Medicare → MDPP Basics
Medicare Diabetes Prevention Program (MDPP) Basics
The Center for Medicare and Medicaid Innovation Medicare Diabetes Prevention Program (MDPP) site is the primary source for information and resources regarding the MDPP. This page provides a brief overview of the MDPP, including the following topics:
- MDPP Services
- Beneficiary Eligibility Criteria and Referrals
- MDPP Supplier Eligibility and Enrollment
- Payment for MDPP Services
- Beneficiary Engagement Incentives
- Medicare Advantage Plans and the MDPP
- Additional Guidance
The MDPP expanded model allows Medicare beneficiaries to access evidence-based diabetes prevention services with the goal of a lower rate of progression to type 2 diabetes, improved health, and reduced spending. On March 23, 2016, the Department of Health and Human Services (HHS) announced that the Centers for Medicare and Medicaid Services (CMS) Office of the Actuary (OACT) certified that the National DPP lifestyle change program would “reduce net-Medicare spending.” MDPP suppliers began enrolling in Medicare on January 1, 2018, and began furnishing MDPP services and billing Medicare for MDPP services on April 1, 2018.
Medicare Advantage plans are also required to offer the benefit to their members. To learn more please see the Medicare Advantage Plans and the MDPP section below.
Some key differences between the CDC recognition requirements and the MDPP benefit should be noted, including:
- Age of beneficiaries (limited to those enrolled in Medicare Part B)
- CDC-recognized organization eligibility criteria versus MDPP supplier organization eligibility criteria
CMS has provided an interactive map showing MDPP suppliers in the United States. Use the map to help find MDPP suppliers in your area.
A list of frequently asked questions about the MDPP and answers from CMS can be found here.
Medicare DPP Promotional Materials for Part B Beneficiaries with resources specific to promoting the Medicare DPP to Medicare Part B beneficiaries and their health care providers that CDC has developed are available here.
Please note that Medicare is a government-sponsored health insurance plan for people aged 65 or older. Medicare has various parts, and the Medicare 101 & MDPP document outlines the distinct parts of Medicare, what services they cover, the associated member cost sharing, and where the MDPP fits in.
MDPP Services
- The MDPP is covered under Medicare Part B as a preventive service once per lifetime.
- Medicare cost sharing does not apply to MDPP services.
- Benefit description:
- Core services period is 12 months: 16 weekly core sessions over months 1-6, and 6 monthly core maintenance sessions in months 7-12
- Sessions are approximately one hour each
- No minimum or maximum number of beneficiaries per session
- Limited in-person and/or remote makeup sessions may be provided
- MDPP suppliers may use any CDC-approved lifestyle change program curriculum.
- Virtual delivery of MDPP services through distance learning is permitted through December 31, 2027.
- MDPP suppliers must apply for and receive MDPP supplier status prior to receiving reimbursement for MDPP services.
- MDPP suppliers must currently have either CDC Preliminary Recognition or CDC Full Recognition prior to applying.
Beneficiary Eligibility Criteria & Referrals
- Eligibility criteria:
- Are enrolled in Medicare Part B (for more information see CMS’s How to Verify an MDPP Beneficiary’s Medicare Coverage document);
- BMI ≥ 25; ≥ 23 if self-identified as Asian;
- A1c (HgA1c) between 5.7 and 6.4%, or a Fasting Plasma Glucose (FPG) test result of 110-125 mg/dL, or a 2-hour Post-Glucose Challenge Test result of 140-199 mg/dL (oral glucose tolerance test) within the previous 12 months;
- Have no previous diagnosis of type 1 or type 2 diabetes with the exception of a previous diagnosis of gestational diabetes; and
- Does not have end-stage renal disease (ESRD) at any point during the MDPP services period.
- The MDPP benefit is available for coverage only once per lifetime.
- Although referrals are not required, the following referrals are allowed, as long as blood test results indicate eligibility:
- Self-referral from participant
- Community referral
- Physician referral
- Other health care practitioner referral
Preventing Diabetes in Your Medicare Population Video: The AMA Ed Hub™ created a 4-minute overview for healthcare providers that explains Medicare DPP services, beneficiary eligibility, and the benefits of referring patients to the program.
Previously, the FPG test and the Post-Glucose Challenge Test were the only diabetes screening tests covered by Medicare, but under the CY 2024 Physician Fee Schedule (see section L), the HbA1c test is now also covered. All three of the diabetes screening tests are covered twice within the 12-month period following the date of the most recent diabetes screening test of an individual.
MDPP Supplier Eligibility & Enrollment
MDPP suppliers must 1) enroll under Medicare; and 2) have CDC full recognition or CDC preliminary recognition. For more information on full and preliminary CDC recognition see the Requirements for CDC Recognition.
- MDPP suppliers must also maintain at least one administrative location—a non-private residence—and a primary business telephone number.
- All “lifestyle coaches” (who are employed by an MDPP supplier) must obtain an NPI, which will be reported with Medicare claims:
- To be eligible to provide MDPP services, coaches may not have had Medicare billing privileges revoked or have been convicted of a felony within the last 10 years.
- Individual coaches cannot apply to be an MDPP supplier.
- Individual coaches should be compliant with the CDC Recognition Standards coach requirements.
- All CDC-recognized organizations must enroll in Medicare as MDPP suppliers to furnish and bill for MDPP services.
- Existing Medicare suppliers must enroll as MDPP suppliers to offer the program.
- If an MDPP supplier’s Medicaid billing privileges are revoked, Medicare billing privileges will also be revoked.
- MDPP suppliers must submit a roster of coach NPIs, names, and social security numbers upon application for enrollment.
- MDPP supplier enrollment began January 1, 2018.
More CMS resources for MDPP Supplier enrollment, located on the Center for Medicare and Medicaid Innovation MDPP site, include:
- MDPP Supplier Roadmap (Overview of the MDPP Supplier Journey)
- MDPP Enrollment (How to Prepare for Enrollment)
- CMS/CDC Roles Fact Sheet (Outlines Roles of CMS/CDC)
MDPP Orientation Video: Provides an overview of the MDPP for organizations interested in becoming suppliers.
Payment for MDPP Services
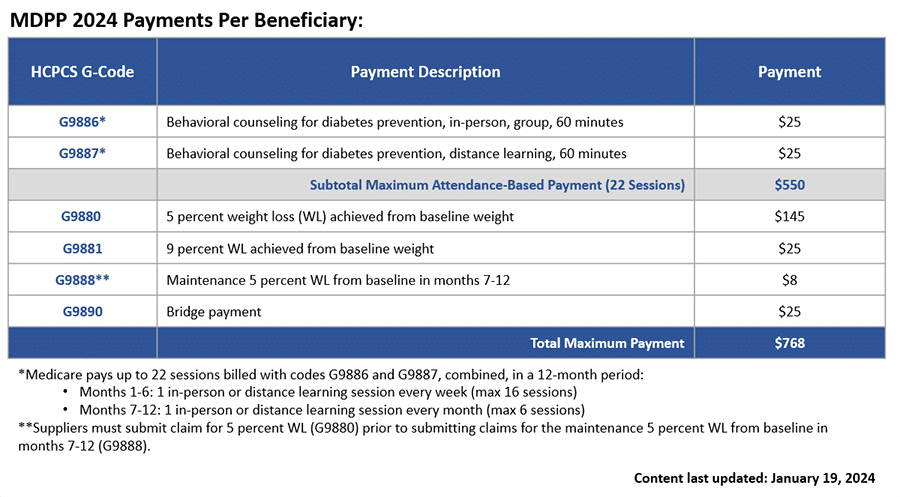
MDPP services are paid for using both a fee-for-service and performance-based payment methodology that is updated annually for inflation. Fee-for-service payments are issued for beneficiary attendance and performance-based payments are given based on beneficiary weight loss.
The following table details the CMS Calendar Year MDPP Payment Rates and the maximum reimbursement available per beneficiary:
Beneficiary Engagement Incentives
- If an MDPP supplier offers an in-kind incentive, the item or service must be provided during the MDPP services period and must have a reasonable connection to the CDC-approved curriculum.
- Cost of incentives must not be shifted to another Federal health care program or to a beneficiary.
- MDPP suppliers must maintain documentation of incentives that individually exceed $25 in retail value; incentives involving technology may not, in aggregate, exceed $1,000 in retail value for any one MDPP beneficiary.
Medicare Advantage Plans and the MDPP
All Medicare beneficiaries have access to MDPP services. There are two ways in which Medicare beneficiaries can receive these benefits:
- Through original Medicare, which is comprised of Part A (hospital services) and Part B (outpatient medical services), or
- Through Medicare Part C, also known as Medicare Advantage.
Original Medicare is administered directly by the federal government, and beneficiaries may receive care from any provider that accepts Medicare. Medicare Advantage (MA) provides Medicare benefits through approved private insurance companies, rather than directly through the federal government, and generally receive care from a specific network of providers. MA plans must provide enrollees with all Medicare Part A and Part B services, but they may also cover additional benefits, such as dental or vision care.
CMS has released guidance for Medicare Advantage plans, including an MA Fact Sheet and document that contains Medicare Advantage-related extracts from the MDPP Calendar Year 2018 Physician Fee Schedule Final Rule. For more information, visit the CMS MDPP website or see CMS MDPP Expanded Model Fact Sheet.
In addition to these resources, CMS, the National Association of Chronic Disease Directors (NACDD), and Leavitt Partners worked collaboratively to host an informational webinar on how MDPP suppliers can work with MA plans. An accompanying resource was developed that details the information presented during the webinar.
Additional Guidance
It is important to note that there are some aspects of the program that have not yet been finalized or that CMS is continuing to monitor. It is expected that additional guidance on these elements will be detailed in future rulemaking. Some of the policies that may be forthcoming include:
- Virtual delivery
- Program integrity safeguards
- Verification processes used by MDPP suppliers to determine whether beneficiaries have enrolled in the program in the past
- Application processes and ongoing technical support of MDPP suppliers
The short-term goal of the MDPP program is to help individuals lose at least five percent of their weight, with the longer-term goals of improved health and lower Medicare expenditures. See the report CMS released on the MDPP Expanded Model Findings at a Glance Evaluation of Performance April 2018 – December 2021 for more details.
If you have any further questions, please visit the MDPP Supplier Support Center.









