Use an Existing Provider Type that Becomes or Affiliates with a CDC-Recognized Organization
States can elect to use an existing provider type that is already enrolled in Medicaid to deliver the National DPP lifestyle change program. States can allow licensed professionals (e.g., physicians, nurses (including advance practice registered nurses – APRNs), registered dieticians, certified diabetes care and education specialists, pharmacists, etc.), unlicensed professionals (e.g., community health workers), and facilities (e.g., clinics, hospitals, federally qualified health centers, etc.) to deliver and/or be reimbursed for the program. The existing Medicaid enrolled provider can serve as the program provider , or oversee another provider in cases when there are different billing and rendering providers.
Leveraging existing provider types may mean the state will not need to pursue a State Plan Amendment (SPA) if the Medicaid State Plan already adequately addresses the services and reimbursement required for National DPP lifestyle change program coverage. For more information about SPAs, see the Attaining Coverage Through a Medicaid State Plan page of the Coverage Toolkit.
States must also ensure existing Medicaid-enrolled providers are qualified (and willing) to provide National DPP lifestyle change program sessions. To deliver the National DPP lifestyle change program, a currently enrolled Medicaid provider must meet the Diabetes Prevention Recognition Program (DPRP) requirements to become a CDC-recognized organization and must provide or be aligned with lifestyle coaches who are trained to use the CDC-approved curriculum. For example, if the currently enrolled Medicaid provider is a licensed or non-licensed individual practitioner, that individual must be trained to use the CDC-approved curriculum and be affiliated with a CDC-recognized organization.
Utilizing Community Health Workers
Community health workers (CHWs) are non-licensed providers. Several states allow Medicaid reimbursement of CHWs, which means CHWs can potentially serve as Medicaid-enrolled lifestyle coaches for the National DPP lifestyle change program (for a list of which states offer Medicaid reimbursement for CHW services, see the interactive map on the National Academy for State Health Policy (NASHP) website). For example, Minnesota was able to use CHWs as lifestyle coaches for its Medicaid population without the submission of a new SPA because the Medicaid State Plan already included language defining preventive services that was broad enough to encompass the National DPP lifestyle change program and covered services provided by CHWs (see the Minnesota example on the (see the Minnesota example on the Attaining Coverage Through a Medicaid State Plan page and the Minnesota State Story of Medicaid Coverage for more details).
States’ policies on reimbursement and certification for CHWs vary. Some states, like Minnesota, require CHWs to be certified for Medicaid reimbursement. To learn more about certification and other implementation considerations, see the CDC’s Implementing Considerations for Community Health Workers.
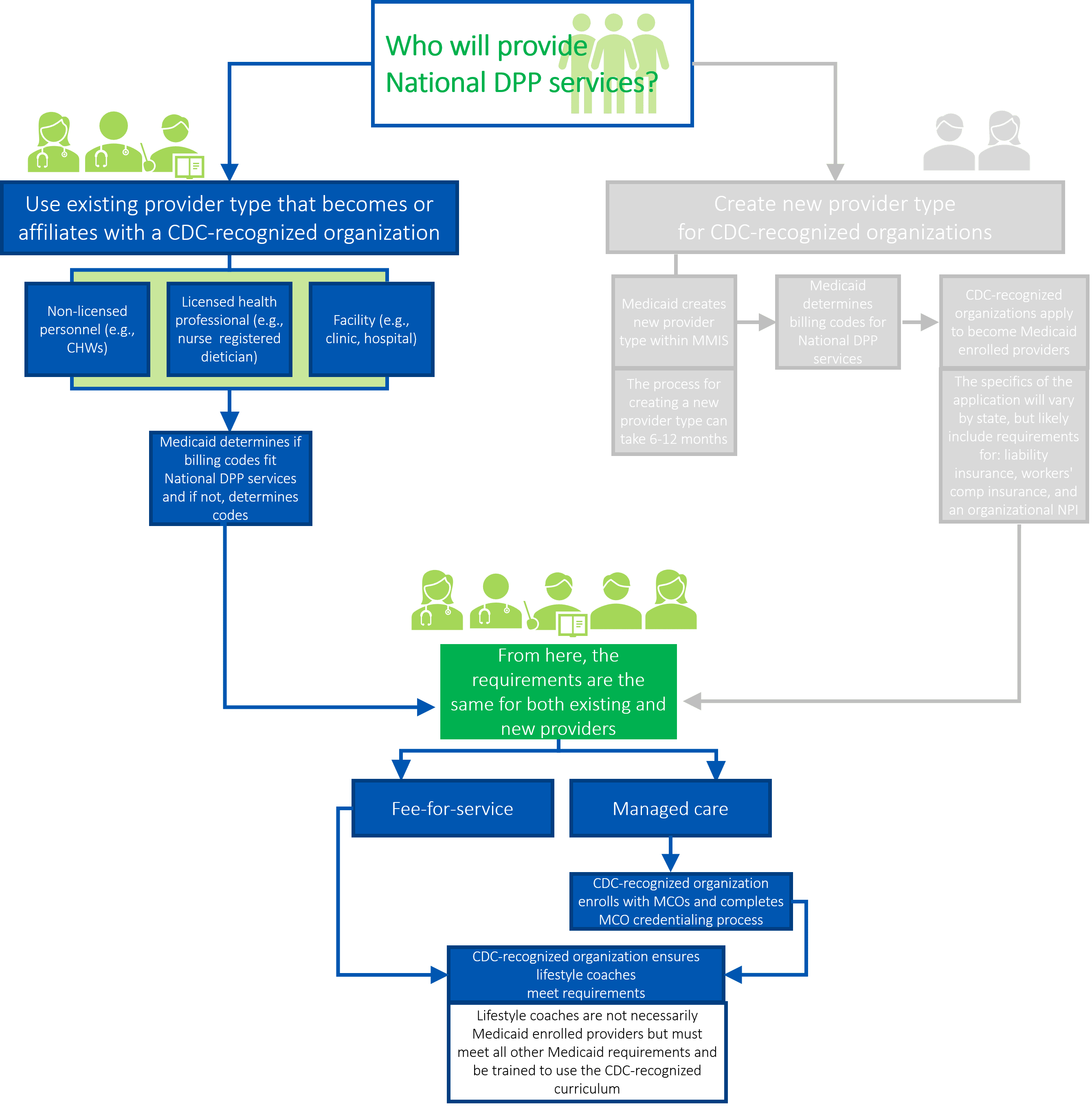
The following paragraphs provide additional details about the steps in the above graphic.
Medicaid Determines if Billing Codes Fit National DPP Lifestyle Change Program Services and if not, Determines Codes
Even when Medicaid uses an existing provider type, these providers may not be authorized to bill for the codes associated with the National DPP lifestyle change program. Moreover, the codes that existing Medicaid enrolled providers can bill for may not necessarily fit the specifications of the National DPP lifestyle change program schedule of sessions. Finally, the use of codes not specified for the National DPP lifestyle change program services may make it impossible to effectively evaluate the utilization of the program. In these cases, it may be necessary for Medicaid to add or open a new code to the state system. For more information, please see the Coding and Billing page.
Managed Care: CDC-Recognized Organization Enrolls with MCOs and Completes MCO Credentialing Process
Many state Medicaid agencies contract with Medicaid managed care organizations (MCOs). In a managed care environment, the Medicaid agency contracts with and pays MCOs a capitated rate to deliver Medicaid covered services to beneficiaries. In these states, the CDC-recognized organization will likely enroll in one or more MCO networks and complete each MCO’s credentialing process.
Some MCOs may pursue a delegated credentialing process for lifestyle coaches. With delegated credentialing, the MCO is responsible for credentialing the CDC-recognized organization, but is not responsible for credentialing the individual lifestyle coaches (see section below). For more information on MCOs, please see the Engaging MCOs to Attain Coverage page.
CDC-Recognized Organization Ensures Lifestyle Coaches Meet Requirements
Lifestyle coaches facilitate National DPP lifestyle change program sessions. When a CDC-recognized organization becomes a Medicaid enrolled provider, its individual lifestyle coaches may not have to enroll with Medicaid. Instead, the CDC-recognized organization would be responsible for ensuring the lifestyle coaches are trained and qualified to facilitate the National DPP lifestyle change program as well as meet all other Medicaid requirements. As the Medicaid-enrolled provider, the CDC-recognized organization may then need to provide updated rosters of its lifestyle coaches to Medicaid.









