Commercial Payers → Fiscal Operations → Reimbursement Models for Commercial Payers
Reimbursement Models for Commercial Payers
The Information below about cost and reimbursement for the National Diabetes Prevention Program (National DPP) lifestyle change program can help commercial health insurance plans and employers anticipate the financial impact of covering the program. See the Cost and Value page for more information about analyzing the cost of covering the program. This Reimbursement page also outlines how the National DPP lifestyle change program can be accounted for in insurer’s Medical Loss Ratio calculation.
Costs
Organizations interested in delivering the National DPP lifestyle change program as a CDC-recognized organization can use the American Medical Association’s National DPP Lifestyle Change Program Budget Considerations Tool to estimate the cost of delivering the program.
Activities that drive program costs include marketing and recruitment efforts, facility fees, and direct program delivery costs such as staffing costs. For example, entities may need to hire staff, sign a lease for a facility, and make phone calls or send mailings to potential participants. Online program costs may differ. Online program providers incur significant development costs and then tend to have lower ongoing costs for delivering the program. Ongoing variable or per-participant costs for online program providers include the cost of digital scales that may be issued to participants at the outset for purposes of recording weight, as well as staffing costs.
The Budget Projection Template (click the icon to download) can be used by payers to estimate the total cost of covering the National DPP lifestyle change program for eligible members or employees, as well as the average cost per participant. The Commercial Budget Projection Template Instructions (click the icon to open) is meant to be used alongside the Budget Projection Template to help the user identify the decisions and data needed. It also explains how to interpret the results of the Budget Projection Template.
Costs in Practice
ADCES
The director of prevention at the Association of Diabetes Care and Education Specialists (ADCES) (formerly the American Association of Diabetes Educators (AADE)) estimates that the per-participant cost of delivering the program ranges from $250–$500 among successful ADCES program delivery sites. ADCES has been implementing the National DPP lifestyle change program within nationally certified diabetes self-management education and support (DSMES) programs (ADCES-accredited, ADA-recognized, and CDC-recognized) to deliver the National DPP lifestyle change program with oversight by Certified Diabetes Educators.
CMS OACT Report
The Centers for Medicare & Medicaid Services (CMS) Office of the Actuary (OACT) certification report published in March of 2016 referenced the cost incurred in providing the program by a large national carrier. Less than 10% of the participants were over 65.
“The evaluation of their program included results from the first 3 years of the intervention. The carrier spent nearly $200 per person, and the medical spending reductions were nearly that amount over the 3 years evaluated. Therefore, the DPP is expected to break even in program year 4. The spending reductions achieved for the participants aged 55 or older were slightly higher than the average for the entire group. In addition, the carrier noted that the savings were significantly higher for the participants who achieved the 5% weight-loss goal.”
For more information, see CMS OACT certification report or CDC’s Designing a Natural Experiment study.
YMCA
The YMCA program fee is $429 for the year-long program. Consumers pay in a variety of ways and YMCAs work with them if financial assistance is needed. Some payers pay the flat $429 fee regardless of how much of the program a participant completes. For claims-based reimbursement, a performance-based fee schedule is used, and payers pay claims based on the achievement of specific milestones. Average cost for the program is comprised of fixed and variable costs. When there are more participants in the program to absorb the fixed costs, the average cost can be substantially lower, but volume is key.
Under certain circumstances, individuals may be able to cover their portion of participation costs with their Health Savings Account (HSA). See the section titled Using HSA Dollars to Pay for the Program on the Case for Coverage for Commercial Plans and Employers page for more information
Reimbursement Models
To date, payers covering (or proposing coverage) of the National DPP lifestyle change program have provided reimbursement using one or a combination of the following methods:
- Fee-for-service: reimbursement on a per session basis
- Attendance Milestone: variable reimbursement provided after multiple sessions have been completed (e.g., 1st session, 4th session, 9th session, 16th session)
- Performance-based model: offering different reimbursement levels based on outcomes, such as weight loss and weight loss maintenance
- Combination: using a combination of the fee-for-service, attendance milestone, and/or performance-based models.
Reimbursement Models in Practice
Solera Health
Solera Health, a preventive care benefits manager, contracts with health plans and employers that cover the National DPP lifestyle change program. Solera uses a pay-for-performance reimbursement model, so claims are submitted for reimbursement at a series of milestones–typically upon enrollment, engagement at 4 weeks, engagement at 9 weeks, and 5% weight loss. Solera’s pricing applies to all community and digital CDC-recognized organizations at a single price point.
Omada
is a CDC-recognized organization that delivers the National DPP through an online format. Omada’s fees are outcome-based—the company charges a one-time enrollment fee when participants join the program, but following that payment, all revenue is dependent on achieving the clinical outcomes promised to partners.
Kentucky Employees’ Health Plan
The Kentucky Employees’ Health Plan, a self-funded plan for Kentucky’s public employees, pays CDC-recognized organizations that provide the National DPP lifestyle change program a fixed amount depending on the level of services provided, defined by three tiers. To help with start-up costs, 25% of the fee is paid after the participants have completed two classes in the first six months; the remaining 75% is paid after the fourth class has been completed.
- Tier 1—basic program, reimbursed at $350–$429 per enrollee
- Tier 2—basic program plus a year-long gym membership, reimbursed at $429 (only two CDC-recognized organizations are offering gym memberships)
- Tier 3—basic program plus additional services, reimbursed at a rate higher than $429
MDPP Expanded Model
The Medicare Diabetes Prevention Program (MDPP) expanded model allows Medicare beneficiaries to access evidence-based diabetes prevention services with the goal of a lower rate of progression to type 2 diabetes, improved health, and reduced spending. To learn more, please visit the Center for Medicare and Medicaid Innovation MDPP site. Additional information is also available on the MDPP Basics page of the Coverage Toolkit.
MDPP services are paid for using both a fee-for-service and performance-based payment methodology that is updated annually for inflation. The current payment rates can be found here: CMS Calendar Year MDPP Payment Rates.
Medical Loss Ratio
The National DPP lifestyle change program can be counted in the numerator of the Medical Loss Ratio (MLR) in most cases.
The Medical Loss Ratio is the percentage of an insurer’s premium dollars that is spent on medical care and quality improvement activities (e.g., chronic disease management, wellness programs, etc.). For example, if an insurer spends 85 cents of every premium dollar on medical care and quality improvement activities, its MLR is 85%. In most cases, the National DPP lifestyle change program should be able to be counted in the medical care or quality improvement activity component of that calculation.
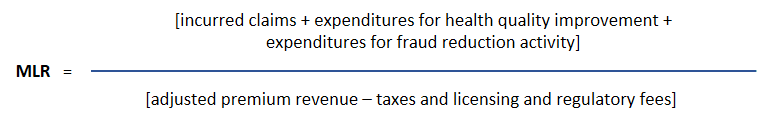
Under the Affordable Care Act, the Centers for Medicare & Medicaid Services (CMS) requires commercial individual and small group products to have at least 80% MLR and large group products to have at least 85% MLR. Self-funded insurance products, however, do not have a minimum MLR requirement. Self-funded products administered by an insurance company are also excluded from a minimum MLR requirement.
<!—for="" more="" information,="" see="" the="" MDPP Final Rule page.—>
<!–Note: The payments in this table were developed for a Medicare population, and may not reflect the costs of delivering the program to the Medicaid population. Data from the CDC cited in the CMS OACT certification report indicates that Medicare participants had a higher adherence rate (i.e., attend more classes on average) and had a higher rate of weight loss than younger age groups.
In CMMI’s proposed expansion of the model tested with the YMCA of the USA (Y-USA) DPP within Medicare, the CMS Office of the Actuary (CMS OACT) certification report referenced the following schedule of proposed payments. The schedule is driven both by outcomes and session attendance. The maximum year one reimbursement would be $450 for a given participant. The report assumed that CMS would, on average, pay $300 in year one for a given participant.
Note: the proposed MDPP payment schedule varies slightly from the table below and is not yet finalized. See the proposed payment schedule on the MDPP Final Rule page.
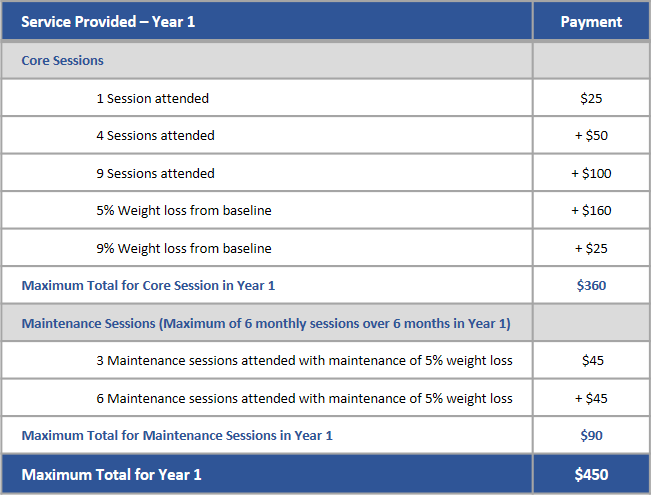
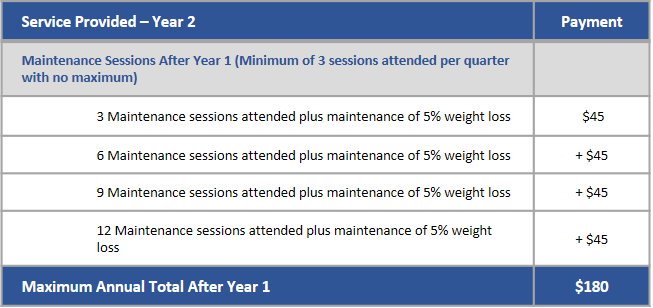
Table included in the CMS OACT certification report; reformatted for this site. See the CMS OACT certification report here.
Note: The payments in this table were developed for a Medicare population, and may not reflect the costs of delivering the program to the commercially insured population. Data from the CDC cited in the CMS OACT certification report indicate that Medicare participants had a higher adherence rate (i.e., attend more classes on average) and had a higher rate of weight loss than younger age groups.–>