Health Equity → Health Equity and the National DPP → The National DPP and HRSN
Addressing HRSN Through the National DPP Lifestyle Change Program
The National Diabetes Prevention Program (National DPP) lifestyle change program is uniquely positioned to address social determinants of health (SDOH) to promote health equity and reduce health disparities in type 2 diabetes. The program can accomplish this by considering the implications of SDOH and addressing unmet health-related social needs (HRSN) among program participants. This page will discuss how the National DPP lifestyle change program teaches valuable skills that address HRSN, as well as opportunities to address HRSN to support participants’ success in the program. It is divided into the following sections:
- Health Equity Modifiable Slide Deck
- The National DPP Lifestyle Change Program Curriculum Focuses on Valuable Skills That Address HRSN
- Addressing HRSN Can Support Participant Success in the National DPP Lifestyle Change Program
- Examples of Addressing HRSN Through the National DPP Lifestyle Change Program
- Health Equity and COVID-19
Health Equity Modifiable Slide Deck
The Health Equity Modifiable Slide Deck was created to support conversations between state health departments and partners working to promote the National DPP lifestyle change program. The slide deck’s content supports the potential for the National DPP lifestyle change program to help achieve health equity goals, reduce health disparities, and overcome health and economic social needs. This slide deck can be used as part of strategic conversations to obtain buy-in, create alliances, and initiate collaborations to improve health equity.
The National DPP Lifestyle Change Program Curriculum Focuses on Valuable Skills That Address HRSN
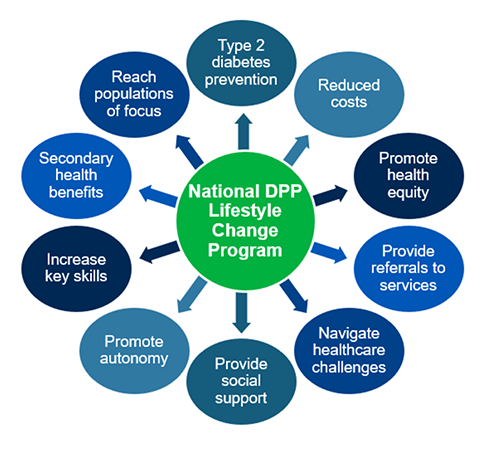
The curriculum of the National DPP lifestyle change program gives participants the opportunity to focus on skills including decision making, problem solving, stress management, and priority setting that can help participants overcome HRSN. The program curriculum respects participant dignity and their autonomy to make health behavior changes with support from Lifestyle Coaches. The relationships between a participant and their Lifestyle Coach can increase self-efficacy among participants. Likewise, the relationships between participants are beneficial and can provide long-term social support and camaraderie as participants seek to make personal health behavior changes.
In addition to these benefits, the National DPP lifestyle change program may provide a year-long forum to discuss the complexities of health care, health care providers, and health insurance, ideally leaving participants with a clearer understanding of how to function within the health care system. Due to its multiple touch points over the course of one year, the program can also be used as a referral point to encourage participants to access other community resources or health, behavioral, and social care services.
Finally, CDC-recognized organizations and Lifestyle Coaches can strengthen the innovative role the National DPP lifestyle change program can play in promoting health equity. CDC-recognized organizations are typically located in the community and may offer other programs and services that promote health equity. Lifestyle Coaches are uniquely trained, and can include non-traditional providers, such as community health workers (CHWs), which often are individuals living in the same communities they serve.
Addressing HRSN Can Support Participant Success in the National DPP Lifestyle Change Program
Participant retention and engagement in the National DPP lifestyle change program can increase as barriers to participation are overcome. The structure of the program provides space for individualized support, as Lifestyle Coaches are uniquely positioned to work with participants to address their specific HRSN. When Lifestyle Coaches are from the same community as program participants, they often understand participant barriers and opportunities.
The Minnesota Best Practices Guide for Lifestyle Coaches and Program Coordinators highlights several ways Lifestyle Coaches can address HRSN to support participant success in the National DPP lifestyle change program:
- Tailor recruitment outreach to populations of focus.
- Enhance the National DPP lifestyle change program curriculum to increase its effectiveness for a specific cultural community or translate the curriculum into another language. Newly developed curricula must be submitted, reviewed, and approved by CDC prior to use. In addition, organizations that develop supplemental materials for an already approved CDC curriculum must submit those for review and approval. Information on how to do this is available here. Existing curriculum translations can be accessed on the Curriculum page of the Coverage Toolkit.
- Incorporate the use of additional low-literacy materials, such as visuals and materials written at a 6th grade level or below.
- Make it easy to participate in make-up sessions.
- Develop partnerships with other organizations to help address barriers to participation, such as with local food shelters, transportation, and child care services.
- Add additional class locations to meet the needs of participants, such as having a class at a church because members of that church are already familiar with the location and meet there regularly.
- Increase access to the National DPP lifestyle change program by offering a combination of in-person, online, distance learning, and/or distance learning via telephone delivery of the program.
- Facilitate social connections between program participants.
- Use supplementary experiences to address HRSN, such as addressing food security by making healthy food available at each session.
To learn more about Minnesota’s experience engaging participants and addressing HRSN, please see this video. To learn more about recruitment and retention strategies for the National DPP lifestyle change program, please visit the Recruitment and Referral page and the Retention page of the Coverage Toolkit.
Populations of Focus for the Medicare Diabetes Prevention Program (MDPP)
Tailoring recruitment outreach and the program curriculum for specific populations of focus can increase the relevancy of the National DPP lifestyle change program for the population. CDC, CMS, and NACDD have hosted multiple webinars on working with populations of focus in the Medicare Diabetes Prevention Program (MDPP), including African American and Asian American populations; Hispanic, Latino/a, and Spanish origin populations; and men, dual eligible, and people living with disabilities. The webinars and the accompanying summaries can be found on the Populations of Focus tab on the MDPP Implementation Resources page of the Coverage Toolkit.
Scaling the National DPP Lifestyle Change Program in Underserved Areas
From 2017-2022, CDC’s 1705 grants provided funding to 12 organizations to build out the National DPP infrastructure in underserved areas to ensure that all adults with prediabetes, or at high risk for type 2 diabetes, have the opportunity to enroll in a CDC-recognized evidence-based lifestyle change program. In June 2023, NACDD hosted a Virtual Showcase to highlight the successes of these organizations. The following presentations highlighted the importance of considering health equity when delivering the National DPP lifestyle change program to populations of focus.
- Dr. Leandris Liburd, Office of Health Equity (OHE), Acting Director, Centers for Disease Control and Prevention – recording and slides
- In this presentation Dr. Liburd defined commonly used health equity terms. She discussed health equity intervention and action principles that can be applied to diabetes prevention.
- Black Women’s Health Imperative (BWHI) – recording and slides
- Presenters: Paula Green-Smith and Leneé Reedus-Carson
- This presentation described BWHI’s work with its seven affiliate organizations in Alabama, Indiana, Michigan, Tennessee, and Texas. BWHI highlighted several of the innovative approaches used to increase the availability of the National DPP lifestyle change program for identified populations of focus.
- The Balm in Gilead – Southeast Diabetes Faith Initiative – recording and slides
- Presenters: Pamela Price, Deputy Director, The Balm in Gilead and Tanya Henderson, Project Director, The Balm in Gilead
- This presentation described The Balm in Gilead’s Southeast Diabetes Faith Initiative with 52 local affiliate sites across Alabama, Florida, Georgia, Mississippi, North Carolina, South Carolina, and Virginia. This talk specifically highlighted their work with African Americans and older adults, connection with community organizations, and development of key partnerships.
- National Alliance for Hispanic Health (NAHH) – recording (beginning at 21:24) and slides
- Presenters: Paul Baker, Managing Director for Programs, NAHH and Mayra Mendoza, Chronic Care Quality Manager and Deputy Chief Outreach and Wellness Officer, Project Vida Health Center
- This presentation described NAHH’s work with its nine affiliates across California, Florida, Nebraska, Texas, Nebraska, and Washington, D.C. NAHH highlighted the strategies used to provide the National DPP lifestyle change program to underserved Hispanic communities in Texas.
In addition, CDC’s Using Program Supports to Enhance the National DPP Lifestyle Change Program Webinar, highlights the key efforts to scale the National DPP lifestyle change program in areas that are underserved, discusses the partners in that effort, and provides an overview of the evaluation framework for the project. Along with CDC partners, the CDC presents a key case study from the DP17-1705 work, Implementing Program Supports to Retain Participants from Populations of Focus in the National DPP Lifestyle Change Program. Furthermore, CDC shares approaches from organizations that used various types of program supports to help reinforce information in the program curriculum, remove barriers to participation, address social determinants of health, and promote social support.
Examples of Addressing HRSN Through the National DPP Lifestyle Change Program
The COVID-19 public health emergency exposed existing weaknesses in how HRSN are addressed and, as such, health equity has become a high priority across the nation. One of the U.S. Department of Health and Human Services’ (HHS) Healthy People 2030’s five goals is specifically related to SDOH: “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.” Likewise, states are engaging in work to address HRSN through a variety of methods and partnerships.
This section will outline examples from states and organizations that are addressing HRSN in various ways that impact engagement with the National DPP lifestyle change program.
AAPCHO
The Association of Asian Pacific Community Health Organizations (AAPCHO) serves Pacific Islanders by collaborating with local communities, federally qualified health centers (FQHCs), and other organizations to improve the health of Pacific Islanders. Through the Pacific Islander Diabetes Prevention Program (PI-DPP), AAPCHO provides a CDC-recognized diabetes prevention program that is tailored to Pacific Islanders. Within that program, AAPCHO provides participants with assistance and program supports to address HRSN uniquely faced by this population.
On July 21, 2021, AAPCHO, in collaboration with other partners, held a webinar to explore strategies for HRSN screening and building effective practices to begin addressing SDOH through outreach and enabling services.
Alaska
Alaska offers the National DPP lifestyle change program through three delivery modalities: in-person, online, and distance learning via telephone. The online and distance learning via telephone programs are available to all eligible Alaskans free of cost. The distance learning via telephone delivery option through InquisitHealth includes one-on-one phone consultations with a Lifestyle Coach. This option provides program access to individuals living with limited broadband internet or phone data.
Illinois
Illinois is advancing Medicaid participant enrollment in the National DPP lifestyle change program by better understanding the challenges beneficiaries have related to participation and retention. Current initiatives include holding listening sessions to better understand what factors would encourage participants to stay in the program and what skills they would like to develop. The Illinois Department of Public Health is also utilizing grant funding to build a community advisory group, which involves selecting National DPP lifestyle change program graduates to serve as community advisors and develop strategies to improve access to the program.
To learn more about Medicaid coverage of the National DPP lifestyle change program in Illinois, see Illinois’ State Story of Medicaid Coverage. For more information on recruitment, referrals, and retention of Medicaid beneficiaries in the National DPP lifestyle change, visit the Recruitment and Referral page and the Retention page of the Coverage Toolkit.
Maryland
To better address HRSN, Maryland Department of Health has connected each of their managed care organizations (MCOs) with regional CDC-recognized organizations to discuss and develop plans for collaboration. Together they have developed an eligibility algorithm and are creating pathways to work with health care providers to adapt initiatives to better align with a patient-centered point of view. This includes developing referrals to community-based organizations that address HRSN.
In addition to their referral system, Maryland is also using CHWs as Lifestyle Coaches to deliver the National DPP lifestyle change program. CHWs typically act as a member of the care delivery team supporting health equity by providing care education, social service navigation, and coordination, while also organizing peer support and performing outreach. In Maryland, CHWs are certified by accredited training programs.
For additional information about Maryland’s involvement with the National DPP lifestyle change program, see the Maryland Medicaid Demonstration Project page of the Coverage Toolkit.
Medicaid Demonstration Project
During the Medicaid Coverage for the National DPP Demonstration Project, Lifestyle Coaches met the needs of program participants by incorporating low-budget recipe suggestions and culturally relevant food and exercise strategies. They also allowed for program flexibility by implementing flexible make-up sessions that were held individually, in small groups, and over the phone; and allowed participants to bring family members or caregivers to class. Finally, the Lifestyle Coaches coordinated group outings such as fitness classes, group walks/runs, local grocery store tours, and trips to local farmers’ markets.
Some of the participating MCOs and accountable care organizations (ACOs) addressed the needs of Medicaid beneficiaries by providing transportation vouchers, ride-shares, and/or free or reduced-price childcare. CDC-recognized organizations indicated that addressing these HRSN was more effective at facilitating participant retention than offering monetary program supports.
For more information, see the Medicaid Coverage for the National DPP Demonstration Project Retention Brief.
Mississippi
The Mississippi State Department of Health has collaborated with their Department of Agriculture to expand the Supplemental Nutrition Assistance Program (SNAP) program benefits and deliver additional food to people participating in the National DPP lifestyle change program and other evidence-based programs such as Diabetes Self-Management Education and Support (DSMES). As part of this initiative, Mississippi has worked with farmers’ markets to support locations near community centers and prepare community food subscription programs for individuals in need.
North Carolina
The North Carolina Department of Health and Human Services (NCDHHS) launched its Healthy Opportunity Pilots program in February 2022 through an 1115 waiver. These pilots cover the cost of 29 interventions, including the National DPP lifestyle change program, for select counties enrolled in the regional pilots. These pilots also address other HRSN such as housing stability, transportation, food security, interpersonal violence, and toxic stress. The goal of the pilots is to create and evaluate a systematic approach to integrate and finance evidence-based, non-medical interventions.
NCDHHS released several resources to learn more about the program including a fact sheet, policy paper, and FAQ document. Additional resources can be found on the Healthy Opportunities Pilots website.
Rhode Island
The Rhode Island Department of Health is implementing multiple layers of screening for and addressing HRSN among National DPP lifestyle change program participants. In partnership with the state’s ACOs and CDC-recognized organizations, it is focusing on addressing HRSN-related factors that impact program participation, as well as needs that go beyond program goals. The Rhode Island Department of Health’s planning team outlined a screening and referral workflow to identify HRSN touch points. For example, Community Health Network (CHN) patient navigators serve a key role in identifying HRSN during both enrollment and follow-up calls. Rhode Island plans to scale National DPP lifestyle change program access and utilization by increasing the number of CHWs and Lifestyle Coaches that are trained in these areas.
Virginia
The Virginia Department of Medical Assistance Services (Virginia Medicaid) has engaged in discussions with MCOs on how individuals with HRSN can be identified. Virginia Medicaid is also working to identify individuals that are eligible for the National DPP lifestyle change program by linking primary care physicians to National DPP lifestyle change program referrals via automated orders through their electronic health record (EHR). This process allows collaborative partners to access HRSN screenings performed directly by those who care for the individuals.
Within the recruitment process, Virginia Medicaid is also creating initiatives to ask and determine what would prevent participants from participating in the National DPP lifestyle change program. This initiative allows Virginia Medicaid to assess individual HRSN. This initiative is supported by participating MCOs that want to improve enrollment and retention in the National DPP lifestyle change program.
In Virginia’s model, CHWs directly market the National DPP lifestyle change program to target populations through planned community activities, health fairs, local churches, and social media campaigns. CHWs utilize the 3-2-1 method for participant outreach – 3 phone calls, 2 texts, and 1 email. CHWs also utilize the PRAPARE tool to identify potential health-related social needs (HRSN) prior to the first session. To learn more about HRSN screening tools, see the Leveraging State and National Health Equity Initiatives page of the Coverage Toolkit.
In addition to this work, Virginia is working to roll out an initiative that provides healthy food vouchers and childcare stipends to participants in the National DPP lifestyle program as they meet predetermined milestones.
Health Equity and COVID-19
In many ways, the COVID-19 pandemic highlighted and exacerbated existing health inequities across the nation. This section will discuss the connection between COVID-19 and type 2 diabetes and the impact of COVID-19 on the National DPP lifestyle change program.
The Connection Between COVID-19 and Type 2 Diabetes
Emerging research increasingly shows that individuals with prediabetes and type 2 diabetes face a greater chance of experiencing severe complications from COVID-19, including hospitalization, ventilation, and death. Public health emergencies could also exacerbate other health-related challenges for persons living with prediabetes and type 2 diabetes, such as reduced access to medical care, decreased physical activity, and decreased food security.
Rates of food insecurity more than tripled from 10.5% in 2019 to 38.3% in March and April 2020, coinciding with the beginning of the COVID-19 pandemic and public health emergency. This 2020 study also found that 54% of Black respondents, 45% of Native American respondents, and 53.4% of Hispanic respondents reported moderate to high food insecurity.
Individuals with obesity have increased risk for severe illness from COVID-19 as well. People who are overweight may also be at increased risk. During the COVID-19 pandemic, it was reported that having obesity may triple the risk of hospitalization due to COVID-19 infection.
Additional information on the connections between COVID-19 and type 2 diabetes that underscore the need for chronic disease prevention and management can be found in this report released by NACDD and Gardner Policy Institute.
The Impact of COVID-19 on the National DPP Lifestyle Change Program
At the start of the COVID-19 pandemic, many states rapidly pivoted from in-person programming to online or distance learning delivery of the National DPP lifestyle change program. In addition to this transition, many states faced Lifestyle Coach staffing shortages. Strategies utilized by states to address Lifestyle Coach shortages included:
- Using a team Lifestyle Coaching strategy, where two Lifestyle Coaches were assigned to each cohort. This helped ensure continuity of the cohort if a Lifestyle Coach was unable to attend a session or continue teaching a cohort.
- Utilizing National DPP State Quality Specialists (SQS), a network of specialists at the state level trained by CDC to provide technical assistance in addition to the assistance provided by the National Diabetes Prevention Program Customer Service Center, to address Lifestyle Coach staffing shortages.