Building Partnerships → Partner Networks
Partner Networks
A partner network is a group of organizations and representatives of different communities that team up to advance a common goal or vision. In the context of type 2 diabetes prevention, partners leverage each other’s expertise and reach to maximize their capacity and capabilities. Working together, partners can affect population and systems-level changes to increase enrollment into the National Diabetes Prevention Program (National DPP) lifestyle change program.
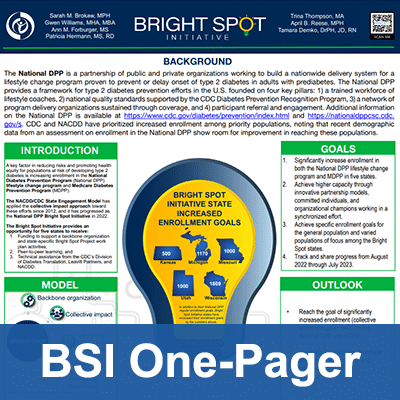
The Bright Spot Initiative (BSI) is an example of how state health departments implemented a partner network that increased enrollment into the National DPP lifestyle change program. Year 1 of the BSI generated robust insights and best practices that may be useful for state health departments considering strategies to expand the National DPP lifestyle change program in their states.
There are five sections on this page:
- Bright Spot Initiative Overview
- Partner Network Approach
- State Health Department Roles
- Readiness and Engagement for State Health Departments Considering a Partner Network Approach
- Centering the Partner Network on Health Equity
Bright Spot Initiative Overview
Collective Impact Background
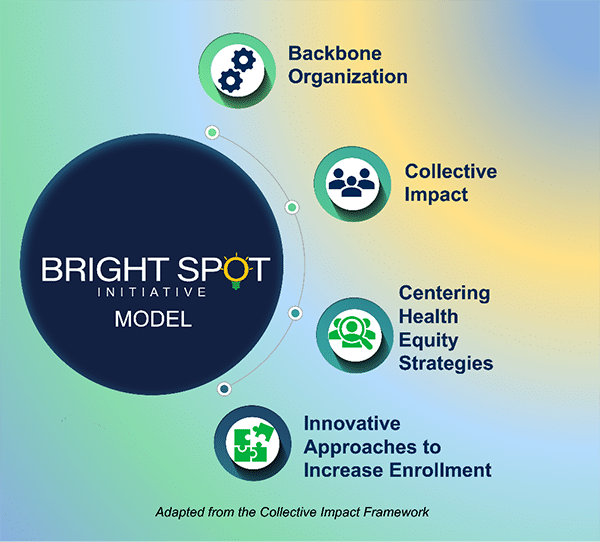
State health departments centered their BSI work around collective impact. Collective impact is an engagement approach which consists of a multisectoral collaboration of organizations and community members that advance equity through shared learnings and integrated actions to achieve population and systems-level change. Collective impact is built on five conditions with equity incorporated throughout. The five conditions are:
- A common agenda – The partner network comes together to collectively define the problem and center around a shared vision to address that problem.
- Shared measurement system – The partner network aligns on tracking data and progress, which fosters continued learning and shared accountability.
- Mutually reinforcing activities – The partner network’s strengths and activities are defined and strategically leveraged to maximize results.
- Continuous communications – The partner network works toward building trust among each other, cultivating strong relationships and promoting collaborative communication.
- Backbone organization – The partner network and overall project management are coordinated through a dedicated central organization or team to push the group toward successful implementation of collective impact.
The Bright Spot Concept
The BSI applies the principles of collective impact and the NACDD/CDC State Engagement Model (StEM) with the goal of dramatically increasing enrollment in the National DPP lifestyle change program and Medicare Diabetes Prevention Program (MDPP). The StEM approach centers around the State Engagement Meeting, where diverse organizations convene to develop a plan to advance the prevention of type 2 diabetes. The BSI further leverages these two models to promote health equity for populations identified as having increased risk of developing type 2 diabetes (priority populations).
Through the BSI, five states were provided funding and technical assistance by NACDD and CDC to implement their projects (see the BSI State Profiles below). States and partner organizations were convened in peer-to-peer learning labs to share key information on topics while attendees engaged in discussions exploring practical solutions and best practices. The information gleaned from the peer-to-peer learning labs was used to develop a compendium of project insights, learnings, and tools for future cohorts.
Goal
The goal of the BSI is to increase enrollment in the National DPP lifestyle change program and the MDPP. The backbone organization—the coordinating body that brings together partners to achieve the goal of increased enrollment, coordinates program activities to achieve the goal (see the Backbone Organizations section below). Partners commit to specific enrollment goals for general and priority populations.
Participants and Efforts to Date
In 2019, CDC and the American Medical Association (AMA) identified North Carolina as the first Bright Spot state in a pilot initiative. The North Carolina Department of Health and Human Services (NC DHHS) partnered with CDC and the AMA to implement and track enrollment strategies through 2021. CDC and the AMA evaluated the pilot and reflected on lessons learned to inform Year 1 of the multi-state BSI, which ran from August 2022 through July 2023.
Bright Spot Initiative Year 1
NACDD and CDC facilitated a competitive application process and selected five state health departments to implement Bright Spot projects in their states:
- Kansas Department of Health and Environment
- Michigan Department of Health and Human Services
- Missouri Department of Health and Senior Services
- Utah Department of Health and Human Services
- Wisconsin Department of Health Services
Bright Spot Initiative Year 1 Learnings
As instrumental partners throughout the BSI work, during Year 1 state health departments expanded their reach to specific priority populations. The departments leveraged existing chronic disease prevention efforts and their robust partner networks to achieve population and systems-level change. States centered health equity throughout their work as a core strategy. The innovative approaches resulted in significant program capacity to enroll persons with prediabetes. See the BSI One-Pager to learn more.
Bright Spot Initiative Webinar
Dramatically Increasing Enrollment into the National Diabetes Prevention Program: An Illuminating Look at the Bright Spot Initiative Webinar
This webinar allows viewers to learn more about the Bright Spot Initiative and glean new ideas about working to increase enrollment in the National DPP and the MDPP through ways to better reach and engage priority populations.
Learning objectives:
- Describe the collective impact approaches and results from the Bright Spot Initiative.
- Explore how states center equity in their Bright Spot Initiative projects.
- Identify challenges and successes experienced by each state, specifically in partnering to reach priority populations.
- Apply lessons learned from Bright Spot Initiative states to your type 2 diabetes prevention efforts.
Bright Spot Initiative State Profiles
Kansas
- State Agency: Kansas Department of Health and Environment (KDHE)
- Backbone Organization: KDHE
- Why backbone organization was selected: KDHE acted as the backbone organization to leverage existing partnerships and connections with organizations that contribute to diabetes prevention across the state.
- Project Overview: KDHE worked with partners to achieve their 500 persons project enrollment goal. They worked with partners to conduct marketing and outreach, host in-person employer events, and coordinate their Arthritis Program with the National DPP lifestyle change program on the HALT platform to increase participation in both programs.
- Priority Population: Hispanic and Latino, Black or African American, and low-income populations.
Michigan
- State Agency: Michigan Department of Health and Human Services (MDHHS)
- Backbone Organization: Michigan Public Health Institute (MPHI) Center for Health Equity Practice (CHEP)
- Why Backbone Organization was Selected: MPHI CHEP’s mission is to center equity, promote health, and advance well-being in the Michigan community. MPHI CHEP was selected to serve as Michigan’s backbone organization because they were uniquely positioned to create and facilitate dialogue between clients, communities, government, and policymakers as they are a trusted voice in the community.
- Project Overview: Michigan conducted a project to increase enrollment of Black and African American persons in the National DPP lifestyle change program through the strengthening of equity leadership and accountability, the utilization of community champions to prioritize the voice of the community, and the bolstering of referrals within the largest hospitals in southeast Michigan.
- Priority Population: Black or African American adults in Wayne, Oakland, and Macomb counties.
To learn more about Michigan’s efforts to support the National DPP lifestyle change program, visit Michigan’s State Story of Medicaid Coverage on the Coverage Toolkit.
Missouri
- State Agency: Missouri Department of Health and Senior Services (DHSS) Diabetes and Heart Disease Program
- Backbone Organization: Simply Strategy
- Why Backbone Organization was Selected: Missouri selected Simply Strategy as the backbone organization because of their previous knowledge of the National DPP lifestyle change program landscape in Missouri, their existing partnerships with National DPP lifestyle change programs in the St. Louis area, and because they had previously contracted with the Missouri DHSS.
- Project Overview: Missouri conducted a project to increase enrollment in the National DPP lifestyle change program by 1,000 participants. Missouri’s project activities worked toward the expansion of state National DPP lifestyle change program suppliers, creation of referral networks across different organizations, development of a bi-directional healthcare provider referral pathway, and augmentation of an existing prediabetes awareness campaign to reach more people.
- Priority Population: Black or African American and Hispanic and Latino adults age 45 and older; high-risk populations located in the St. Louis Region, with a focus on those residing within the St. Louis Promise Zone Region within North St. Louis City and North St. Louis County.
Utah
- State Agency: Healthy Environments Active Living (HEAL) program at the Utah Department of Health and Human Services (DHHS)
- Backbone Organization: Steering Committee for the Prevention of Diabetes in Utah (Steering Committee)
- Why Backbone Organization was Selected: Utah selected the Steering Committee as the backbone organization as they are comprised of experts, specialists, and interested parties from various sectors across the state. The Steering Committee meets to work through and discuss policies that encourage the sustainability of the National DPP lifestyle change program, improve infrastructure within the state, and provide guidance and recommendations to partners.
- Project Overview: In 2022, the state of Utah passed a law that provides coverage of the National DPP lifestyle change program for eligible Medicaid members. DHHS capitalized on this by conducting a project to enroll 500 adults enrolled in Medicaid and 500 adults not covered by Medicaid through outreach to patients and healthcare providers, providing support for CDC-recognized organizations to become Medicaid program suppliers, leveraging the Utah 211 program, and carrying out a social digital marketing campaign.
- Priority Population: Adults enrolled in Medicaid; women age 45 and older; people living in high health improvement areas.
Wisconsin
- State Agency: Wisconsin Department of Health Services (DHS)
- Backbone Organization: The Chronic Disease Prevention Program (CDPP), a program housed in the DHS Division of Public Health.
- Why Backbone Organization was Selected: Wisconsin selected the CDPP as the backbone organization as they work with each National DPP lifestyle change program supplier in the state.
- Project Overview: Wisconsin conducted a project where they partnered with National DPP lifestyle change program and MDPP suppliers across the state and leveraged existing infrastructure to increase enrollment of priority populations in the National DPP lifestyle change program. Wisconsin’s goal was to increase enrollment by 1,809 participants, which was 20 percent more than the baseline enrollment as of July 2022. Wisconsin’s project activities worked toward increasing partnerships across the state with organizations serving priority populations, strengthening technical assistance and coordination among suppliers, developing and implementing a data collection process, and boosting communication and outreach to priority populations.
- Priority Population: Individuals at disproportional risk of developing type 2 diabetes; supplier-specific priority populations that included Asian and Hmong, Black or African American, Hispanic and Latino persons, persons with a high school education or lower, persons age 35 and older, men, and adults enrolled in Medicaid and Medicare.
For more information about Wisconsin’s involvement with the National DPP lifestyle change program, see Wisconsin’s State Story of Medicaid Coverage on the Coverage Toolkit.
Customizing the Bright Spot Initiative to State Needs
Each state integrated collective impact uniquely within its BSI project. This page highlights the different experiences and approaches that each state health department took. State health departments considering a partner network approach may reflect on the insights presented and adapt their approach to what will work in their state. The following sections highlight elements and processes of an effective partner network that states may consider when planning an approach that is unique to their priority populations.
Partner Network Approach
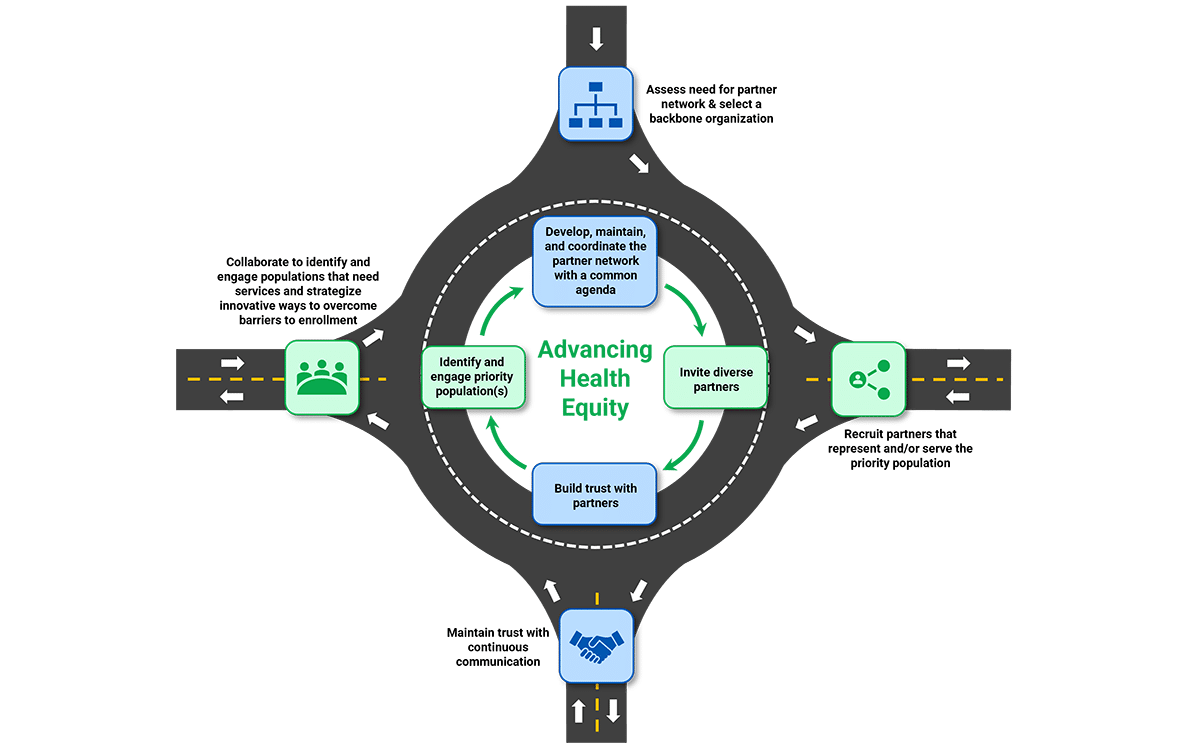
The partner network approach is a continuous process that involves six activities: assessing the need for a partner network, selecting a backbone organization, selecting partners, gaining buy-in from partners, identifying priority population(s), and engaging priority population(s). Each state health department that pursues a partner network approach will start at different points in the process. Regardless of where and how a state health department begins their partner network approach to advancing diabetes prevention, they should anticipate continually and iteratively working on these six activities.
Developing and Maintaining a Partner Network for the National DPP Lifestyle Change Program
Backbone Organizations
What is a Backbone Organization?
A backbone organization is critical for the effective implementation of a partner network. The backbone organization as the coordinating body, brings together diverse partners and leads a synchronized effort to establish and achieve the goal of increased enrollment in the National DPP lifestyle change program. Backbone organizations create and translate a common agenda into tactical activities that are executed and managed on the ground in states and regions. Examples of organizations that served in a backbone organization capacity include state health departments and public health institutions. However, backbone organizations may also be community-based organizations (CBOs).
How is a Backbone Organization Selected?
State health departments pursuing a partner network approach to increase enrollment in the National DPP lifestyle change program decide whether they will serve as the backbone organization or partner with another organization. When deciding, it is important to evaluate whether the organization or department can fulfill the roles and responsibilities outlined below. Successful backbone organizations have proven their capability through prior collaborative projects and initiatives and have existing partnerships with organizations advancing diabetes prevention.
What is the Role of a Backbone Organization?
The backbone organization provides project management, data analytics, partnership engagement support, and provide staff (or contractors) to work with CDC-recognized organizations and other key partners in the state or region to assist the partners in meeting local enrollment goals.
The following outlines the key roles and responsibilities of a backbone organization to drive large-scale participant enrollment:
- Serve as an overall project manager.
- Conduct a landscape and data analysis to identify additional opportunities to increase enrollment.
- Facilitate partner commitment.
- Plan and facilitate regular meetings with the partners.
- Work to keep partners engaged, committed, and on task.
- Help partners establish a realistic enrollment goal.
- Track project progress against agreed-upon metrics.
- Develop standard methodology and processes that align with local, regional, and national goals.
To learn more about backbone organizations, see the National DPP NC Backbone Organization Roles and Responsibilities document, and the Bright Spot Initiative Backbone Organization Roles and Responsibilities.
Developing a Partner Network
After identifying a backbone organization, state health departments should continue to form their partner network. A strong partner network includes organizations and community members with a common agenda and a shared vision. State health departments considering a partner network must establish new and strengthen existing partnerships to increase enrollment in the National DPP lifestyle change program. In addition to the BSI approach, another vehicle for establishing a network could be to form an Umbrella Hub Arrangement (UHA). UHAs connect community-based organizations (CBOs) with healthcare payment systems to pursue sustainable reimbursement for the National DPP lifestyle change program. UHAs effectively streamline administrative and contractual efforts to allow partners to maximize their efforts toward a shared goal. To learn more about UHAs, visit the Umbrella Hub Arrangements page of the Coverage Toolkit. Important partners in both a UHA and a partner network include but are not limited to:
- National DPP lifestyle change program suppliers
- CDC-recognized organizations
- CBOs
- Community members
- Healthcare associations
- MDPP suppliers
- Payers
- Pharmacies
- Providers and healthcare organizations
- State health departments
- Technical Partners (e.g., referral or billing platforms)
State health departments may use a partner network approach, a UHA approach, or both.
Selecting Partners
Partner networks are only as effective as the organizations involved. Partnering with organizations with a track record of successful collaboration is essential to drive change toward the shared goal. Organizations committed to preventing type 2 diabetes and other chronic conditions could be potential strong partners. Consider evaluating a partner network’s membership based on the following:
- What are the organizations operating within communities of identified priority populations, and could they effectively support the shared goal of increased enrollment?
- Are there existing partners that have experience in diabetes prevention? What roles do they currently fill or could fill?
- What resources would a potential partner bring to the partner network? Do those resources align with the strategic needs of the group?
- How could an organization or individual be involved in planning and project activities?
- Are there potential barriers to recruiting certain partners? Are there strategies that could help overcome those barriers?
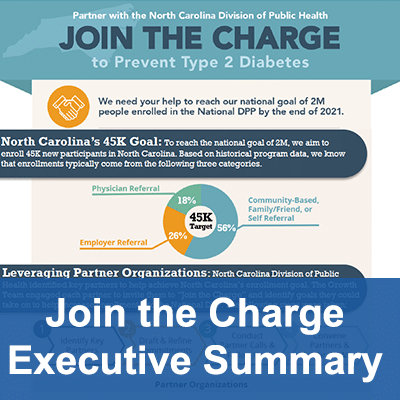
Gaining Buy-In from Partners
Partner networks are most effective when the state health department garners collective buy-in from partners early on during partnership development. Gaining buy-in early aids the state health department in finding partners from different sectors that are devoted to specific activities that align with the shared goal of increasing enrollment and advancing diabetes prevention. Some of these activities might center around the following:
- Awareness
- Identification, screening, and testing
- Equity
- Capacity building
- Referrals
- Coverage
- Availability
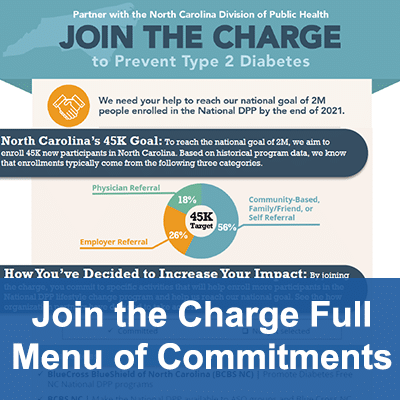
The Join the Charge Executive Summary and the Join the Charge Full Menu of Commitments documents show the types of organizations that NC DHHS partnered with and what their commitments were. Consider reviewing these documents to get an idea of the types of partnerships that can be part of a partner network.
State Health Department Roles
State Health Departments Well-Positioned to Support Partner Networks
State health departments typically have extensive experience promoting and expanding type 2 diabetes prevention through grant-funded work (such as the 2320, 1815, 1817, and 1705 grants), robust partnerships and capabilities to build new ones, a commitment to promoting health equity, building infrastructure to work with National DPP lifestyle change program suppliers, and/or experience working with communities across their states. This experience positions state health departments well to participate or be a backbone organization in a partner network to increase enrollment in the National DPP lifestyle change program.
Potential Roles of State Health Departments within a Partner Network
State health departments may play the following roles within a partner network:
Facilitate Connections
- Identify connection opportunities between partners and facilitate an introduction. Partners may be able to share resources and support each other as they further their respective diabetes prevention efforts.
- Develop and facilitate partner networks that include various partners (all types of payers, delivery organizations, healthcare providers, employers, and employer coalitions) with different strengths; strategically engage each partner to maximize promotion and enrollment efforts. State health departments have decades of experience providing leadership and applying the StEM framework to convene and engage multisectoral partners to develop a statewide diabetes action plan to achieve a shared goal toward scaling and sustaining the National DPP lifestyle change program.
- Help priority populations by partnering with organizations that influence the communities they operate in and incorporate the community’s voice.
- Align partners and partner networks on National DPP lifestyle change program messaging—marketing materials developed by different partners should be culturally relevant and consistent in language.
- Synergize other chronic disease prevention and management efforts like arthritis management, colorectal cancer screening, and food assistance when promoting the National DPP lifestyle change program – share information when administering programs.
- Work with community champions to build trust within communities.
KDHE worked with their partner CAPPA Health to connect their Diabetes Program and their Arthritis Program. They combined the National DPP lifestyle change program and the Walk with Ease Program on the shared HALT referral platform to increase participation among persons that are both prediabetic and have arthritis. Synergizing efforts across both chronic disease programs allowed the state to maximize their reach when referring potential participants to either program. KDHE utilized the coupling of the Walk with Ease and National DPP lifestyle change programs to connect additional chronic disease programs. This has led to the creation of the Kansas Community Care Alliance (KCCA), which is a collaborative alliance between chronic disease community partners, community members, and multiple sections within KDHE.
Provide Technical Assistance to Partners
- Have dedicated staff that can assist organizations through different aspects of the program.
- Objectively identify priority populations within the state using a data-backed approach:
- Break down beneficiary data by demographics.
- Work with partners to leverage their patient data.
- Use data to understand better how populations in the state consume digital media – tailor marketing using that information.
- Understand where there are gaps in data and identify opportunities to fill those gaps (e.g., sub-populations that are not effectively captured in existing data sets).
- Work with state policymakers to align on policy language and structure that will effectively provide coverage for the National DPP lifestyle change program for persons enrolled in Medicaid.
HEAL in Utah DHHS identified specific areas where they lacked expertise and then cross-referenced those areas with local health departments that could fill those gaps. Instead of trying to do that work themselves, they have shifted power and supported local health departments that are subject matter experts in their regions to carry out better work that will impact their communities. The ability to shift power to the entity most skilled in completing a specific task frees up capacity for the state health department to focus their energy toward providing technical assistance and support to those partners.
Compile Resources
- Share a repository of resources partners can leverage for their efforts, such as pre-cleared marketing materials and healthcare provider toolkits.
- Offer marketing materials; create customized, culturally relevant materials.
Missouri DHSS Diabetes and Heart Disease Program partnered with Elasticity to develop a healthcare provider toolkit for referring patients to organizations delivering the National DPP lifestyle change program. They uploaded the toolkit to their website and worked with the Missouri Hospital Association to distribute it to healthcare providers to integrate into their workflows. The state health department also partnered with the Missouri Family Physicians Magazine to highlight the toolkit in a quarterly issue sent to more than 3,000 physicians and medical students.
Track Progress
- Create open channels for feedback to facilitate accountability across partner networks.
MDHHS worked to develop feedback channels that directly loop back into their processes and how they work with partners, which strengthened accountability throughout their project. The state health department’s large health system partners—Trinity Health, Corewell Health, Ascension, and Henry Ford Health— and the National Kidney Foundation of Michigan have been highly involved in providing informal feedback through consistent collaborative meetings on the types of changes and improvements needed to bolster enrollment numbers. The Community Champion Workgroup surveyed healthcare providers, lifestyle coaches, and community members to gather their feedback and share with health system partners.
Celebrate Wins
- Convene the partners regularly to thank them for their contributions. Help promote recognition of their efforts through statewide channels.
Wisconsin DHS met monthly with its nine partners including health systems, county health departments, pharmacies, and YMCAs, where partners shared their work. The state health department provided time to spotlight different partners at each meeting and discussed how things were going, any advancements partners made in their work, and any challenges partners may have experienced. At the end of Year 1, partners gave a mini poster presentation about their process, enrollment, experiences, and work success.
To learn more about how NC DHHS supported partners, see the Join the Charge Transition Package document. This document provides details on how NC DHHS facilitated connections, compiled resources, tracked progress, and celebrated wins to support their partner network throughout their BSI project.
Readiness and Engagement for State Health Departments Considering a Partner Network Approach
Assessing Readiness
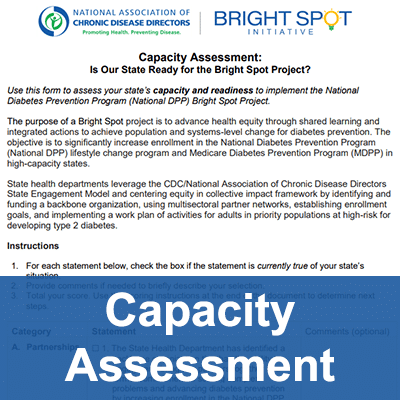
State health departments are vital partners for partner networks due to their experience, capability, and commitment to diabetes prevention. Their capacity allows for rapidly mobilizing work plan tactics and activities to support a partner network. After learning more about partner networks and the BSI, the next step for a state health department considering its partner network is to assess its readiness for engagement. State health departments may consider the following next steps:
- Conduct a capacity assessment to gauge whether the state health department can implement a partner network model. The Capacity Assessment document is provided as a resource for this purpose.
- Understand why there is interest in a partner network, what the enrollment goals are, which priority populations would be served, who would be engaged as partners, and how partners will be engaged to implement their efforts? State health departments can refer to the StEM process and the Qualifications Statement document for engaging partners to address these strategic questions.
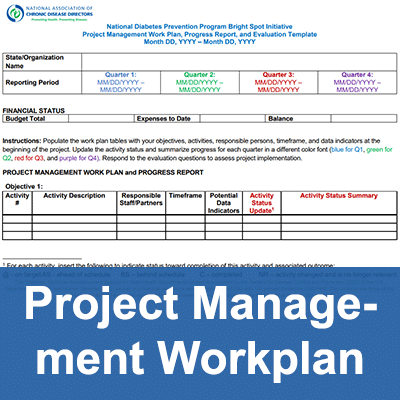
- Develop a project management work plan and an evaluation plan. State health departments can utilize the Project Management Work Plan template for their partner network approach.
Centering the Partner Network on Health Equity
Health Equity and Collective Impact
Collective impact integrates health equity through five conditions: a common agenda, shared measurement system, mutually reinforcing activities, continuous communications, and backbone support organization. State health departments considering a partner network approach to increasing enrollment should incorporate health equity throughout their and their partners’ activities. CDC defines health equity as the state in which everyone has a fair and just opportunity to attain their highest level of health. Health equity implies that everyone has a fair opportunity to achieve their full health potential, and achieving health equity would mean the removal of “avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically or by other means of stratification.”
Experts in collective impact have identified five emerging strategies critical to centering health equity:
- Ground the work in data and context, and target solutions.
- Focus on systems change, in addition to programs and services.
- Shift power within the collaborative.
- Listen to and act with the community.
- Build equity leadership and accountability.
Learn more about how promoting health equity can support the impact of the National DPP lifestyle change program, and how the program itself can be used as a tool to promote health equity on the Health Equity and the National DPP page of the Coverage Toolkit.
Access the following NACDD webinars for more information about health equity and social determinants of health.
Multidirectional e-Referral Results in Health Equity – Part 1
Timing: 1:02:05
Centering Health Equity in Practice
State health departments participating in the BSI used the five strategies above to center health equity in ways that aligned with the needs and populations in their state:
- Ground the work in data and context, and target solutions. Used data to identify underserved communities and help states create tailored geographic approaches.
- Focus on systems change, in addition to programs and services. Established and leveraged existing partnerships with organizations that mirror the populations they serve to create opportunities for increasing awareness among priority populations and recruiting new lifestyle coaches.
- Shift power within the collaborative. Actively incorporated community leaders or champions into decision-making roles to further health equity.
- Listen to and act with the community. Created and customized culturally relevant material that resonated with priority populations and made the National DPP lifestyle change program more accessible.
- Build equity leadership and accountability. Conducted health equity trainings to assist in creating a shared understanding of health equity and to actualize it throughout multiple aspects of the partner network approach.
Priority Populations
CDC and NACDD have prioritized increased enrollment among priority populations. Recent demographic data from an enrollment assessment of National DPP lifestyle change programs showed room for improvement in reaching these populations. Furthermore, there is an urgency to increase the enrollment of Medicare beneficiaries in the MDPP. State health departments considering a partner network approach should identify priority populations to engage in their state.
Approaches to Identifying Priority Populations
Each state health department in Year 1 of the BSI leveraged data, recent legislation, and state- and federally-recognized zones of high need to make informed decisions when identifying priority populations in their state:
- Kansas analyzed Behavioral Risk Factor Surveillance System (BRFSS) data to identify disparities in prediabetes and type 2 diabetes prevalence rates in different geographic regions. Kansas identified men as disproportionately affected through their data analysis and designated them as a priority population.
- Michigan utilized BRFFS data to identify that Black non-Hispanic adults in the southeast Michigan region were disproportionately experiencing prediabetes and type 2 diabetes and were underrepresented in the National DPP lifestyle change program.
- Missouri focused on the St. Louis Region, with an additional targeted sub-population in the St. Louis Promise Zone Region. The St. Louis Promise Zone region is recognized federally as a high-poverty area with little or no resources for communities to address unmet needs related to social determinants of health.
- Utah directed its efforts toward increasing enrollment in the Medicaid population in line with recent legislation providing coverage of the National DPP lifestyle change program for eligible Medicaid members.
- Wisconsin analyzed sociodemographic information and diabetes and prediabetes across the state. They used the American Community Survey (ACS) data to identify potential priority populations specific to each of their nine National DPP lifestyle change program supplier partners. They identified Asian and Hmong, Black or African American, Hispanic and Latino, persons with a high school education or lower, persons 35 and older, men, and Medicaid and Medicare members as priority populations.
Engaging Priority Populations
After identifying priority populations, state health departments should consider how best to engage those populations to maximize reach and reception. BSI state health departments carried out unique project plans to engage their populations of focus. Here are some examples:
- One of Wisconsin’s CDC-recognized organizations connected with the Wisconsin Hmong Nurses Association to highlight healthcare provider education about the National DPP lifestyle change program and Diabetes Self-Management Education and Support (DSMES). Educational materials were shared to further partner with this organization and connect program suppliers whose priority populations include Hmong communities with the association. Partnering with an organization that mirrored one of its priority populations promoted greater reach and influence.
- In Michigan, MDHHS and MPHI CHEP piloted a community champion workgroup which consisted of one community champion from each health system in the Southeast Michigan Hospital Collaborative (SEMIHC) that represented the priority populations they worked with. The community champions elevated the voices of their communities by collecting feedback and providing it to the health systems. The workgroup evaluated the results and provided recommendations about identifying and solving barriers and future diabetes prevention efforts.
- Utah utilized a staff member to conduct outreach to healthcare providers with high rates of Medicaid patients eligible for the National DPP lifestyle change program to provide resources on how to help patients enroll and how to receive reimbursement from Medicaid. The staff member contacted 24 primary care physicians who serve Medicaid members with prediabetes.
Marketing to Priority Populations
Marketing is an essential tool to use when engaging with priority populations. State health departments must consider how their marketing strategy aligns with their identified priority populations and their overall engagement strategy. Outreach should be created with the specific audience in mind, ensuring that the language will resonate with the priority population. Priority populations that relate to the marketing materials presented to them may be more inclined to inquire about or enroll in the National DPP lifestyle change program. State health departments should ensure that outreach is culturally relevant, relatable, and delivered through the correct media channels that will reach their priority populations. To learn more about reaching out to potential program participants, visit the Communicating and Promoting the National DPP as a Medicaid Benefit page and the Recruitment and Referral page of the Coverage Toolkit.
Partner networks provide state health departments with more resources and capability to market the National DPP lifestyle change program effectively. Healthcare providers, National DPP lifestyle change program suppliers, health plans, community-based organizations, CDC-recognized organizations, marketing vendors, and/or other entities can utilize existing marketing materials in their workflows and awareness campaigns.
To view examples of effective marketing materials and strategies, see the Do You Have Diabetes, and Do You Have Prediabetes – Spanish documents. In addition, please see the BSI Learning Lab 4 Presentation on marketing the National DPP lifestyle change program, and listening to and acting with the community.
Multi-Payer Approach
When identifying and engaging priority populations, it is important to understand the barriers to enrollment they may experience. The costs of the National DPP lifestyle change program may inhibit or prevent people from enrolling. State health departments interested in partner networks to significantly increase enrollment in the National DPP lifestyle change program may consider utilizing existing assets and coverage in their states such as Medicare, Medicaid, commercial health plans, state employee coverage, employer-sponsored insurance, and coverage in correctional facilities (i.e., prisons). A multi-payer approach will ensure that populations with different types of insurance coverage can enroll in the National DPP lifestyle change program, eliminating a potential barrier to enrollment.
States may work with existing partners like employers or commercial health plans to expand their employees’ coverage for the National DPP lifestyle change program. The Case for Coverage for Commercial Health Plans and Employers page of the Coverage Toolkit provides resources for working with employers or commercial health plans. Healm is a free resource designed to support employers considering covering the National DPP lifestyle change program as a benefit for their employees.
If a state does not provide Medicaid coverage of the National DPP lifestyle change program, state health departments may consider partnering with the Medicaid department and state policymakers. Find a map of the states currently covering the Medicaid program here. State health departments can begin having those discussions and work toward establishing Medicaid coverage using the resources found on the Case for Coverage for Medicaid page of the Coverage Toolkit.
Additional information on how NACDD advances diabetes prevention, NACDD partners, success stories, and resources related to diabetes are available on the NACDD Diabetes page.