Building Partnerships → Building Network Capacity
Building Network Capacity and Supporting CDC-Recognized Organizations
This page provides information and examples for how state Medicaid agencies and state health departments can assess the landscape and technical assistance needs of CDC-recognized organizations, expand the capacity of the state network through support of existing and recruitment of new organizations, help organizations develop business acumen skills for successfully engaging with payers, and explore options for providing third-party or collective administrative support (including but not limited to umbrella hub arrangements (UHAs)). Many of the state examples relate to Medicaid coverage of the National DPP lifestyle change program, yet the strategies and lessons learned may be applied more broadly.
This page is organized by the following topics:
- Expanding Roles of CDC-Recognized Organizations
- Network Access and Management Rules
- Network Capacity Assessment
- Increasing Network Capacity
- Providing Technical Assistance and Building Core Business Skills
- Administrative Support for CDC-Recognized Organizations
- Resources

Expanding Roles of CDC-Recognized Organizations
As the coverage landscape has expanded for the National DPP lifestyle change program it has increasingly become necessary for CDC-recognized organizations to take on financial and administrative responsibilities and engage with public and private payers in new ways. Likewise, it has become increasingly important that the network of CDC-recognized organizations is sufficient to ensure access to programs by individuals who have the National DPP lifestyle change program as a covered benefit through Medicaid, Medicare, a state employee health plan, or employer or commercial insurance.
State Support for Network Capacity
State Medicaid and public health may play important roles in supporting network capacity in their states, identifying and meeting the technical assistance needs of CDC-recognized organizations, and supporting engagement with payers. Federal Medicaid network access rules also require that states ensure adequate access to service providers, which in this case are CDC-recognized organizations (for more information, visit the Medicaid Agencies Network Management page on the Coverage Toolkit).
Roles of CDC-Recognized Organizations
Overall, CDC-recognized organizations’ functions have expanded from focused program delivery to include additional professional responsibilities that may include:
- Program and business administration
- Legal and regulatory requirements
- Business planning, forecasting, and managing supply and demand
- Revenue management
- Staffing, training, and ongoing education needs
- Funding (including sustainable reimbursement rates, innovative funding and alternative payment models, and start-up funding)
- Enrolling as a Medicaid enrolled provider and a Medicare Diabetes Prevention Program (MDPP) supplier (as applicable) and becoming credentialed with Medicaid managed care and Medicare Advantage plans
- Technology and data management
- Inclusion of online or distance learning delivery platforms
- Engaging with electronic health records and health information systems
- Network and referral coordination
- Regulatory and compliance management
- Data management including collection, analysis, reporting (including sending data to CDC’s Diabetes Prevention and Recognition Program (DPRP)), and evaluation
- Billing and reimbursement
- Contracting (including with managed care), Business Associate Agreements (BAA), Memorandums of Understanding (MOU), and Data Use Agreements (DUA)
- Navigating reimbursement systems, and billing and claims submission
- Marketing and communication
- Identifying and implementing strategies for reaching Medicaid beneficiaries, underserved populations, and priority populations
Network Access and Management Rules
Medicaid Network Access Rules
Within Medicaid, states must ensure adequate access to providers (i.e., CDC-recognized organizations). The “equal access provision” outlined in Title 42 of the Code of Federal Regulations (CFR) requires that state Medicaid reimbursement ensures that program enrollees have the same access to care that is available to the general population (42 CFR 447.204).
Additionally, states must monitor access to care through an access monitoring review plan. “The access monitoring review plan and analysis must, at a minimum, include: The specific measures that the state uses to analyze access to care such as, but not limited to:
- Time and distance standards,
- Providers participating in the Medicaid program,
- Providers with open patient panels,
- Providers accepting new Medicaid beneficiaries,
- Service utilization patterns,
- Identified beneficiary needs,
- Data on beneficiary and provider feedback and suggestions for improvement,
- The availability of telemedicine and telehealth, and
- Other similar measures…”. (42 CFR 447.203)
Medicaid Managed Care Network Management Rules
The Medicaid managed care rule finalized in April 2016 and updated in 2020 includes several provisions related to network management that will need to be followed when contracting with CDC-recognized organizations.
First, all MCO contracted providers (i.e., CDC-recognized organizations) are required to enroll with the state as Medicaid providers, even if they do not deliver services to Medicaid fee-for-service beneficiaries. As Medicaid enrolled providers, these organizations will need to comply with Medicaid program integrity rules such as confidentiality, screening, and disclosure standards.
Second, states must set a quantitative network adequacy standard for certain classes of provider types contracting with MCOs. States can choose which quantitative standard they use (e.g., minimum provider-to-enrollee ratios, maximum travel time or distance to providers, a minimum percentage of contracted providers that are accepting new patients, maximum wait times for an appointment, hours of operation requirements, or a combination of these quantitative measures). While CDC-recognized organizations are not one of the designated classes of providers subject to these standards, MCOs might consider using similar types of quantitative standards when developing their National DPP lifestyle change program networks.
Beyond state and federal rules, some key issues MCOs may want to consider when establishing a network of CDC-recognized organizations for the National DPP lifestyle change program include:
- Geographic dispersion to ensure adequate access and availability of programs;
- The data tracking processes and mechanisms to be used by the covered providers; Standards for claims submission processes; etc.
Commercial Network Standards
Nearly every state has flexible qualitative network adequacy standards such as requiring networks to be “sufficient in numbers and types of providers to assure that all covered benefits to covered persons will be accessible without reasonable delay.” For more information see Regulation of Health Plan Provider Networks.
However, more than half of states have also implemented objective quantitative tests of network adequacy. Common quantitative standards include:
- Maximum time and distance enrollees travel to access services
- Types of providers available to enrollees
- Maximum length of time enrollees wait for appointments for nonemergency services
- Ratios of providers to enrollees
Commercial plans, self-insured employers, and the CDC-recognized organizations they contract with to provide the program should be aware of all state network adequacy statutes and regulations in states where they operate. For quick reference, a summary of network adequacy standards developed by the National Conference of State Legislatures is available here (dated 02/01/2018).
Section 1311(c) of the Affordable Care Act (ACA) introduced federal network adequacy standards for individual market and small group commercial plans that are Qualified Health Plans.
Qualified Health Plans are required to have a provider network that:
- Includes essential community providers in accordance with 45 CFR 156.235;
- Maintains a network that is sufficient in number and types of providers, including providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay; and
- Is consistent with the network adequacy provisions of section 2707(c) of the Public Health Service Act.
A Center for Medicare & Medicaid Services (CMS) letter describing how this standard will be applied in 2017 is available here.
These federal rules serve as a “regulatory floor,” but states have the latitude to retain authority over enforcing network rules. Therefore, state network standards also apply to Qualified Health Plans.

Network Capacity Assessment
State-led efforts to build network capacity should begin with an assessment of current statewide capacity of CDC-recognized organizations. This may involve mapping the state landscape of programs, collecting general information on existing programs, and identifying any technical assistance needs of those programs.
State Landscape
An initial strategy for states in assessing network capacity may be to map or otherwise represent existing CDC-recognized organizations to show the number and location within a state. This information can be used to identify gaps according to different filters, such as areas with elevated diabetes prevalence and/or obesity, low socioeconomic levels, and at-risk populations. For example, the location of CDC-recognized organizations (shown for Minnesota in Figure 1 below) could be overlayed with other factors, such as adult diabetes prevalence (shown for Minnesota in Figure 2 below). States can use this information to guide decisions on where and how to prioritize support for new and existing CDC-recognized organizations.
A list of CDC-recognized organizations that is filterable by state, city, or organization can be found here.
Figure 1. Minnesota CDC-Recognized Organizations, 2019
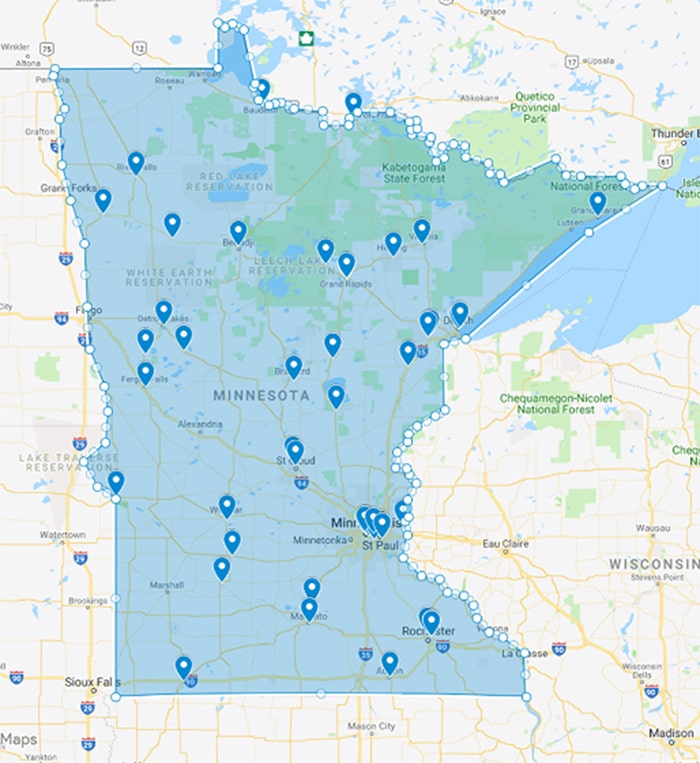
Figure 2. Minnesota Adult Diabetes Prevalence by County Overlayed
with National DPP CDC-Recognized Organization Sites, 2016
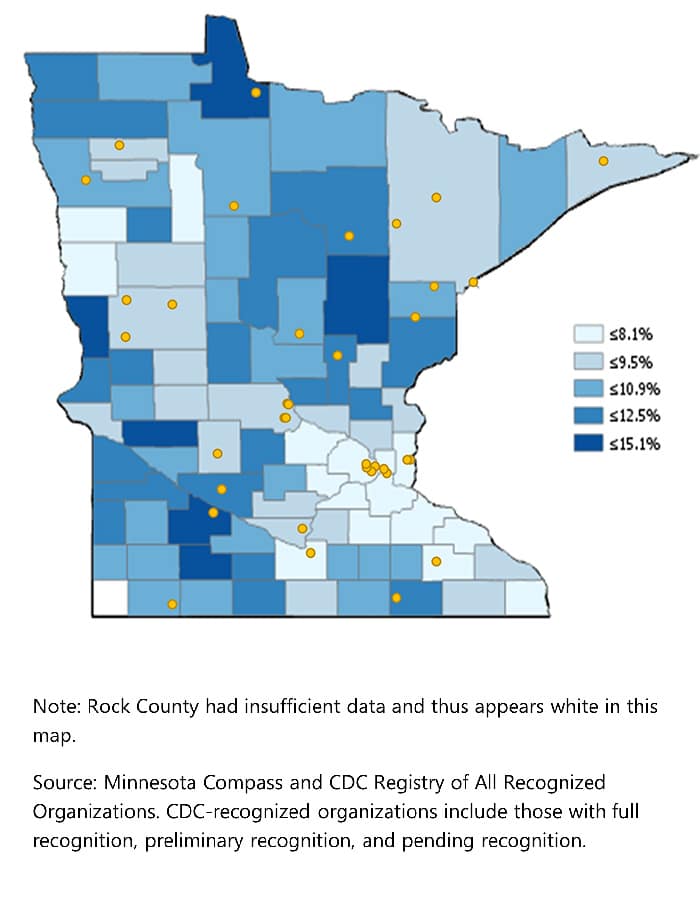
A useful resource to track and map state and local data can be the CDC’s United States Diabetes Surveillance System, an interactive web application that compiles diabetes data and trends at national, state, and county levels. The Surveillance tool provides estimates and trends of diabetes prevalence, risk factors, preventive care practices, and complications. The system also includes a Social Determinants of Health tool that provides county-level estimates of diabetes, physical inactivity, and obesity within the context of important social factors.
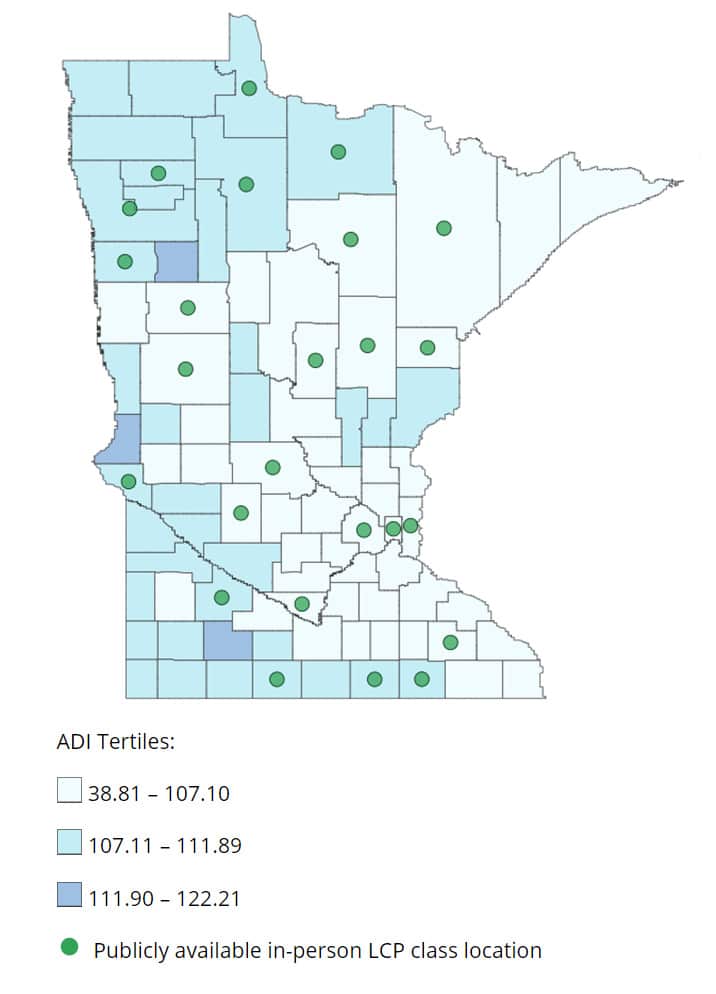
Study authors from the CDC’s Division of Diabetes Translation have published information regarding program availability by county-level diabetes incidence and by disadvantaged socioeconomic status. Disadvantaged status is measured using the Area Deprivation Index (ADI) score. According to CDC, “ADI is a geographic area-based measure of the socioeconomic disadvantage experienced by a community. The index uses various markers of socioeconomic status including level of education, housing value, family income, and unemployment status. High disadvantage is associated with a higher risk for poor health, as well as poorer health care outcomes.” For example, Figure 3 below shows the publicly available in-person National DPP lifestyle change program classes compared to the ADI Score in Minnesota. This article includes similar maps of the United States that can help assess the presence of publicly available National DPP lifestyle change program classes as of March 1, 2017. Organizations could use maps like these to understand the counties most in-need of new programs.
Figure 3: Publicly Available In-Person National DPP Lifestyle Change Program Classes Compared to ADI Score, 2017
Program Assessment
Beyond the statewide distribution of CDC-recognized organizations, it can be important to understand the realities of the different entities, including:
- Delivery mode (in-person, online, distance learning, or combination)
- Level of DPRP recognition (preliminary, pending, or full)
- Populations being served
- Language(s) for delivery and program materials (both current programming and capabilities)
- Program saturation (e.g., Do they find it difficult to fill classes or is there a wait list?)
- Capacity for expansion (through adding locations, classes, trained lifestyle coaches, language or cultural adaptations, or additional delivery modes)
- Billing/reimbursement mechanisms in place (such as managed care organizations (MCOs), Medicaid, or commercial/employer contracts)
- Access to bi-directional referral systems
- Technical assistance needs
It can also be helpful to identify MDPP suppliers within a state. This information can help states better understand how potentially sustainable their existing network is, and where to focus efforts on capacity building and expansion. To become an MDPP supplier, CDC-recognized organizations must enroll in Medicare and must have capabilities to submit claims to Medicare for reimbursement (these capabilities could be applied to other payer types).
- A list of current MDPP suppliers can be found here.
- A map of current MDPP suppliers by zip code or region is available here.
For more information about the MDPP, see the MDPP page of the Coverage Toolkit.
Technical Assistance Needs Assessments
To better understand the capacity and technical assistance needs of current CDC-recognized organizations, several states have conducted research through surveys, focus groups, barrier analyses, and other mechanisms. The identification of technical assistance needs helps states develop training opportunities, resources, ongoing communications, and support that states provide to CDC-recognized organizations. For additional information on providing technical assistance to CDC-recognized organizations, see the Providing Technical Assistance and Building Core Business Skills section below.
Surveys
Surveys can be a convenient way to learn more about the CDC-recognized organizations in the state. Surveys have the advantage that they can be administered remotely to a large number of organizations.
State Example
Maryland and Pennsylvania: Surveying CDC-Recognized Organizations
Both Maryland and Pennsylvania surveyed their CDC-recognized organizations to collect general information, assess current capacity, and gauge interest in offering the National DPP lifestyle change program to Medicaid beneficiaries.
- Maryland Survey for CDC-Recognized Organizations Offering Online Programs – This is the survey the Maryland Department of Health sent to online programs, but surveys were sent to in-person programs as well.
- Pennsylvania Survey for CDC-Recognized Organizations Interested in Offering the Program – This survey was sent to in-person, online, and combination programs in Pennsylvania. To develop the survey questions, Pennsylvania first conducted interviews with CDC-recognized organizations using the Pennsylvania Formative Interview Guide.
- Sample Survey for CDC-Recognized Organizations – This network capacity sample survey was adapted from a state example.
For more information on Maryland and Pennsylvania’s Medicaid coverage of the National DPP lifestyle change program, visit the Maryland Medicaid Demonstration Project and the Pennsylvania State Story of Medicaid Coverage pages of the Coverage Toolkit.
Focus Groups
Another approach to gathering information about technical assistance needs is by asking questions to a focus group. This approach gives the interviewer the opportunity to adapt questions and to ask follow-up questions. Focus groups can also allow responders to build on each other’s answers.
State Example
Colorado: Focus Group
Colorado held discussions with its CDC-recognized organizations and MDPP supplier network in early 2020 to gather input for the development of a National DPP Medicaid benefit in their state. The purpose of these stakeholder engagements was to ensure that Colorado’s benefit (anticipated 2021) is constructed in a way that supports provider uptake. The Colorado Focus Group Questions asked the CDC-recognized organizations about:
- Current populations served
- Referral requirements
- Provider types
- Medicaid enrollment technical assistance needs
- Additional considerations for the development of the Medicaid National DPP benefit
Barrier Analysis
Barrier Analysis is a model used to identify root causes of a particular behavior or trend in order to develop effective social and behavioral change messages, strategies, and activities to address positive change or uptake.
State Example
California: Barrier Analysis
California conducted a barrier analysis in the process of planning for Medicaid coverage of the National DPP lifestyle change program. This barrier analysis was an in-depth look at potential challenges California might face during implementation of the program. Most notably, the analysis identified perceived barriers for CDC-recognized organizations and managed care plans (MCPs), including:
- Perceived barriers for CDC-recognized organizations
- Lack of knowledge of the Medi-Cal (California Medicaid) National DPP lifestyle change program benefit
- Background check/fingerprint requirements
- Low reimbursement rates
- Invoice system infrastructure
- Perceived barriers for MCPs
- Questions about the policy guidance for MCPs
- How MCPs can offer the benefit by achieving CDC-recognition
- Concerns around audits and investigations
- Low reimbursement rates
For more information onCalifornia’s Medicaid coverage of the National DPP lifestyle change program, visit the California State Story of Medicaid Coverage page of the Coverage Toolkit.

Increasing Network Capacity
Based on the findings from a state’s landscape and organizational assessments, it may be determined that additional CDC-recognized organizations are needed to expand the state’s network footprint, engage with payers, and provide adequate access to participants across locations and program types. A state’s network of CDC-recognized organizations can be expanded by recruiting new organizations to become CDC-recognized, creating a new Medicaid enrolled provider type for CDC-recognized organizations, and expanding the network of payers covering the National DPP lifestyle change program.
Recruiting New Organizations
In order to bolster network capacity, states may want to consider targeting and recruiting specific entities or members of certain professions to become CDC-recognized and deliver the National DPP lifestyle change program (or affiliate with existing programs). Many licensed providers are likely already engaging with payers and may have an interest in, infrastructure for, and ability to expand program delivery to include the National DPP lifestyle change program. Examples include:
- Medicaid enrolled providers (depending on the state, will include many of the following)
- Accountable care organizations (ACOs)
- Diabetes Self-Management Education and Support (DSMES) programs
- Chronic-disease focused programs (such as hypertension, asthma, HIV)
- Licensed professionals, including registered dietitians (RD), registered nurses (RN), certified diabetes care and education specialists (CDCES), physical therapists, and chiropractors
- Pharmacists
- Community health workers (CHW)
- MCOs
- Health care systems and hospitals
- Wellness clinics or health clubs
- Local public health departments
- Federally Qualified Health Centers (FQHC)
- Area Agencies on Aging (AAA)
- Community-based organizations (CBOs), such as YMCAs
- Colleges, universities, and institutes for higher education
Additional information about some of these groups is provided below.
State Example
New Jersey: Identify Existing Medicaid Providers in the State
In 2019, New Jersey had 21 CDC-recognized organizations in the state. To enable access for Medicaid beneficiaries who could benefit from the program and allow MCOs to achieve network adequacy, the state identified currently enrolled Medicaid providers who could deliver the program. The state has engaged in a variety of activities to identify Medicaid enrolled providers, including:
- Cross-walking the CDC’s DPRP online directory of CDC-recognized organizations with New Jersey Medicaid’s enrolled provider list
- Leveraging resources within New Jersey’s 211 (essential community services hotline)
- Engaging MCOs
- Outreaching to provider associations such as the Association of New Jersey Chiropractors
- Contacting YMCAs
To organize this effort and track the information gained, New Jersey created a spreadsheet to catalogue existing Medicaid providers who already are CDC-recognized organizations or are interested in becoming CDC-recognized organizations.
New Jersey also procured a Geographical Information System (GIS) that has the capability to perform pre/post data comparison of network capacity, map claims and utilization within the existing network of Medicaid enrolled providers, and identify gaps in CDC-recognized organizations.
Accountable Care Organizations
Accountable care organizations (ACOs) are groups of providers who are responsible for the cost and quality outcomes of a defined population of patients. ACOs and other types of alternative payment arrangements (also called value-based payment arrangements) are meant to reward health care providers for keeping patients healthy. Given these incentives, ACOs can be important partners in the effort to advance the National DPP lifestyle change program by becoming CDC-recognized and delivering the program, making referrals to existing programs, or becoming champions of type 2 diabetes prevention within their networks.
More information can be found on the How to Engage ACOs in the National DPP Lifestyle Change Program page of the Coverage Toolkit.
DSMES Programs
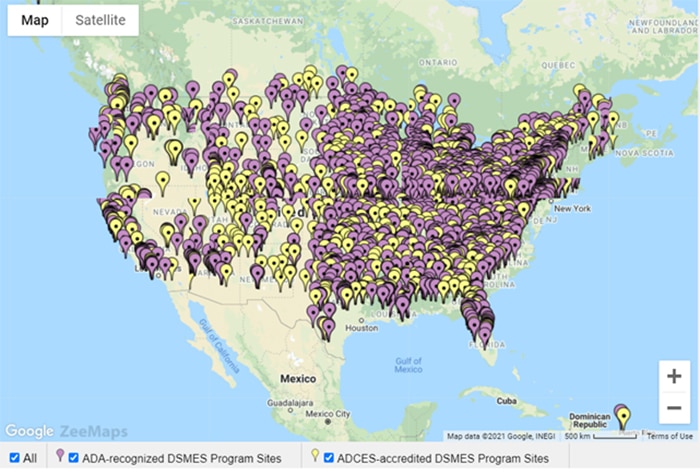
Diabetes Self-Management Education and Support (DSMES) programs may be a key resource for expanding the network of CDC-recognized organizations in many states, as there is significant geographic coverage of existing locations across the United States. These programs are also generally equipped to handle systems such as privacy compliancy, data sharing, and billing, and have an intact program infrastructure with coordinators and staff (who could potentially be trained as lifestyle coaches).
DSMES programs are often linked into physician referral systems and may already be connected to potential participants. They are also well-positioned to transition potential or existing participants who are identified as having type 2 diabetes (either before, during, or after participating in the National DPP lifestyle change program) to appropriate alternative services.
Both the Association for Diabetes Care and Education Specialists (ADCES) and the American Diabetes Association (ADA) share information about their accredited and recognized programs with CDC, and that data informs the map on ADCES’ website ADCES’ website. The map is searchable and updated quarterly with CDC data from both organizations. Figure 4 below identifies each ADA-recognized and ADCES-accredited DSMES program site in the mainland US as of January 1, 2021.
Figure 4: ADA-Recognized and ADCES-Accredited DSMES Program Sites, 2021
Licensed Professionals
Licensed professionals, including registered dietitians (RDs), registered nurses (RNs), certified diabetes care and education specialists (CDCES), physical therapists, and chiropractors, may share many of the same advantages as DSMES programs, especially related to familiarity with reimbursement systems and access to populations at high risk for type 2 diabetes.
To learn more about the roles of licensed professionals in delivering the National DPP lifestyle change program in Medicaid, see the Determining the Medicaid Enrolled Provider Type page of the Coverage Toolkit.
State Example
Wyoming: Piloting the National DPP Lifestyle Change Program in Medicaid Using Registered Dietitians
Wyoming Medicaid began a pilot in early 2020 to reimburse RDs delivering the National DPP lifestyle change program to Medicaid beneficiaries. RDs were already Medicaid enrolled providers in the state, allowing them to submit for reimbursement without making broader systems changes. Through a strong partnership between Medicaid and public health, the state agencies worked to partner RDs in the state to CDC-recognized organizations to oversee and deliver the program to Medicaid beneficiaries.
Pharmacists
Pharmacists may also be helpful in promoting and delivering the National DPP lifestyle change program and engaging with payers. The CDC has compiled resources for pharmacists to promote engagement in the program. The CDC has also released an Action Guide that includes case studies and promotes pharmacist participation on three tiers: promoting awareness; screening, testing, and referral; and delivering the program. To learn more, visit the Engaging Pharmacists page of the Coverage Toolkit.
Community Health Workers
A community health worker (CHW, also known as promotores and promotoras de salud, community health representatives, and community health advisors) is a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community they serve. CHWs are generally non-licensed health workers; however, some state agencies certify them through accredited CHW training programs. CHWs may be trained on the National DPP lifestyle change program curriculum and become Medicaid-enrolled providers (if allowed through state rules) or affiliate with Medicaid-enrolled providers.
To learn more about CHWs, see the Use an Existing Provider Type that Becomes or Affiliates with a CDC-Recognized Organization page of the Coverage Toolkit. Additionally, for more information on which states allow Medicaid reimbursement of CHW services through state rules see the interactive map on the National Academy for State Health Policy (NASHP) website.
State Example
Minnesota: Working with CHWs
In Minnesota, CHWs may deliver the National DPP lifestyle change program as part of the state’s Medicaid benefit. To qualify for Medicaid reimbursement, CHWs must work under the supervisions of specific Medicaid enrolled provider types, have valid certification, be affiliated with a CDC-recognized organization, and be trained as a lifestyle coach.
For more information on Minnesota’s Medicaid coverage of the National DPP lifestyle change program, visit the Minnesota State Story of Medicaid Coverage page of the Coverage Toolkit.
Managed Care Organizations
MCOs may become CDC-recognized and deliver the National DPP lifestyle change program directly to their members. MCOs can identify members with prediabetes or who are at high risk for type 2 diabetes, use established communication channels to outreach to their members about the program, and track referral and program outcomes through their internal systems.
State Example
Oregon: Working with Coordinated Care Organizations
The Oregon Health Authority created an implementation guide for coordinated care organizations (CCOs) that includes considerations for CCOs seeking to become CDC-recognized organizations (see pages 21-22 and Appendix A).
For more information on Oregon’s Medicaid coverage of the National DPP lifestyle change program, visit the Oregon Medicaid Demonstration Project page of the Coverage Toolkit.
Health Care Systems and Hospitals
Health care systems and hospitals are also uniquely positioned to help build state capacity for the National DPP lifestyle change program, increase patient engagement, and engage with payers. These facilities can become CDC-recognized and offer classes taught by hospital-employed lifestyle coaches at the hospital and affiliated sites. Many hospitals already offer DSMES classes and may cross-train registered nurses, dietitians, nutritionists, health educators, or CHWs to be lifestyle coaches and deliver the program.
Hospitals and health care systems can also contract with a local CDC-recognized organization and host classes at the hospital or at affiliated sites. This may help expand an organization’s reach as well as shift administrative responsibilities from a community-based organization to a hospital system. Hospitals can also act as a referral hub in their community and refer patients to available National DPP lifestyle change programs.
State Example
Maryland: Integrating the National DPP Lifestyle Change Program into Hospitals and Health Systems
The Maryland Department of Health, as part of their work in the CDC’s 6|18 Initiative, created a document entitled, Shared Learnings for Integrating the National DPP into Hospitals and Health Systems, which includes information about capacity building, recruitment and referrals, provider engagement, National DPP lifestyle change program implementation and data sharing, and payer reimbursement.
For more information on Maryland’s Medicaid coverage of the National DPP lifestyle change program, visit the Maryland Medicaid Demonstration Project page of the Coverage Toolkit.
FQHCs
FQHCs are comprehensive, community-based primary care providers that offer affordable care in areas with high need for health care. Their location in communities and their accessibility to patients makes FQHCs good candidates to deliver the National DPP lifestyle change program to their patient populations.
FQHCs receive payment and support from Medicaid, Medicare, private insurance, self-pay, Health Resources and Services Administration (HRSA) grants, and a variety of other grant funding sources.
FQHCs are reimbursed by Medicaid using an encounter-based prospective payment system (PPS), which is calculated on a per-visit basis and is designed to cover all qualifying services and supplies provided during the visit. For states that have established Medicaid coverage for the National DPP lifestyle change program, reimbursement of the program would either be rolled into existing FQHC PPS rates, or it would be reimbursed separately (i.e., FQHCs would bill the Medicaid agency directly for the service under a separate billing code).
Additionally, MCOs have more flexibility in how they pay for FQHC services; however, plans are required to pay FQHCs at least what they would pay non-FQHC providers in their network for the same medical services. If total MCO payments to an FQHC are less than what the center would have been paid under the PPS, the state Medicaid agency must pay the difference.
For additional information on Medicaid and Medicare reimbursement of FQHCs delivering the National DPP lifestyle change program, including state examples, see the Engaging Federally Qualified Health Centers page of the Coverage Toolkit and the FQHCs: Medicaid and Medicare Reimbursement for the National DPP Lifestyle Change Program document.
Creating a New Medicaid Enrolled Provider Type
For states that have established or are pursuing Medicaid coverage for the National DPP lifestyle change program, creating a new Medicaid enrolled provider type for CDC-recognized organizations may be another route to expand network capacity. Creating a new provider type for community-based organizations allows these entities to enroll and receive reimbursement from Medicaid directly. This may in turn foster sustainability for the benefit and potentially lead to increases in both the number of CDC-recognized organizations in a state as well as their ability to engage with various payers.
More information can be found on the Determining the Medicaid Provider Type page of the Coverage Toolkit.
Expanding the Network of Payers
As a means of supporting the sustainability of CDC-recognized organizations, states may also play a role in expanding the number of payers covering the National DPP lifestyle change program. State public health departments can engage Medicaid agencies and identify and outreach to employers and private payers within the state to make the case for coverage and support program implementation.
Resources to support states’ efforts around increasing coverage include:
- Case for Coverage for Medicaid and the Case for Coverage for Commercial Plans and Employers pages of the Coverage Toolkit: provide resources including targeted information, presentation templates, and handouts that can be used by CDC-recognized organizations to make the case for covering the National DPP lifestyle change program.
- Policy to Payment Roadmap: highlights activities that lead to coverage and operationalization of the National DPP lifestyle change program. The intended audiences for this resource are state Medicaid agencies and state public health departments, and it can serve as an informational resource for CDC-recognized organizations, MCOs, and health care providers.
- Project Management Tool (PMT): can be used when setting strategy and developing processes to achieve employer coverage of the National DPP lifestyle change program. The PMT is intended to capture critical steps to help move employers toward coverage, assign team members to tasks, provide a timeline for action, and track progress on steps for reporting. A Project Management Tool User Guide has been created to help navigate the PMT.
- Employer Slide Library: an editable resource intended for use when presenting to employers that are considering adding the National DPP lifestyle change program as a covered benefit for their workforce. An Employer Slide Library User Guide has been created to help navigate the slide library.

Providing Technical Assistance and Building Core Business Skills
Based on findings from technical assistance needs assessments and other communication with CDC-recognized organizations, state public health departments and other stakeholders may develop strategies to provide technical assistance directly to CDC-recognized organizations or through the development of supportive resources and facilitating engagement with payers. This technical assistance may target certain geographical locations, demographics, types of programs, or specific topics.
The technical assistance may consist of:
- Creating and providing guidance and resources related to the National DPP lifestyle change program as a covered benefit
- Linking CDC-recognized organizations to payers
- Helping CDC-recognized organizations engage with and make the case for coverage to payers
- Providing guidance and templates for managed care contracting and credentialing
- Outlining strategies for enrollment, recruitment, and retention
- Assisting with Medicaid provider enrollment
- Data and technology processes and regulations
- Financial planning, management, and sustainability
- Supporting peer-to-peer engagement among CDC-recognized organizations to promote shared learnings around recruitment and retention and other priorities
- Providing lifestyle coach training and assistance for organizations seeking to become CDC-recognized
Training and Resources
State-Specific Technical Assistance and Guidance
Many states convene CDC-recognized organizations and other interested parties to provide guidance and technical assistance related to the National DPP lifestyle change program, becoming a Medicaid-enrolled provider, and engaging with payers. In addition, states often create online resources and websites to house information related to the program and associated benefits.
California
State Example
California: Partnering to offer Medi-Cal DPP Benefit
The California Department of Public Health (CDPH) held a webinar in May 2019 that described how to partner with other organizations to offer the Medi-Cal (California’s Medicaid agency) DPP benefit. CDPH sent letters to existing CDC-recognized organizations and DSMES programs to invite them to the webinar and sent out an FAQ to attendees with responses to questions afterwards.
For more information on California’s Medicaid coverage of the National DPP lifestyle change program, visit the California State Story of Medicaid Coverage page of the Coverage Toolkit.
Maryland
State Example
Maryland: Supplemental Guidance for Becoming and National DPP Provider
The Maryland Department of Health (MDH) created a supplemental guidance document to assist new CDC-recognized organizations with applying to become a National DPP provider in Medicaid. A webinar was also held to go over the guidance document, which is linked to on the HealthChoice Diabetes Prevention Program website along with a program manual and FAQ updates.
MDH also held a business plan training workshop for CDC-recognized organizations and their fiscal staff. The training focused on creating strategies, objectives, and action plans to help with marketing, recruiting, and retaining participants in the National DPP lifestyle change program. Participants developed draft business plans and learned about implementation and monitoring strategies.
For more information on Maryland’s Medicaid coverage of the National DPP lifestyle change program, visit the Maryland Medicaid Demonstration Project page of the Coverage Toolkit.
Minnesota
State Example
Minnesota: Supporting Lifestyle Coaches with Strategies to Increase Enrollment and Retention
NACDD, Leavitt Partners, and the Minnesota Department of Health partnered to compile evidence- and experience-based practices on recruitment, enrollment, and retention into a single Best Practices Guide. The guide is written for lifestyle coaches and program coordinators who serve low income, Medicaid-eligible participants. However, many of the principles discussed in the guide could be used by any stakeholder working to increase recruitment, enrollment, and retention in the National DPP lifestyle change program and would apply to all eligible participants. For more information on the guide and strategies to increase retention, see the Retention page of the Coverage Toolkit.
The Minnesota Department of Health has also created a series of short videos to accompany the guide and help lifestyle coaches, program coordinators, and other individuals increase participation in their National DPP lifestyle change programs. The videos include:
- MN National Diabetes Prevention Program Best Practices Guide – Hennepin Health. This short video explains how Hennepin Health has integrated community health workers and healthy food boxes into their National DPP lifestyle change program.
- MN National Diabetes Prevention Program Best Practices Guide – Recruiting Participants. This short video covers some effective strategies for recruiting participants into the program.
- MN National Diabetes Prevention Program Best Practices Guide – Keeping Participants Engaged. This short video provides strategies for engaging participants.
- MN National Diabetes Prevention Program Best Practices Guide – Lifestyle Coaches. This short video covers strategies for selecting and training lifestyle coaches.
For more information on Minnesota’s Medicaid coverage of the National DPP lifestyle change program, visit the Minnesota State Story of Medicaid Coverage page of the Coverage Toolkit.
New York
State Example
New York State Story: Engaging CDC-Recognized Organizations in the Medicaid Benefit
The New York State (NYS) Medicaid program, in collaboration with the Department of Health’s (DOH) Office of Public Health’s Bureau of Community Chronic Disease Prevention, provided training and resources relative to Medicaid’s implementation and coverage of the National DPP benefit via a statewide kick-off webinar that was held on November 13, 2019. The webinar provided an overview of the new Medicaid National DPP lifestyle change program structure and covered topics such as: Medicaid National DPP program structure, Medicaid eligibility requirements, provider enrollment pathways, program reimbursement structure and amounts, and various resources.
NYS intends to continue to conduct additional National DPP collaborative outreach in order to:
- Increase providers’ knowledge and awareness of Medicaid’s coverage of the National DPP lifestyle change program.
- Educate current and potential Medicaid National DPP lifestyle change program delivery organizations about becoming a NYS Medicaid service provider.
For more information on New York State’s Medicaid coverage of the National DPP lifestyle change program, visit the New York State Story of Medicaid Coverage page of the Coverage Toolkit.
Oregon
State Example
Oregon: Medicaid Benefits National DPP Companion Guide
The Oregon Health Authority (OHA) developed the 2023 Companion Guide for Coordinated Care Organizations and Oregon Health System Partners Serving Oregon Health Plan Members to provide technical and policy direction for implementation and address commonly asked questions. This guide provides general information on the National DPP lifestyle change program in Oregon, describes pathways to implementation through coordinated care organizations (CCO), provides a review of Oregon’s benefits, and details funding methodologies.
OHA also conducted a 3-part webinar series for managed care, clinics, and community-based organizations to support improved network capacity and uptake of the National DPP lifestyle change program. The webinars included information on how to leverage key partnerships to improve network capacity, contracting with CCOs, overcoming barriers to program implementation and referrals, and engaging Medicaid beneficiaries in the National DPP lifestyle change program. The webinars and slides are available here (scroll down to the “National Diabetes Prevention Program” section of the page).
For more information on Oregon’s Medicaid coverage of the National DPP lifestyle change program, visit the Oregon Medicaid Demonstration Project page of the Coverage Toolkit.
Pennsylvania
State Example
Pennsylvania: Engaging CDC-Organizations
Pennsylvania held a webinar in October 2020 to engage CDC-recognized organizations around their benefit and walk them through the process of enrolling in Medicaid. Their 120-minute webinar also featured panel discussions with CDC-recognized organizations already enrolled with Medicaid and contracting with MCOs in Pennsylvania to deliver the lifestyle change program.
For more information on Pennsylvania’s Medicaid coverage of the National DPP lifestyle change program, visit the Pennsylvania State Story of Medicaid Coverage page of the Coverage Toolkit.
National Resources
There are abundant online resources to support CDC-recognized organizations that have been made available through CDC and its partners in the National DPP. Listed below are a selection of resources that directly relate to coverage and engaging with public and private payers that may be shared with partners by state public health departments and Medicaid agencies or used to develop state-specific resources.
CDC’s Customer Service Center
The CDC has many available resources through their National DPP Customer Service Center (CSC) to support CDC-recognized organizations engaging with payers.
- The Working with Employers and Insurers Guide provides information for CDC-recognized organizations on recruiting, engaging, and retaining people with prediabetes who have health insurance coverage into their programs. This guide also includes information on different types of insurance plans and guidance for reaching employers and insurers.
CSC also has resources on covering the National DPP lifestyle change program as a wellness/insurance benefit, and promotional materials for employers and insurers.
National DPP Coverage Toolkit
NACDD and Leavitt Partners have created the following resources, which are intended to support MCOs, CDC-recognized organizations, and referral organizations around Medicaid coverage of the National DPP lifestyle change program. These documents can be tailored to include state-specific information.
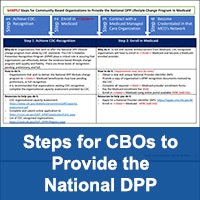
- Steps for Community-Based Organizations to Provide the National DPP Lifestyle Change Program in Medicaid: A visual overview for achieving CDC-recognition, enrolling in Medicaid, contracting with MCOs, and becoming credentialed in an MCO’s network. This document provides CDC-recognized organizations that are new to interacting with Medicaid and MCOs with a clear guide for the steps they need to take to receive Medicaid reimbursement for delivering the program to Medicaid beneficiaries.
- Tips for Contracting with Medicaid Managed Care Organizations: A two-page document that lists tips for community-based organizations that wish to contract with Medicaid MCOs.
- Self-Reflection and Capacity Discussion Questions: This document can primarily be used in two ways: (1) As a self-reflection exercise for CDC-recognized organizations, MCOs, referral organizations, and organizations in the delivery planning process to assess their own organizational capacity to support the National DPP lifestyle change program. (2) As a tool to generate discussions between different types of organizations; for example, a CDC-recognized organization could begin a conversation with an MCO by asking the MCO the questions listed in the MCO section.
Additional pages of the Coverage Toolkit that may be of use include:
- The MCO Contracting with CDC-recognized Organizations page, which contains sample language for common contract elements in contracts between MCOs and CDC-recognized organizations.
- The Commercial Payer Contracting with CDC-recognized Organizations page, which contains sample language for common contract elements in contracts between commercial payers and CDC-recognized organizations.
- The Data, Reporting, and Evaluation page, which describes the types of data involved with the National DPP lifestyle change program and the processes and protocols by which that data is shared among parties.
American Medical Association
The American Medical Association (AMA) also has many resources on their Prevent Diabetes website to support health care providers and CDC-recognized organizations. For example, AMA offers a budget considerations tool for health care organizations or CDC-recognized organizations considering delivering the National DPP lifestyle change program. The AMA website also includes other helpful resources such as a sample business associate agreement and CPT code guidance.
Linking Organizations with Payers
Another role that state Medicaid and public health agencies can play in supporting CDC-recognized organizations is connecting them to payers (both public and private). This can be done by disseminating contact information of eligible CDC-recognized organizations to payers, identifying payers that cover the National DPP lifestyle change program, and by hosting virtual or in-person platforms to allow these connections to be established.
Hawaii
State Example
Hawaii: Health Plan Engagement
In Hawaii, the state health department engaged a large health plan operating in the state that had recently announced coverage of the program. With support from NACDD, the state brought together the health plan and a local CDC-recognized organization to discuss program specifics and walk through the components of operationalizing coverage. As part of this meeting, the partners explored resources on the Coverage Toolkit, shared lessons learned from national payers, and outlined ways that the state could support the health plan’s efforts.
Maryland
State Example
Maryland: “Meet and Greets”
The Maryland Department of Health (MDH) brings together the state’s MCOs on a regular basis to introduce them to in-person and virtual Medicaid-enrolled CDC-recognized organizations. These “meet and greet” sessions allow Medicaid-enrolled CDC-recognized organizations to showcase their National DPP lifestyle change programs to the Medicaid MCOs and make the case for why the MCOs would want to contract with their organization. After these sessions, Medicaid-enrolled CDC-recognized organizations and MCOs have the necessary information and points of contact to pursue contracting with each other.
For the “meet and greets,” CDC-recognized organizations prepare slides that highlight their National DPP lifestyle change programs. CDC-recognized organizations’ presentations often feature:
- Organization mission, leadership, and staff
- Delivery modalities for the National DPP lifestyle change program
- Expertise delivering to specific populations (e.g., African American males, immigrant populations, low education populations, etc.)
- Program statistics (e.g., enrollment, retention, and weight loss)
- Recruitment and enrollment strategies
- Data collection and billing capabilities
For more information on Maryland’s Medicaid coverage of the National DPP lifestyle change program, visit the Maryland Medicaid Demonstration Project page of the Coverage Toolkit.

Administrative Support for CDC-Recognized Organizations
There is also continued momentum for exploring and establishing models in which CDC-recognized organizations partner with other entities to share or offload administrative responsibilities. Administrative support functions can be supported through collaboration with third-party organizations, coordination of umbrella hub arrangements, or facilitation of delivery-only models.
Third-Party Organizations
CDC-recognized organizations may benefit from collaborating with a third-party organization that can assist with the administration of the National DPP lifestyle change program and other chronic disease prevention and management programs. Third-party organizations can be national or local entities that provide outsourced specialized services to community-based organizations, health care providers, and payers. These organizations may offer expertise and scale to groups of CDC-recognized organizations, providing functions such as claims processing and billing, data and reporting, eligible participant lists, and referral management. Existing entities that offer similar services include:
- UHAs: see next tab
- Community care hubs (CCH): CCHs are community-focused entities that organize and support networks of CBOs providing services to address health-related social needs (HRSN) by contracting with health care organizations, performing payment operations, managing referrals, ensuring service delivery fidelity and compliance, and providing technology, information security, data collection, and reporting. The U.S. Administration for Community Living (ACL) is supporting this developing model in collaboration with CDC and CMS. For more information, read the Department of Health and Human Services’ Community Care Hubs: A Promising Model for Health and Social Care Coordination.
- Third-party administrators (TPA): TPAs are typically defined as companies that administer self-funded employee benefit plans (such as health welfare, workers’ compensation, and retirement plans) on behalf of an employer or health plan sponsor.
- Management service organizations (MSO): organizations that provide services to providers, which may include claims processing; electronic health record management; fiscal management; referrals and participant identification; human resources; contract management; operations; data, reporting, and analytics; and sometimes clinical, social, and behavioral health program supports.
- Administrative services organizations (ASO): organizations that generally provide payroll, employee benefits, human resource guidance, and workers’ compensation insurance coverage.
- Provider integrators: a new term describing an organization serving to connect health systems, payers, patients or members, and CDC-recognized organizations.
Third-party organizations can assist CBOs offering the National DPP lifestyle change program in meeting administrative and programmatic needs, including:
- Verification of billing and claims-based reimbursement by public and commercial insurers
- Support in achieving CDC-recognition and managing MDPP supplier regulations
- Contracting and negotiation support
- Data collection, analysis, storage, security, management, and submissions
- Legal support on HIPPA and HITECH; data use agreements
- Multi-partner convening, governance, and technical support
- Plan member identification; recruitment and secure referral of at-risk individuals
State Example
Illinois: Assessing the Role of Third-Party Organizations
To better understand the landscape of third-party organizations serving CBOs in Illinois, the Illinois Public Health Institute (IPHI), NACDD, and Leavitt Partners conducted a series of interviews with third-party organizations providing services to CBOs, more traditional health care providers, and payers. Findings from these interviews identified key functions that need to be established between CBOs and MCOs to cover chronic disease prevention and management programs in Illinois. These functions included legal, data, financial, certification or credentialing, contract and network building, and network coordination and referral.
Findings from the interviews also indicated that there are practices a third-party organization may want to incorporate to improve its ability to meet the needs of Illinois’ CBOs and, in turn, its overall success in the market. These practices include using a high-touch approach with organizations; having the ability to provide knowledge, time, and resources; maintaining a sense of mission for the work; establishing access to start-up funds; and maintaining diversification of services.
Umbrella Hub Arrangements
The CDC has also created UHAs, which allow CDC-recognized organizations to partner with a lead organization, also known as the umbrella hub organization or UHO, to form an arrangement for the purposes of obtaining sustainable reimbursement from payers and sharing the infrastructure costs needed to scale the National DPP lifestyle change program. This concept stems from the discussion earlier on this page capturing the many ways in which CDC-recognized organizations’ roles are expanding, including organizations having to develop and expand business skills; utilize technology in new ways; enroll, contract, and credential with payers; and engage in communication and marketing campaigns. UHAs are intended to allow CDC-recognized organizations to receive support for these new responsibilities. Additionally, UHAs may serve to increase CBOs’ attractiveness to payers that may prefer to enter into a single contract with a network of CDC-recognized organizations rather than many different contracts with separate organizations. UHAs are also encouraged to engage a range of organizations offering different services and programs including but not limited to the National DPP lifestyle change program.
To learn more, see the Umbrella Hub Arrangements page of the Coverage Toolkit.
Delivery-Only Models
Another consideration when working with a range of organizations is the potential for orchestrating “delivery-only” models. In a delivery-only model, a community-based organization or program has a relationship with a provider in which the CDC-recognized organization is only responsible for the delivery of the program, and the provider is responsible for the administrative responsibilities (such as recruitment, referral, reimbursement, data collection, reporting, etc.).
An example of a delivery-only model could be a YMCA contracting with a larger health system, in which the YMCA is responsible for delivering the program, while the health system assumes a range of administrative responsibilities. This would minimize the need for an organization to take on significant technological, financial, and administrative responsibilities associated with engaging with payers and health systems.
In Medicaid, this model may be tied to the concept of billing and rendering providers. Some states may choose to utilize different billing and rendering providers to support National DPP lifestyle change program delivery. Billing providers are reimbursed by Medicaid and rendering providers are typically licensed, credentialed, or other designated Medicaid enrolled provider types that do not have the authority to bill Medicaid but can offer a service under the supervision of the billing provider. More information on billing and rendering providers can be found on the Determining the Medicaid Provider Type page of the Coverage Toolkit.