Create a New Provider Type for CDC-Recognized Organizations
States can elect to create a new provider type that would allow CDC-recognized organizations such as community-based or other organizations to enroll in Medicaid and deliver the National DPP lifestyle change program.
Creating a new provider type gives states the advantage of enrolling a group of providers who have experience with and are specifically focused on delivering the National DPP lifestyle change program. It can also allow states to better track and evaluate use of the benefit. California, Maryland, New York, and Pennsylvania have all created a new provider type that allows CDC-recognized organizations to enroll in Medicaid. To learn about each state’s approach, visit the State Stories of Medicaid Coverage page of the Coverage Toolkit.
A state will need to create a new provider type (if an existing provider type does not exist) to allow CDC-recognized organizations to enroll in Medicaid even if it is only offering the National DPP lifestyle change program through managed care. The current Medicaid managed care rule requires all MCO-contracted providers to enroll as Medicaid providers, even if they do not deliver services to Medicaid fee-for-service beneficiaries. Maryland and Pennsylvania are examples of states that created a new provider type for CDC-recognized organizations participating in the states’ Medicaid managed care programs.
It can take 6-12 months for a state Medicaid agency to create a new provider type. There are several reasons why the process can take this long. First, creating a new provider type often means the Medicaid agency is establishing and covering a new service, which involves administrative/or and regulatory changes. Second, creating the new provider type is just one of many ongoing program operations and changes competing for time and resources within Medicaid―and balancing these multiple priorities and programs can extend the timeline. Third, creating a new provider type requires a substantial amount of coordination both within and beyond the Medicaid agency. Medicaid agencies may have to coordinate with internal reimbursement, coverage, and IT staff, as well as coordinate with external partners such as the state legislature, the public health department, and health care provider associations (who can help engage health care providers on the new provider type and service).
Medicaid Communication to CDC-Recognized Organizations
Communicating to CDC-recognized organizations that Medicaid has created a new provider type is an important step in program implementation. For example, Maryland Medicaid developed a series of webinars to explain the process for how CDC-recognized organizations can enroll in Maryland’s electronic Provider Revalidation and Enrollment (ePREP) portal under its new provider type. Maryland Medicaid provides access to these webinars (both recordings and notices about upcoming webinars), the ePREP link, and other documents related to Medicaid coverage of the National DPP lifestyle change program on its HealthChoice Diabetes Prevention Program Information for Providers website.
Similarly, California created a website, hosted a webinar, and provided a FAQ document to communicate to CDC-recognized organizations how to enroll in Medi-Cal.
Pennsylvania Medicaid began its process of communicating the creation of a new Medicaid provider type through a Medicaid bulletin describing how CDC-recognized organizations can enroll in Medicaid. Pennsylvania also surveyed all CDC-recognized organizations in the state to assess the organizations’ knowledge of the new provider type and to understand what type of technical assistance would be most valuable to provide regarding Medicaid enrollment and delivering the National DPP lifestyle change program to Medicaid beneficiaries.
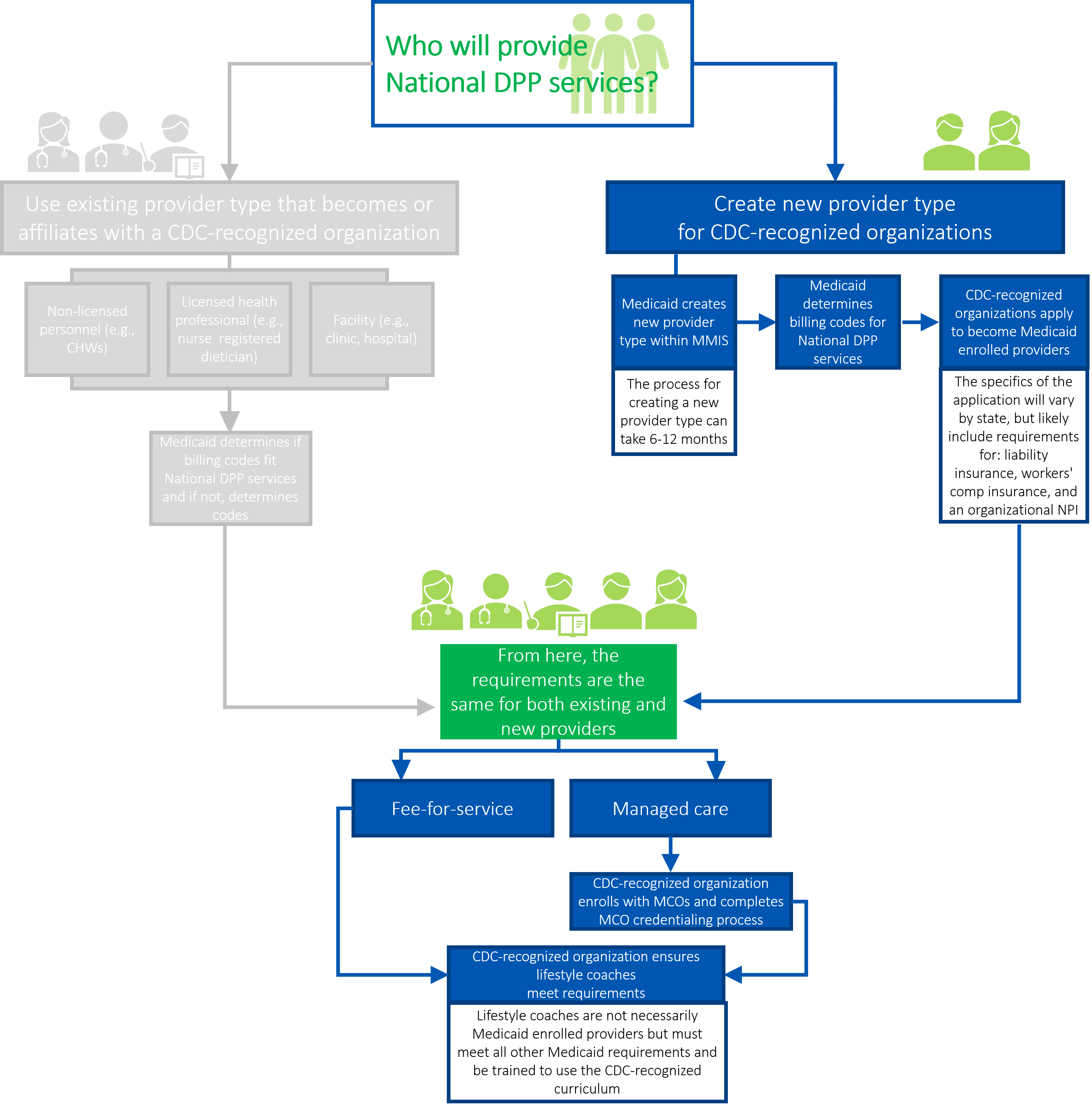
The following paragraphs provide additional details about the steps in the above graphic.
Medicaid Creates New Provider Type Within MMIS
Another reason the process can take several months is that the new provider type must be entered into the Medicaid Management Information System (MMIS) or Medicaid Enterprise System (MES). This includes developing programs and systems that (1) allow the provider to enroll and be reimbursed, (2) capture data, (3) develop and submit reports, and (4) track new providers, among other processes. This is a time consuming process and often a manual process, regardless of the age of the MMIS or MES system. For example, provider type values can be referenced in many places throughout the system, and it takes time to reprogram these values when a change is made. Additionally, testing must be scheduled and executed, and defects addressed before the system goes live.
Once a new provider type is created within the MMIS or MES system, and Medicaid is ready to enroll new Medicaid providers, it may be advisable to create resources and training opportunities for these new providers (see the Medicaid Communication to CDC-Recognized Organizations section above).
Medicaid Determines Billing Codes for National DPP Lifestyle Change Program Services
Medicaid must identify or develop billing codes for National DPP lifestyle change program sessions in order to reimburse providers. National DPP-specific CPT codes (0403T and 0488T) are intended to be used by CDC-recognized organizations that provide National DPP lifestyle change program services. For more information, please see the Coding and Billing page of the Coverage Toolkit.
CDC-Recognized Organizations Apply to Become Medicaid Enrolled Providers
CDC-recognized organizations must submit appropriate documentation to enroll in Medicaid. Exact requirements vary by state and may include: submission of an application to Medicaid, proof of general liability insurance for the organization’s administrative location, proof of workers’ compensation insurance, proof of CDC recognition, and an organizational National Provider Identifier (NPI). An NPI is a unique identification number that is needed to submit claims.
Medicaid Conducts Screening of CDC-Recognized Organizations
The Centers for Medicare & Medicaid Services (CMS) considers Medicare Diabetes Prevention Program (MDPP) providers to be a high categorical risk for fraud and abuse. MDPP suppliers must therefore comply with high-risk screening requirements including site visits and background checks, and fingerprinting for individuals with 5% or more ownership of the organization. Because Medicare categorizes National DPP lifestyle change program providers as high risk, Medicaid may generally follow that risk status as well and conduct high-risk screenings of CDC recognized organizations (per interpretation of the rule below).
For more information about high risk status, please see the February 2, 2011 final rule on provider screening: Medicare, Medicaid, and Children’s Health Insurance Programs; Additional Screening Requirements, Application Fees, Temporary Enrollment Moratoria, Payment Suspensions and Compliance Plans for Providers and Suppliers.
Medicaid Determines Site Visits If Using Online Providers
Another consideration for creating a new provider type is where and how site visits will occur. Numerous factors may shape these policies, including if the National DPP lifestyle change program is delivered online, through distance learning, and/or through a combination approach, if the CDC-recognized organization’s administrative offices are located in a different state, and if the Medicaid agency rated the CDC-recognized organization as high-risk. State Medicaid agencies may consider various options for site visits for these and other circumstances. For example, Medicaid agencies might require an in-person site visit which would mean the CDC-recognized organization must have an administrative office located in-state. Medicaid agencies may be able to accept a virtual site visit of an administrative office located in another state. Finally, a Medicaid agency may be able to accept a site visit conducted by a different state’s Medicaid agency.
Managed Care: CDC-Recognized Organization Enrolls with MCOs and Completes MCO Credentialing Process
Many state Medicaid agencies contract with Medicaid managed care organizations (MCOs). In a managed care environment, the Medicaid agency contracts with and pays MCOs a capitated rate to deliver Medicaid covered services to beneficiaries. In these states, the CDC-recognized organization will likely enroll in one or more MCO networks and complete each MCO’s credentialing process.
Some MCOs may pursue a delegated credentialing process for lifestyle coaches. With delegated credentialing, the MCO is responsible for credentialing the CDC-recognized organization but is not responsible for credentialing the individual lifestyle coaches (see section below). For more information on MCOs, please see the Engaging MCOs to Attain Coverage page.
CDC-Recognized Organization Ensures Lifestyle Coaches Meet Requirements
Lifestyle coaches facilitate National DPP lifestyle change program sessions. When a CDC-recognized organization becomes a Medicaid enrolled provider, its individual lifestyle coaches may not have to enroll with Medicaid. Instead, the CDC-recognized organization would be responsible for ensuring the lifestyle coaches are trained and qualified to facilitate the National DPP lifestyle change program as well as meet all other Medicaid requirements. As the Medicaid-enrolled provider, the CDC-recognized organization may then need to provide updated rosters of its lifestyle coaches to Medicaid.
Content Last Updated: January 16, 2021









