Medicaid → MCOs and Value-Based Care → Engaging ACOs
How to Engage ACOs in the National DPP Lifestyle Change Program
Accountable care organizations (ACOs) are one of the most common types of alternative payment arrangements in the transition to value-based health care in the United States. ACOs and other types of alternative payment arrangements (also called value-based payment arrangements) are meant to change the incentives to better enable health care providers to keep patients healthy. Given these changed incentives, ACOs can be important partners in the effort to advance the National Diabetes Prevention Program (National DPP) lifestyle change program.
This page is intended to provide National DPP stakeholders with information about ACOs and specific strategies for how to engage ACOs in the effort to prevent type 2 diabetes. Throughout this page “National DPP stakeholders” is a term used to describe a broad category of entities and individuals interested in advancing diabetes prevention, including public health departments, state Medicaid agencies, CDC-recognized organizations, and any other entity or individual working to prevent type 2 diabetes.
This page is divided into four sections:
- What Are ACOs? An Overview of the Transition from Fee-For-Service to Value in Health Care
- How Can ACOs be Partners in the National DPP?
- How Can National DPP Partners Outreach to ACOs?
- How Can National DPP Partners Promote ACO Engagement?

What Are ACOs? An Overview of the Transition from Fee-For-Service to Value in Health Care
The Movement to Value
The movement to value refers to the health care industry’s collective efforts to realign financial incentives to reward the value of care provided as opposed to the volume of services provided. In the status quo fee-for-service (FFS) model that is prevalent today, providers are reimbursed for every service and procedure they provide and thus the more services provided, the more the provider is paid. The FFS environment lacks incentives for prevention. FFS also pays acute and subspecialty services much higher reimbursement rates than primary care and preventative services, rewarding intervention over prevention. Additionally, FFS often results in care that is not well coordinated, creating a frustrating health care experience for patients.
Conversely, in value-based payment arrangements, which have a history of receiving bipartisan support and attention from public and private payers, providers are financially rewarded for providing the “right care, at the right time, in the right place,” which means providing patients with the care that will keep them the healthiest in the lowest cost settings. Value also encourages providers, including both primary care providers and specialists, to coordinate a patients’ care across different care settings. Importantly, value-based payment is simply the mechanism that enables the real goal of the value movement, which is to fundamentally change how care is delivered in ways that promote health. Value-based payment arrangements can be implemented by public and private payers alike, and have been employed in Medicare, Medicaid, and commercial plans.
Value and Prevention
Value-based payments incentivize and enable care delivery changes that will ultimately reduce the overall costs of care and improve quality outcomes. Because of this, providers engaged in value-based arrangements focus on proactive disease management and prevention. For example, if a provider receives payment through a value-based payment arrangement, that provider has a financial interest in helping a patient with diabetes better self-manage their diabetes and avoid what can be frightening (and costly) emergency department visits as well as other negative health outcomes related to poorly managed diabetes. The provider paid under the value-based payment arrangement is also more incentivized to prevent patients from developing type 2 diabetes in the first place.
Accountable Care Organizations
In addition to expanding insurance coverage, the Affordable Care Act (ACA) also promotes the transition to value by encouraging the formation of ACOs. One of several different types of value-based payment arrangements, ACOs are groups of providers who are responsible for the cost and quality outcomes of a defined population of patients. Managing the health of a population of patients often requires providers to change how they deliver care. For example, providers may lengthen their appointment time with patients, conduct group visits for patients with the same health conditions, extend their clinic hours on nights and weekends, conduct home visits after release from the hospital to prevent readmissions, and help address patients’ social determinants of health (the social, economic, and environmental factors that influence health) as well as their mental health by staffing social workers in the clinic or hospital.
In 2018, about 10% of covered lives in America received care through an ACO. Providers can participate in ACO payment arrangements/contracts with both public and private payers, and ACOs can be led by physician groups, hospital systems, or a combination of the two. ACOs are a population health payment arrangement, meaning they strive to keep an entire population of patients healthy, and are different from other types of value-based payment arrangements, such as a bundled or episodic payments, which give providers accountability for the cost and quality of care within a specific episode, like a procedure or condition. Bundled payments are common for hip and knee replacements and childbirth.
ACOs and Total Covered Lives Over Time

Total ACOs by Contract and Provider Type

Source: Leavitt Partners Center for Accountable Care Intelligence
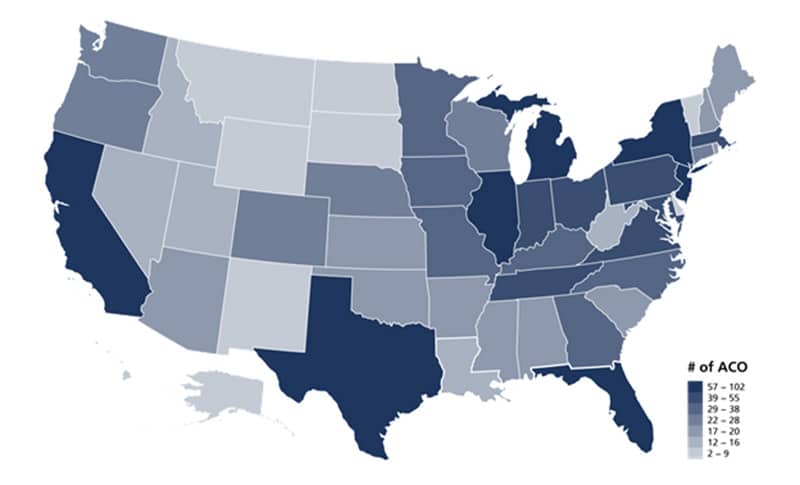
Number of ACOs By State
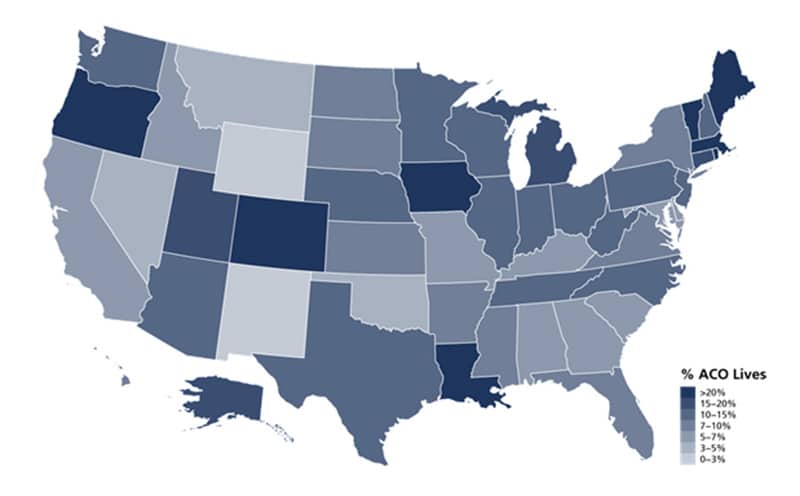
Percentage of Population Covered by ACO
Risk
Change to how care is paid for and delivered takes time and requires large investments in new technology, staff, and training. Given the scope of such change, providers’ financial accountability can change gradually. For example, providers new to ACO payment arrangements may elect to participate in “upside risk” only payment arrangements, which means that if the ACO achieves its quality and cost goals, the providers receive modest bonus payments (also called shared savings); however, if cost and quality goals are not met, the providers do not lose any money. As they become more comfortable and committed to the ACO payment arrangement, providers participate in “downside risk” payment arrangements, which means if providers meet their cost and quality goals, they receive larger bonuses, but if they do not, they actually lose money (also called shared losses). The end goal of the ACO movement is to have providers receive capitated or population-based payments, which means the ACO receives a designated per member per month amount of money and manages the cost of care to that budget. These value-based arrangements are more advanced and require providers to manage the full financial risk of a population’s health needs; however, they can also offer big benefits by giving providers predictable, prospective revenue and the flexibility to creatively invest in caring for patients’ clinical and non-clinical needs.
ACO Evaluation and Performance
ACOs are evaluated on how well they perform relative to a set of predetermined cost and quality measures. For example, depending on the specifics of the value-based contract with a payer, an ACO might have a financial benchmark that is either based on the ACO’s historical spending or the regional spending for the ACO’s geographic area, or a blend of both. At the end of the contract’s performance period (often 12 months), if an ACO’s actual expenditures are less than its benchmark, or projected expenditures, the ACO shares in the generated savings, often in the form of a bonus payment from the payer. To ensure ACOs are not saving money by reducing necessary care, ACOs also must achieve certain quality targets to receive financial savings. Typically, ACOs reduce the cost of care for their population of patients by helping patients to properly self-manage their health conditions and take their medications appropriately, and by providing care in lower costs settings (e.g., in the primary care physician’s office rather than the emergency room).
The goal of ACOs and the movement to value generally is to achieve the “triple aim”: reduce overall health care costs, improve population health, and improve the experience of receiving care. ACOs and other types of value-based payment arrangements have so far not been able to bend the overall health care cost curve, but they have shown promising results at the program level. For example, Medicare’s largest ACO program, the Medicare Shared Savings Program (MSSP) finally achieved net savings for the Medicare program in 2017 and 2018, after half a decade of spending below their benchmark, but receiving bonus payments from Medicare that actually increased overall costs to the Medicare program. As a federally-funded program, Medicare publishes publicly available performance data and results for Medicare ACOs. Performance results from private ACO programs are more difficult to find as that information is not required to be public. More information is known about the designs and performance of Medicaid ACO programs where some states have seen encouraging results, but the variation in states’ approaches makes it difficult to compare across Medicaid ACO programs. Transitioning from a fee-for-service to a value-based arrangement takes substantial time and effort and it can take several years for an ACO to achieve savings.
Quality Metrics
Quality metrics are tools that help measure progress towards goals to improve patient outcomes, improve patients’ experience of care, and improve the process of providing health care. Quality measurement and reporting is not a new practice or limited to value-based payment arrangements, but quality performance is an important part of all value-based contracts. In ACO payment arrangements, quality metrics are used to track whether an ACO maintains or improves patient outcomes and help ensure that providers are not withholding health services in order to generate savings. Quality measures are also used to drive change in care delivery, as the establishment of a quality metric creates an incentive for providers to meet that target. While many ACO programs do include quality metrics related to diabetes management, most do not have metrics specific to preventing the onset of type 2 diabetes. However, efforts are underway to better align ACO quality measures with a prevention-focus. In 2018, the American Medical Association (AMA) convened a cross-specialty, multidisciplinary technical expert panel (TEP) to identify and define new quality measures for prediabetes. The draft measures proposed by the TEP represent the first measures in the U.S. intended to assist in the prevention of type 2 diabetes.
Quality Metrics in Medicare ACOs
In order for Medicare ACOs to remain in good standing with the Centers for Medicare and Medicaid Services (CMS) and take part in shared savings they are required to report a set of mandatory quality measures to CMS. While CMS makes frequent adjustments to the programs’ quality metric set, currently, the largest Medicare ACO program only includes one measure directly related to diabetes (i.e., ACO-27 evaluates the control of hemoglobin A1c (HbA1c) among an ACO’s population with diabetes).
Quality Metrics in Medicaid ACOs
State Medicaid agencies interested in using an ACO payment arrangement have the flexibility to choose which quality measures they’ll ask providers to report and should think critically about which metrics are best suited to the specific care needs and disease burdens of their communities. There is considerable variety in state Medicaid ACO measurement approaches due to each state’s unique access, quality, clinical, and cost goals. Common measurement areas include (1) chronic condition management (e.g., asthma, diabetes); (2) emergency department use; (3) inpatient admission and readmission; (4) well-child visits; (5) patient experience; and (6) behavioral health.
For more information on quality metrics, see the Quality Metrics page of the Coverage Toolkit.

How Can ACOs be Partners in the National DPP?
For any National DPP stakeholder seeking to partner with ACOs to increase the reach and impact of the National DPP, it is helpful to first develop goals for envisioning how ACOs can be more involved.
National DPP stakeholders may generate their own additional goals, but three starting goals could be:
- Identify and refer eligible patients. Encourage ACOs to either start referring or increase their referrals of eligible patients to CDC-recognized organizations.
- Become a CDC-recognized organization. Explain how ACOs can seek CDC-recognition for one or more of their facilities or serve as a CDC-recognized umbrella hub organization for a network of affiliate CDC-recognized organizations.
- Engage as champions. Encourage ACOs to become champions in promoting diabetes prevention generally and the National DPP specifically.
More details on each of these ways ACOs can become more involved are provided below.
Identify and Refer Eligible Patients
One primary way ACOs can help advance the National DPP is to either begin or increase their efforts to identify and refer eligible patients to CDC-recognized organizations. Increasing referrals to CDC-recognized organizations both helps the ACO meet its charge to keep patients healthy and helps strengthen the National DPP through increasing the number of individuals benefiting from the program.
ACOs have made significant investments in technology that can be leveraged to increase referrals. The ACO mission to manage a population of patients and reduce costs relies, in part, on the ACO’s ability to effectively understand the health status and health care needs of their patient population. To do this, ACOs often have robust data collection and management platforms (e.g., electronic health records, registries, and health information exchanges) and analytics tools to identify patterns and gaps in care, often displaying these findings via data dashboards and other reports. ACOs are well positioned to use this technology to identify patients who have prediabetes and then refer those patients to CDC-recognized organizations.
Many entities promoting the National DPP lifestyle change program have found that individuals are more likely to enroll in the program when referred by their personal health care provider. National DPP stakeholders who want to engage ACOs can leverage the National DPP’s evidence, impact on quality metrics, and provider empowerment to make the case to ACOs for why increasing referrals to CDC-recognized organizations aligns with both the goals of the ACO and the goals of the National DPP.
For additional information on referrals, see the Recruitment & Referral page of the Coverage Toolkit. The American Medical Association (AMA) also provides tools specifically designed for physicians to identify and refer eligible patients to the National DPP lifestyle change program.
Become a CDC-Recognized Organization
ACOs can become even more involved in the delivery—not just the referral of patients—of the National DPP lifestyle change program by becoming a CDC-recognized organization. ACOs can determine which of its clinical facilities should seek CDC-recognition to deliver the National DPP lifestyle change program. Under this approach, the ACO would identify and refer eligible patients to their own on-site National DPP lifestyle change program. Clinics that are interested in pursuing this option must apply for CDC recognition and meet the Diabetes Prevention Recognition Program (DPRP) standards. One large health system that initially partnered with community CDC-recognized organizations experienced more streamlined referrals when the health system itself became CDC-recognized and could refer patients to its own program.
ACOs could also serve as an umbrella hub organization, a CDC-recognized organization that contracts with multiple affiliate community-based CDC-recognized organizations. The purpose of the umbrella hub arrangement is for organizations to partner to achieve scale and efficiencies with the National DPP lifestyle change program. The hub organization—in this case the ACO—becomes responsible for submitting claims to both public and private payers on behalf of the affiliate organizations, which, relieved of some administrative complexity, can more fully focus on delivery of the National DPP lifestyle change program. The ACO hub organization would benefit by being able to establish referral relationships with their affiliated CDC-recognized organizations for more streamlined referrals.
Engage as Champions
National DPP stakeholders can encourage ACOs to become champions in promoting the program, which could advance the diabetes prevention effort in several ways. First, the individual ACO is more likely to refer eligible patients to CDC-recognized organizations. Second, the ACO can become a persuasive voice in promoting funding for and awareness of the program. Providers’ influential position in the health care landscape makes their advocacy of a certain effort particularly meaningful when promoting that effort with the public, policy makers, payers, and other key stakeholders.
Case Study: Montefiore Health System
The following information comes from the study by Colin D. Rehm et al, “Lessons from Launching the Diabetes Prevention Program in a Large Integrated Health Care Delivery System: A Case Study,” Journal of Population Health Management, 2017.
- ACO: Montefiore health system is a large health care system located in the Bronx, New York and includes 11 hospitals and a network of primary care and specialty sites. Montefiore has been an ACO since 2012, first participating in CMS’s Pioneer ACO model and currently participating in the Next Generation ACO, CMS’s most advanced ACO model.
- National DPP experience: In 2011, Montefiore partnered with the YMCA of Greater New York to provide the National DPP lifestyle change program to eligible patients. YMCA staff trained Montefiore health educators to deliver the program and Montefiore providers referred eligible patients, who could choose to attend classes at local YMCAs, Montefiore care sites, or other community settings such as churches. Although the YMCA provided valuable experience and management of the program post-physician referral, the process of referring patients to an outside program proved administratively burdensome for Montefiore’s physicians. In 2015, Montefiore brought the program in-house by seeking CDC-recognition and integrating the referral process into the health system’s electronic health record (EHR).
- Outcomes: In the first 11 months of Montefiore bringing the program in-house, more than 1,250 referrals were made, and 282 patients placed in the National DPP lifestyle change program, (22.1 percent placement rate). At the time of the study’s publication (2017), of the 61 graduates from the fall/summer 2015 wave of classes, average weight loss was 3.8 percent and 38 percent lost more than 5 percent of their baseline body weight. Montefiore plans to add a measure of Montefiore’s National DPP referrals to their quality measure set, enabling the ACO’s leadership to see the aggregate referral volume (as a percent of total eligible patients).
- Lessons learned: Montefiore’s experience provides key lessons learned for other ACOs.
- Make referrals as easy as possible on providers by integrating referral documentation into the EHR.
- Minimize delays between a patient’s referral and outreach to enroll the patient in the program. A short interval between referral and outreach increases the likelihood of the patient enrolling in the program.
- Provide patients with a wide range of class options, including class times, locations, and languages. Master trainers that can train other lifestyle coaches can increase capacity to deliver the program.

How Can National DPP Partners Outreach to ACOs?
This section provides information for how National DPP partners can outreach directly to ACOs, including how to:
- Identify ACOs in a State or Region
- Determine ACOs for Outreach
- Outreach and Educate ACOs
- Understand and Address ACO barriers
Identify ACOs in a State or Region
Before attempting to engage ACOs it can be helpful to understand the landscape of ACO activity in a state or region. This can be done by identifying all ACOs and classifying organizations to determine which ACOs may be most receptive to the National DPP.
One way to classify ACOs is by the types of payers they are contracted with and in which value-based programs. Despite the common misconception that ACOs are limited to Medicare, there are ACOs that contract with Medicare, Medicaid, and commercial payers. As ACOs mature, many seek additional value-based contracts with other payers. The most advanced ACOs have multiple contracts covering a significant portion of their patient panels under accountable payment arrangements.
Medicare ACO Programs
Medicare provides lists of participating ACOs across each of its value-based payment arrangements.
- The Medicare Shared Savings Program (MSSP) – Medicare’s largest and most popular ACO program.
- Next Generation ACO Model (NGACO) – Medicare’s most advanced ACO payment arrangement.
- Comprehensive ESRD Care Model (CEC) – Medicare’s specialty ACO model focused on patients with End Stage Renal Disease (ESRD).
- Vermont All-Payer ACO Model – Medicare’s partnership with Vermont to administer a statewide ACO model including all payers.
In addition to ACOs, Medicare has other types of value-based payment arrangements that might be receptive to the National DPP. These include:
- Comprehensive Primary Care Plus (CPC+) – some physician practices concurrently participate in a Medicare ACO program as well as CPC+.
- Other alternative payment models (APMs) – some Medicare ACO provider practices are testing special programs and initiatives through the CMS Innovation Center to speed the adoption of best practices. Download the CMS Innovation Center Model Participants list here, which can be filtered by state, city, initiative, and/or organization name.
Medicaid ACO Programs
As of 2020, twelve states have implemented their own formal Medicaid ACO programs as part of the states’ strategy to contain costs and improve the quality of care for Medicaid enrollees. In addition to the states that have introduced their own official ACO programs, in other states, some ACOs are engaging with Medicaid managed care organizations (MCOs) on a one-off basis, to assume responsibility for Medicaid populations. Whether through the state’s official program or contracted independently, Medicaid ACOs are often comprised of safety-net provider organizations that agree to assume clinical and some measure of financial responsibility for an attributed Medicaid patient population. Medicaid ACO contracts can be held between states and provider entities, or between the state’s contracted Medicaid MCOs and provider entities. States’ Medicaid ACO purchasing strategies vary from state to state. The state Medicaid agency will be familiar with the Medicaid ACOs in their state.
In September 2020, CMS issued a letter to state Medicaid directors providing guidance for how states can implement or expand ACOs and other types of alternative payment arrangements for their Medicaid populations. This letter signals CMS’s ongoing commitment to advancing value in health care.
Commercial ACO Contracts
Many commercial payers utilize value-based payments to incentivize cost containment and continuous quality improvements among their contracted provider practices. As with public payers, the ACO payment arrangement is the most popular vehicle for value-based payment adoption among commercial payers to date. However, unlike public payers, commercial ACO contracts vary significantly, not only from payer to payer but also across a single payer’s ACO contract portfolio. This customization, and a lack of transparency in participants and performance, make commercial ACOs difficult to track. There are no publicly available databases that list all commercial ACOs. The state insurance commissioner may be able to ask the regulated plans to identify ACOs in their networks, although this would not generate information on the self-insured plans. Researching insurance plans on the state’s exchange marketplace may uncover which contract with ACOs as that could be perceived as a competitive advantage as people shop for plans on the individual market. Otherwise, word of mouth and internet research can surface ACOs that contract with commercial payers in certain states.
Leverage Associations to Identify and Reach ACOs
National ACO groups and professional associations can also be sources for identifying and outreaching to ACOs.
National ACO Groups
Several associations and collaboratives exist that can help National DPP stakeholders identify and engage multiple ACOs. For example, the National Association of ACOs (NAACOs) and the Accountable Care Learning Collaborative (ACLC) provide resources and host conferences, webinars, and other events that National DPP stakeholders could attend or become involved in through sponsoring or co-leading. In some states, independent provider or quality associations represent ACO interests (e.g., the New Jersey Health Care Quality Institute which maintains an ACO Council).
Professional Associations
A strategy for reaching a large swatch of ACOs is to outreach to provider professional organizations. State or local medical associations, nurse associations, primary care associations, and local Academy of Family Physicians groups may be effective groups to connect with as providers view these groups as their peers and advocates. These associations may be receptive to the reasoning that engagement with the National DPP will lead to more successful ACOs because helping patients prevent diabetes might improve the financial performance of the ACO.
Determine ACOs for Outreach
ACO activity varies from state to state. A common refrain is, “if you’ve seen one ACO, you’ve seen one ACO,” meaning there is considerable variety across ACOs. The implication of this diversity is that it is important to target ACOs that are likely to be receptive to engaging with the National DPP. This section provides strategies for determining which ACOs to target. It also offers ideas for understanding ACOs’ current diabetes prevention activities (if any).
ACOs With Which You Have an Existing Relationship
A pre-existing relationship with an ACO’s board member or executive may be particularly valuable for helping to add diabetes prevention to the ACO’s long list of priorities. That relationship may lead to an initial conversation with ACO decisionmakers that provides an opportunity to discuss the strategies included on this page for how to partner with ACOs to advance uptake of the National DPP lifestyle change program.
Mature ACOs
More mature ACOs may be more receptive to engaging with the National DPP. ACO maturity is defined by several factors including time as an ACO, level of financial downside risk the ACO accepts, and number of ACO contracts. An ACO that has existed for five or more years, accepts downside financial risk, and holds multiple contracts with government payers and private payers is considered more mature than other ACOs and may be better positioned to refer patients to the National DPP lifestyle change program or pursue CDC-recognition. National DPP stakeholders can find information to indicate maturity through surveying or interviewing ACOs and through secondary research (e.g., the ACO’s website).
ACOs Engaging with SDOH Factors
ACOs that currently provide direct support or connect patients to community resources, such as food banks, domestic violence shelters, and housing and transportation services, may have the infrastructure to more easily refer patients with prediabetes to local CDC-recognized organizations.
Understand Current Efforts.
Understand ACOs’ Current Type 2 Diabetes Prevention Efforts and National DPP Awareness
It may be valuable to understand the ACO’s current levels of awareness and engagement with type 2 diabetes prevention generally and the National DPP specifically, if this is not already known. This information may be available on the ACO’s website or obtained through surveying or interviewing ACOs.
Outreach to and Educate ACOs
After determining ACOs for outreach, it is important to create a strategy for outreaching to and educating ACOs. This section includes tips National DPP stakeholders can use to make the case to ACOs for why they should refer eligible patients or seek to become a CDC-recognized organization.
Make the Case
Make the case for why the National DPP is valuable to the ACO by emphasizing the program’s evidence, corollary health benefits, and existing nationwide infrastructure.
Evidence-Based
Explain to providers that the National DPP lifestyle change program is unique among weight loss programs because it is evidence-based and proven to prevent or delay the onset of type 2 diabetes. Explain how the original clinical trial establishing the program found it reduced participants’ chances of developing diabetes by 58 percent and that subsequent studies have confirmed this finding. For more information on the evidence base of the National DPP, see the Evidence page of the Coverage Toolkit.
Corollary Health Benefits
Make the case that patients’ healthier lifestyle choices as a result of participating in the National DPP lifestyle change program may contribute to a host of corollary benefits in addition to preventing diabetes. These additional benefits range from preventing other types of chronic conditions, such as hypertension and kidney disease, to improved mental health from healthier eating and more physical activity.
Nationwide Infrastructure
Alleviate providers’ concerns that engaging with the National DPP will translate into additional work for them by explaining a nationwide infrastructure for the National DPP lifestyle change program already exists. Highlight how the National DPP lifestyle change program is a readily available patient engagement solution and the ACO itself does not have to create the program within their clinics (unless it chooses to pursue CDC recognition). Explain there are many local in-person delivery sites and online programs available, all of which must adhere to CDC requirements.
Competitive Edge
Describe how diabetes prevention could be seen as a value-add for the ACO and the ACO’s members. If a provider discusses the National DPP with patients, those patients may feel a stronger allegiance to their provider who they perceive as genuinely looking out for their best interests. Explain how this may give that ACO a competitive edge over other ACOs, which could help that ACO reduce certain types of churn (e.g., churn due to a patient who is unhappy with their provider or clinic). Highlight that engaging with the National DPP might also generate positive publicity for the ACO. Explain how other ACOs are beginning to engage with the National DPP. For example, in June of 2019, Keystone ACO member Geisinger Health System’s type 2 diabetes prevention program earned full CDC recognition. Show how the AMA toolkit includes a short video on Park Nicollet’s, a primary care clinic that participates in ACO payment arrangements, engagement with the National DPP.
Appeal to Providers
Health care providers respond to evidence, recommendations from their peers, and knowing they can positively influence patient behavior.
Keep the Presentation Concise
Adapt educational material to be short and focused on the evidence of the program. Health care providers are data-driven and want to see the evidence that an intervention works. For more information on the cost-effectiveness of the National DPP, see the Cost and Value page of the Coverage Toolkit. For presentation templates, see the Case for Coverage for Commercial Plans and Employers page of the Coverage Toolkit.
Activate Peer-to-Peer Learning
Given their extensive training and unique position in society, health care providers often respond better to messages from peers. If a physician or other provider leader in an ACO is excited about the program, she or he can become an effective local champion and help generate enthusiasm for the program from their colleagues.
Explain How Health Care Providers Can Engage
Clearly describe the ways in which ACOs can engage with the program through referrals or through the clinic seeking to become a CDC-recognized organization to offer the program to patients onsite. (For more information on referrals, see the Recruitment and Referral page of the Coverage Toolkit.)
Highlight a Provider’s Influence and Pledge to Help Patients
Explain how patients who receive a referral from their physician are much more likely to enroll in a National DPP lifestyle change program. Health care providers want to do the right things for their patients, including helping them to prevent type 2 diabetes and achieve a healthier lifestyle. Tapping into that inherent desire to help the patient, while recognizing the burdens under which health care providers work, is important for effectively working with physicians.
Disseminate Existing Resources
A robust set of resources already exist on promoting and engaging with the National DPP. National DPP stakeholders can support an ACO’s engagement with the program by directing them to relevant resources specific to the ACO’s needs, including this Coverage Toolkit and AMA and CDC’s toolkit for health care providers. CMS has also created resources for Medicare ACOs that explain the Medicare Diabetes Prevention Program (MDPP) and how ACOs can become engaged, including, how the MDPP supports ACOs’ goals, and two steps for becoming involved: (1) educate patients and providers on prediabetes and available preventive services and (2) become an MDPP supplier and/or partner with nearby organizations to grow MDPP’s reach and impact. For more information, see CMS’s slides (PDF), audio (MP4), and one pager (PDF). Lastly, direct ACOs to any relevant podcasts on the National DPP they may be able to conveniently listen to on their way to work, such as CDC’s podcasts on type 2 diabetes prevention, the Association of Diabetes Care and Education Specialists’ podcasts on diabetes and prediabetes, and University of Kentucky’s HealthCare Regional Extension Center’s PILL podcast on preventive medicine and prediabetes.
Engage Leadership and Other Staff
Leadership and nurses can be powerful champions within the ACO. Care managers, care coordinators, and community health workers play an important role in connecting eligible patients to CDC-recognized organizations.
Identify and Outreach to ACO’s Leadership
National DPP stakeholders may present to the ACO’s leadership team and/or to a group of health care providers at the ACO. Clinical leadership (e.g., chief medical officer) may be the most receptive.
Engage the ACO’s Nurses, Care Managers, and Community Health Workers
Although engaging physicians can be effective, an ACO’s nurses, care managers (also called case managers), and community health workers may be strong champions as well. These individuals can identify for the ACO’s physicians or leadership team the opportunity to prevent diabetes through the National DPP. Moreover, care managers are responsible for helping ensure patients’ care is coordinated across multiple clinical sites and can help patients connect with local CDC-recognized organizations.
Encourage Operational Changes
Encourage ACOs to Risk Stratify Patients
Segmenting the patient population based on current and anticipated health needs is a common practice among ACOs. Risk stratification allows ACO providers to identify and proactively address patients’ care needs prior to escalation. ACOs can leverage these same stratification capabilities to better understand their organization’s needs and opportunities related to diabetes prevention (for more information, see the risk stratification table on the Screening & Identification page of the Coverage Toolkit).
Encourage ACOs to Leverage Their EHR
Work with an ACO’s administrative team to optimize the EHR for prediabetes alerts and referrals. For example, a patient’s lab results could flag for a provider that the patient’s Hemoglobin A1C levels are within the prediabetes range, or flag other warning signs like year-over-year weight gain, as well as patients with a family history of diabetes. Through the EHR, the provider might also be able to refer patients to a nearby CDC-recognized organization.
Understand and Address ACO Barriers
In many ways, National DPP stakeholders are in the vanguard of an important but not yet widely institutionalized intersection between public health and the health care sector. Although ACOs and National DPP stakeholders share the same goal of keeping people heathy, to date, engagement with the National DPP among ACOs has not been widespread. Currently, most ACOs’ preventive care activities focus on the Medicare annual wellness visit and ensuring patients receive their recommended vaccinations and cancer screenings. To understand how to work with ACOs as partners in the effort to advance the National DPP, it is important to understand the challenges ACOs face in implementing type 2 diabetes prevention.
Short-Term Goals
Challenge
Most ACOs operate on a 12-month performance measurement period, which means that ACOs must generate savings within a 12-month time period to be eligible for their bonus payments. Although the National DPP lifestyle change program generates cost savings, those savings are often not realized until several years after an individual completes the program. Therefore, while preventing or delaying the onset of type 2 diabetes generates cost savings for the individual and the larger health care system, an ACO may not reap the benefits of those savings given its short-term performance requirements.
Solution
National DPP stakeholders can educate ACOs and make the case that the National DPP lifestyle change program offers a host of corollary benefits for participants in addition to preventing type 2 diabetes. These additional benefits range from preventing other types of chronic conditions, such as hypertension and kidney disease, to improved mental health from healthier eating and more activity. The accumulation of these ancillary benefits from a healthier lifestyle will augment the ACO’s overall goals of keeping patients healthy, actively engaged and more educated about their own health, and out of high-cost sites of care, which could substantively contribute to the ACO’s short-term (12-month performance period) and longer term (3- to 5-year contract) ROI.
Management vs. Prevention
Challenge
ACOs save money by keeping people out of the hospital and one of the most effective ways to do that is by helping patients with one or more chronic conditions better manage those conditions (by taking their medication regularly, coordinating follow up care, and more primary care provider appointments, etc.) as well as addressing other non-clinical factors, like social, financial, or environmental issues, that may be barriers to disease management. Helping a patient stabilize and effectively self-manage their condition (so the patient doesn’t go to the hospital) has a far quicker ROI for the ACO than helping the patient prevent the onset of type 2 diabetes. Moreover, current quality measures have a strong focus on disease management rather than prevention, including type-2 diabetes management. Finally, given the range of health needs a provider must consider during a visit, chronic disease management likely takes precedent over chronic disease prevention.
Solution
National DPP stakeholders can use a similar strategy for this challenge as they do for the short-term financial performance challenge described above, such as making a case for how helping patients make healthy lifestyle changes can also help patients manage their other health care conditions exacerbated by being overweight, such as hypertension, heart disease, asthma, or depression. National DPP stakeholders can also highlight how the National DPP lifestyle change program is a readily available patient engagement solution. The ACO itself does not have to create the program within their clinics as the National DPP infrastructure is already developed nationwide. There are many local in-person delivery sites and online programs available.
National DPP stakeholders can point to early—yet promising—results from an ACO that has implemented the National DPP lifestyle change program. In early 2019, Geisinger Health System, a member of the Keystone ACO, launched a pilot National DPP lifestyle change program, which by late 2019 was found to be lowering patients’ AIC levels.
Finally, it is helpful for National DPP stakeholders to understand that chronic disease management is often the “low-hanging fruit” for ACOs to reduce their costs. More mature ACOs, those that have been in existence longer or accepted more downside risk, may be more receptive to prevention efforts since they likely already have well-running processes for disease management and can focus more attention on prevention. For more information on how National DPP stakeholders can segment ACOs and identify mature ACOs to target for outreach, see the “How Can National DPP Stakeholders Engage ACOs? Strategies for Success” section above.
Patient Churn
Challenge
In an ACO payment arrangement, attribution is the method of determining which patients an ACO will ultimately be held accountable for managing. Depending on the specific payment arrangement, patients are either attributed to the ACO prospectively (meaning at the beginning of the performance period) or retrospectively (meaning at the end of the performance period). This determination is often based on where they have received the plurality of their past primary care services. ACO payment arrangements are increasingly incorporating voluntary attribution to supplement this claims-based approach, whereby patients can proactively “enroll” by indicating their alignment with an ACO’s participants. However, most patients likely do not know they are in an ACO and patients may change primary care providers based on a change in insurance, a move, or a personal preference for a different physician. Even if a patient doesn’t move or change payers or providers, an ACO’s attributed patient participant list can change from year to year. This patient “churn” can add to ACOs’ challenge of generating an ROI within 12 months given the longer-term ROI associated with type 2 diabetes prevention and can disincentivize ACOs to invest in preventing conditions that take longer to develop, such as diabetes.
Solution
Given the prevalent model of health insurance in the U.S. that enrolls members for a 12-month period, after which time an individual may have insurance that provides them with a different network of providers, churn is a challenge across the health care industry. However, patient turnover should not preclude organizations from engaging in the National DPP lifestyle change program. For example, even though churn rates are highest among the Medicaid population, more and more states are covering the National DPP lifestyle change program for their Medicaid fee-for-service and managed care populations.
National DPP stakeholders can address the challenge of churn in several ways:
- Explain how a state’s Medicaid MCOs cover the program—despite the high levels of churn in the Medicaid population—out of a recognition that widespread prevention of type 2 diabetes ultimately benefits all health system stakeholders in the value movement.
- Describe how type 2 diabetes prevention might be a value-add for an ACO’s member, giving that ACO a competitive edge over other ACOs, which could help that ACO reduce certain types of churn (e.g., churn due to a patient who is unhappy with their provider or clinic).
- Help the ACO understand the broad impacts of lifestyle change across its patient population, including the prevention of type 2 diabetes, but also possible reductions in other key health metrics such as high blood pressure or cholesterol.
- Educate ACO payers—insurance companies that are actively contracting with providers via the ACO payment arrangement—on the value of the National DPP lifestyle change program. Insurance companies are strongly incentivized to prevent the onset of costly chronic diseases in their member population. Moreover, some insurance companies—especially those that dominant in certain markets—are more likely to retain members for more than just one or two years and therefore are more likely to realize the National DPP’s return on investment for those members.
Quality Measures
Challenge
ACOs are evaluated based on their performance on a set of quality measures. Although ACOs aim to keep all patients healthy and free from as many health conditions as possible, quality measures do incentivize ACOs to pay particularly close attention to the conditions directly referenced in their list of required quality measures.
Although many ACOs are measured on their ability to help manage patients with diabetes or patients with multiple chronic conditions (where diabetes is often present), there are currently no quality measures specifically dedicated to type 2 diabetes prevention. However, a quality measure is in progress. In 2018, the American Medical Association (AMA) convened a cross-specialty, multidisciplinary technical expert panel (TEP) to identify and define new quality measures for prediabetes. The draft measures proposed by the TEP represent the first measures in the U.S. intended to assist in the prevention of type 2 diabetes. The proposed measures address screening for prediabetes, providing intervention for those with prediabetes, and follow-up testing for those with prediabetes.
Solution
Even though a dedicated prediabetes quality measure does not yet exist, there are several other quality measures which the National DPP lifestyle change program could help achieve. For example, the 2020/2021 Medicare Shared Savings Program ACO quality measures include:
- Measure ACO-5: Health Promotion and Education. This quality measure is part of the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey for Medicare ACOs. ACOs that educate patients on the National DPP lifestyle change program may receive positive responses from survey participants on the topic of health promotion and education. All ACOs in the Medicare Shared Savings Program report on this measure. View the CMS data here.
- Measure ACO-28: Hypertension (HTN): Controlling High Blood Pressure. Although the National DPP lifestyle change program focuses on preventing type 2 diabetes, several studies have found an association between participation in the program and favorable changes in blood pressure (see Mudaliar 2016 and McTigue 2009). All ACOs in the Medicare Shared Savings Program report on this measure. View the CMS data here.
For more on quality measures for which the National DPP lifestyle change program is relevant, see the Quality Metrics page of the Coverage Toolkit.
Provider Burden
Challenge
Even in ACOs, health care providers often have limited face time with patients and must address a range of clinical care needs and administrative requirements. Preventing type 2 diabetes, or at least referring patients to a CDC-recognized organization for a type 2 diabetes prevention program, may not effectively compete with the long list of priorities health care providers must consider during a visit with a patient. For example, during an office visit, a health care provider may decide to address the patients’ other health care concerns, such as medication adherence, high blood pressure, a cancer screening, or referral to a smoking cessation program. Additionally, providers may have little or no awareness of the National DPP lifestyle change program.
In general, providers feel overburdened and at risk for burnout with the added administrative demands. Administrative burdens are multiplied by provider shortages, the implementation of electronic health records (EHRs), and the increasing expectations of the value movement to lower costs while improving quality amidst an increasingly unhealthy American population. This context can help National DPP stakeholders understand the realities in which many primary care providers work and how to best engage them in the National DPP.
In addition to competing demands, providers may perceive that helping their patients prevent type 2 diabetes through lifestyle change is outside their sphere of influence. Providers recognize the importance of patients with prediabetes losing weight, eating healthier foods, and exercising more regularly; however, providers may feel they have little ability to affect those types of behavior changes in their patients.
Solution
Educating health care providers about the National DPP is an important first step to engaging them as type 2 diabetes prevention partners and helping them understand both the evidence base of the National DPP lifestyle change program and also the extensive National DPP infrastructure that exists throughout the U.S. Explaining this infrastructure—including highlighting local CDC-recognized organizations—may give providers more optimism that they can indeed have a positive influence over their patients’ lifestyle choices. For more information on how to persuasively talk to providers, see the how to appeal to health care providers section of this page.

How Can National DPP Partners Promote ACO Engagement?
This section describes how National DPP partners can leverage statewide opportunities and use stakeholder specific strategies (e.g., strategies specific to state Medicaid agency and payers) to engage ACOs.
Leverage Statewide Opportunities
A state’s Department of Health and Medicaid agency can partner to convene a statewide effort to generate collaboration between the health care sector, including ACOs, and the state’s social services organizations, including CDC-recognized organizations, to advance the National DPP and other efforts to address disease prevention and social determinants of health.
Statewide Collaboration
There are several ways to create a state-wide collaboration that includes type 2 diabetes prevention.
- Medicaid could apply for an 1115 waiver. For example, in 2018, North Carolina received an 1115 waiver to implement the state’s transition to Medicaid managed care and to test a series of pilot initiatives to address Medicaid beneficiary’s housing, food, transportation, and interpersonal safety needs. For more information on how 1115 waivers can be used for coverage of the National DPP, see the Attaining Coverage Through a Section 1115 Demonstration Waiver page of the Coverage Toolkit.
- CMS created the Accountable Health Communities model to increase collaboration between the health care system and community-based social services organizations. National DPP stakeholders can examine the current list of participants to see if any entities (including ACOs) in their state are currently participating in the model. If so, those entities may be particularly receptive to referring eligible patients to CDC-recognized organizations.
- National DPP stakeholders could also determine whether their state or region has any Pathways Community HUB participants. Pathways Community HUBs exist to connect individuals in need to evidence-based social, medical, and behavioral health interventions. National DPP stakeholders could also implement a Pathways Community HUB in their area to facilitate collaboration between ACOs and CDC-recognized organizations.
SDOH Platform Integration
These statewide efforts can be enhanced through technology platforms, such as “Aunt Bertha” and “Unite Us,” that integrate health care and social service needs by connecting patients with community resources to address their SDOH. For example, in collaboration with Unite Us and other partners, North Carolina developed NCCARE360, a statewide platform that both connects individuals in need with community resources and provides a feedback loop on the outcome of those connections. NCCARE360 allows health care providers to refer patients to CDC-recognized organizations. National DPP stakeholders could emulate North Carolina’s approach by encouraging individual CDC-recognized organizations to connect directly with these platforms or a state agency—either the department of health or Medicaid agency—could organize an effort to have all the state’s CDC-recognized organizations included in the platform. Public health agencies could use their position as neutral conveners to drive this type of effort.
Engage Other Providers
National DPP stakeholders can also outreach to other types of providers, such as those providing behavioral health and oral health services. For example, clinics where behavioral health and primary care are provided in concert may find that referring eligible patients to the National DPP lifestyle change program helps improve patients’ mental health. Additionally, dentists are often the first to identify warning signs of early diabetes. Although dentists are not usually involved in ACOs, (except in Oregon’s Coordinated Care Organizations), they are another potential champion to bring the National DPP to patients’ attention and/or work with their physical health providers.
Utilize Stakeholder-Specific Strategies
Thus far this page has discussed strategies that may be applicable for a broad range of National DPP stakeholders. However, there are several specific strategies that certain stakeholders can use to incentivize ACOs’ engagement with the National DPP. For example, state Medicaid agencies could encourage type 2 diabetes prevention through a performance improvement project. Additionally, payers and self-insured employers are highly incentivized to prevent diabetes given the high costs of diabetes treatment and care. Finally, as purchasers of health insurance for their employees, fully insured employers are also incentivized to contract with insurers that help their enrollees prevent diabetes.
State Medicaid Agency
Encourage Preventive Diabetes-focused Performance Improvement Projects
Medicaid MCOs must conduct a state-defined number of Performance Improvement Projects (PIPs) annually to satisfy federal requirements to develop and implement a Quality Improvement Strategy under 42 CFR 438.240(d). The state Medicaid agency can require a diabetes prevention PIP in its MCO contracts.
Add a Diabetes Prevention Quality Metric
If there are ACOs in the state with Medicaid contracts, the state Medicaid agency may contract directly with those ACOs or the state’s Medicaid ACOs may contract directly with the ACOs. If the state contracts directly with the ACO, the state may determine the quality metrics on which the ACO is measured. To incentivize ACOs to take preventive steps for patients at risk of developing type 2 diabetes, the state can use a heat map to identify ACOs operating in regions of the state that have been identified as having a higher prevalence of diabetes. This would help target which ACOs should be required to include a quality metric that drives actions for patients who have been diagnosed with prediabetes, such as referral to a type 2 diabetes prevention program like the National DPP lifestyle change program. It is important for the state to remember that ACOs have a variety of quality measures and clinical needs to consider and the decision to add a quality measure must balance the opportunity to increase preventive care for patients with prediabetes without adding to the clinical or reporting burden of providers.
Payers
ACO Payers
National DPP stakeholders can educate ACO payers—insurance companies that are actively contracting with providers via the ACO payment arrangement—on the value of the National DPP lifestyle change program. Insurance companies are strongly incentivized to prevent the onset of costly chronic diseases in their member population. Moreover, some insurance companies—especially those that are dominant in certain markets—are more likely to retain members for more than just one or two years and therefore are more likely to realize the National DPP’s return on investment for those members.
Make Referrals as Easy as Possible for the ACO
In Maryland, all Medicaid MCOs in the state collaborated to produce a single National DPP lifestyle change program referral form that all Medicaid MCOs can give to their in-network providers. The form is branded with the Maryland HealthChoice managed care program logo rather than any individual MCO’s logo. The purpose of this coordination is to reduce the administrative burden on providers by using a single form.
Enable Risk Stratification
Payers will be key in defining a population of interest and should consider developing prediabetes patient risk scores to better understand which patients are most at risk for type 2 diabetes. Segmenting patients with prediabetes into different risk categories (e.g., among those with prediabetes, some may be at very high risk for developing type 2 diabetes, others at much lower risk) can be effective for targeting the patients at highest risk for developing type 2 diabetes. This type of segmenting could be attractive for ACOs that want to identify the patients who would most benefit from the National DPP lifestyle change program.









