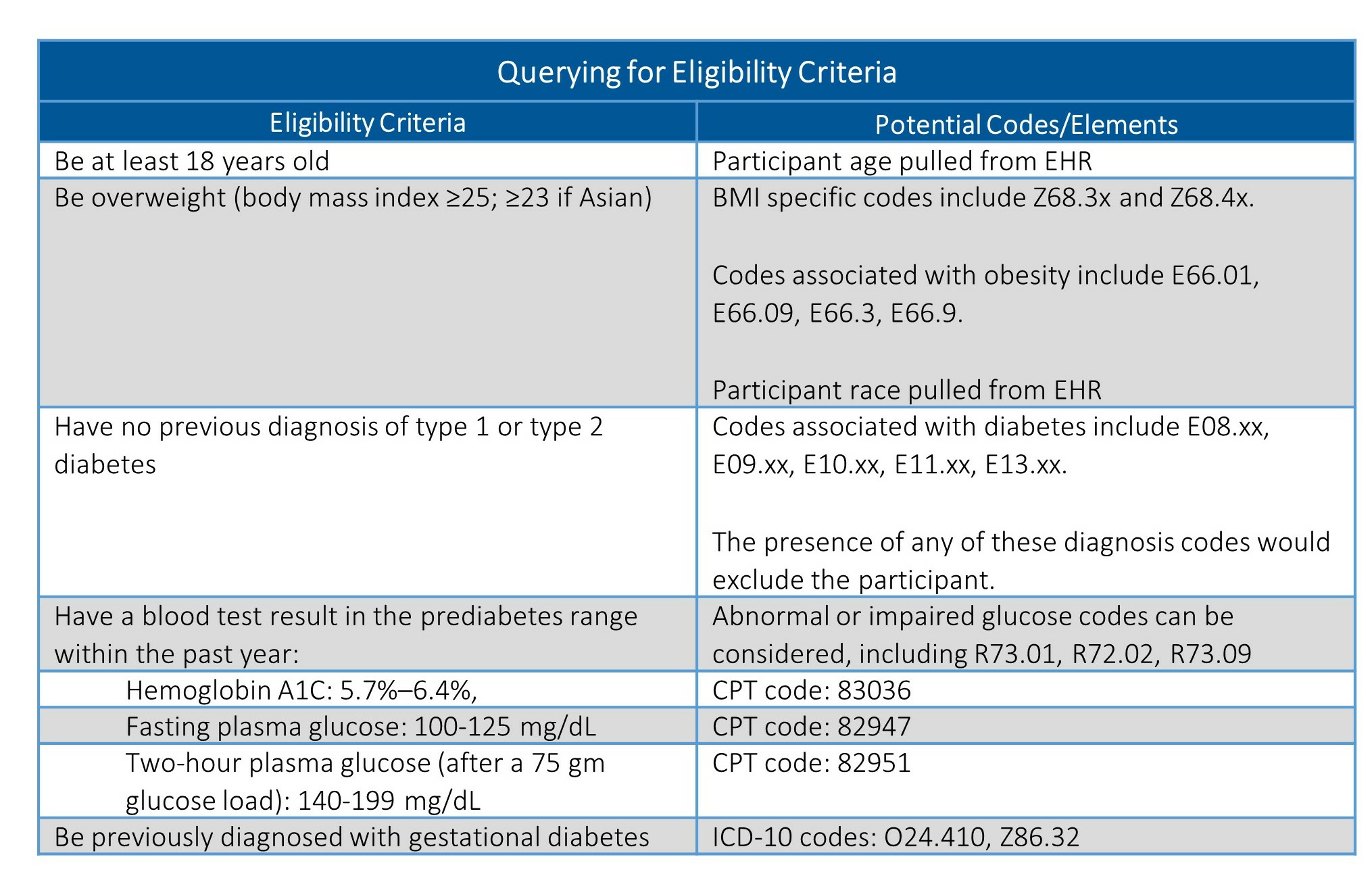
A description of many of these codes, as well as applicable office visit or procedure codes, can be found on the AMA’s list of codes to use when screening for prediabetes and diabetes. While the ICD-10 and CPT codes should be consistent across facilities, how databases are structured and queried is likely to vary. It is important to engage a database expert within your organization early in this process to understand how best to refine your query.
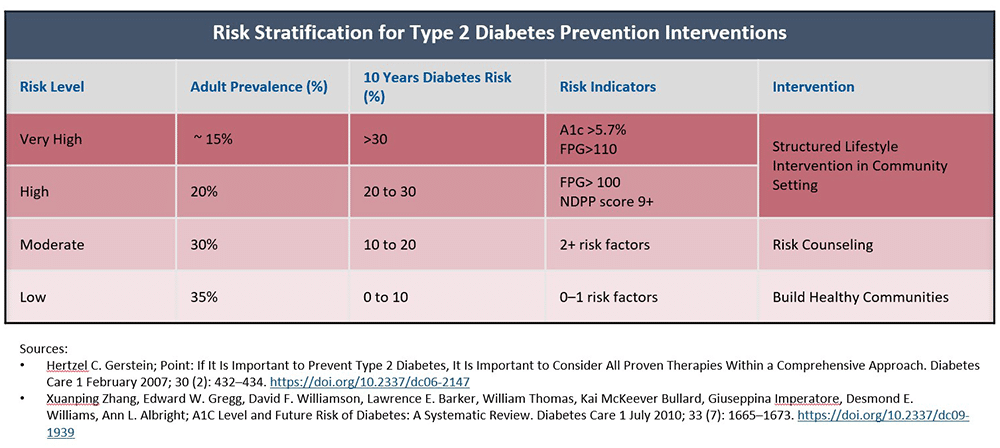
Risk Stratification
Once this data is collected, it could then be stratified to determine which individuals are at the highest risk of developing diabetes and could most benefit from this program. Below is an example risk stratification table, informed by information in the cited articles, which could be used to assess potential participants and how broadly or narrow a plan may want to extend access to the program.
Tracking Eligibility Through a Claims System
A subject’s participation in the program can also be tracked by following the submission of claims as they are received. This provides information on whether or not the participants are both attending and meeting milestones in the program.
For more information on coding for the National DPP lifestyle change program in a claims system, see the Coding and Billing page.
Identification by Providers
In other states and implementations, providers have been trained to assist in identifying individuals at risk for type 2 diabetes.
Health Care Provider Videos – Prediabetes and the National DPP
These videos were developed to encourage health care teams to work together and with their patients to identify prediabetes and increase referrals to the National DPP lifestyle change program. These videos were created by NACDD in collaboration with the AMA and through support from the CDC, Division of Diabetes Translation.Team-Based Care: Clinical Care Management and the National DPP
This video, based in a hospital, highlights the responsibility of care management in implementing and sustaining effective diabetes prevention strategies by health care providers, including referrals to the National DPP lifestyle change program.
Timing: 3:18 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Team-Based Care: Clinical Care Team Roles and Responsibilities for Diabetes Prevention
This video, based in a clinical setting, explores the different roles health care team members can play in identifying patients with prediabetes and providing care and follow-up, including referrals to the National DPP lifestyle change program.
Timing: 4:05 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Clinical Care: Prediabetes Identification and Treatment
This video illustrates how health care providers can help their patients address prediabetes through referral to the National DPP lifestyle change program.
Timing: 4:18
Audience: Clinical Care team (physician, nurse practitioner, physician’s assistant, nurse, medical assistance, care manager, care coordinator, etc.)
Wellness Events
Some commercial plans and employers have found that an effective screening and identification mechanism is a worksite wellness event or health fair. These events frequently include a biometric screening or the opportunity for members to take a risk assessment with a tablet or with paper and pencil. Members or employees found to be at risk for type 2 diabetes may receive an immediate referral and be placed in contact with a local in-person or online CDC-recognized organization.