Health Equity → Priority Populations → Disability and Inclusion
Inclusion of People with Disabilities
According to the CDC, in the United States, one out of four people or roughly 61 million adults, live with a disability. Statistics also show that individuals living with a disability are more likely to have heart disease, stroke, diabetes, or cancer, less likely to engage in aerobic physical activity, and have higher rates of obesity. The National Diabetes Prevention Program (National DPP) lifestyle change program can help reduce the incidence of some of these outcomes, however, participation is contingent upon ensuring the program is inclusive for all participants. This page will help to define inclusion related to working with those with disabilities, spotlight organizations who are leading the way, and provide resources to help organizations develop inclusive National DPP lifestyle change programs. This page is divided into the following sections:
- Disability and Inclusion in the National DPP Lifestyle Change Program
- Roadmap 2 Inclusion
- Creating Inclusive Programs: 1705 National Organization Work
Disability and Inclusion in the National DPP Lifestyle Change Program
Disability and Diabetes
Disability is defined as, “any condition of the body or mind that makes it more difficult for the person with the condition to do certain activities and interact with the world around them.” There are many types of disability, which can include disabilities related to an individual’s vision, hearing, movement, thinking, learning, communicating, and many more. It is important to remember that not all disabilities are easy to see or recognize.
According to CDC’s Disability and Diabetes Prevention page, about 1 in 6 people with disabilities in the United States had been diagnosed with diabetes in 2020 (with variation in rates across states, races/ethnicities, and age group) compared to 1 in 14 people without disabilities. Addressing this disparity will require a reframing of how we view disability. Traditionally, most individuals look at disability through the Medical Model lens, which views disability as a problem within the person that must be fixed and restricts participation for the individual as a result of their disability. The Medical Model focuses on disability treatment and/or cures for that individual. To promote inclusion, individuals must also view disability through the Social Model lens, which instead focuses on accessibility of the program or environment. In the Social Model, a person is disabled when the program or environment does not accommodate their unique functional level. In other words, a person cannot participate because the program or environment itself is not accessible to them. Keeping an orientation towards the Social Model requires the basis for all strategies to center on creating societies and resources which are inclusive to all. Approaches should focus on aspects such as barrier removal and anti-discrimination policies and legislation.
Inclusion in the National DPP Lifestyle Change Program
How inclusion is defined can vary. The National Center on Health, Physical Activity and Disability (NCHPAD), along with other national advocates, experts, and individuals with disabilities, have created a definition for inclusion that has an orientation towards public health and communities, shown in the call out box below.
Inclusion means to transform communities to ensure all community members:
- Are presumed competent;
- Are recruited and welcome as valued members of their community;
- Fully participate and learn with their peers; and
- Experience reciprocal social relationships.
GRAID Framework
One approach to increase inclusion of people with disabilities in the National DPP lifestyle change program is incorporating the five domains of inclusion. These domains are based on an evidence informed framework called the Guidelines, Recommendations, Adaptations, Including Disability or GRAIDs. The GRAIDs were developed by NCHPAD and other national partners in the field of disability and health to provide guidance on how to adapt evidence-based programs, like the National DPP lifestyle change program, to fully include participants with disabilities. These domains include:
- Built Environment: Use of structural features such as ramps, signs, clear paths, lighting, firm and stable floor surfaces, and more.
- Service: Person-to-person assistance such as providing peer assistance, transportation, or communication aids.
- Instruction: Incorporating instructional opportunities for staff and family to better include individuals with disabilities, such as webinars, seminars, or trainings.
- Equipment and Technology: Devices or resources to allow for participation by all individuals, including specialized utensils, automatic doors, communications devices, accessible web sites, and more. A list of examples relevant to the National DPP lifestyle change program are available at the Prevent T2 for All Inclusive Nutrition and Physical Activity Toolkit. This list of adapted equipment focuses mainly on food preparation and cooking as well as physical activity.
- Policy: Policies, procedures, regulations, or rules which influence behavior and create a more inclusive environment.
9 Guidelines for Disability and Inclusion
The Commit to Inclusion webpage, created by NCHPAD and partners as part of a national campaign to increase the inclusion of people with disabilities in physical activity programs and policies, also provides useful resources for organizations and communities to understand and improve program and environmental inclusion. The foundation of the campaign are the 9 Guidelines for Disability Inclusion. Much like the GRAID framework, these guidelines provide guidance to communities to ensure that any physical activity or health promotion programs or policies that are enacted include people with disabilities. These Guidelines are outlined in an implementation manual titled, Guidelines for Disability Inclusion in Physical Activity, Nutrition, & Obesity Programs and Policies which provides information on why the guidelines are important, how to accomplish them, and examples and resources related to each guideline. Descriptions for each of the guidelines (found on page 2 in the above document) are provided below.
- Objectives Include People with Disabilities: Program objectives should explicitly and unambiguously state that the priority population includes people with a range of different disabilities.
- Involvement of People with Disabilities in Development, Implementation and Evaluation: Program development, implementation, and evaluation should include input from people with a range of different disabilities and their representatives.
- Program Accessibility: Programs should be accessible to people with disabilities and other users socially, behaviorally, programmatically, in communication, and in the physical environment.
- Accommodations for Participants with Disabilities: Programs should address individual needs of participants with disabilities through accommodations that are specifically tailored to those needs.
- Outreach and Communication to People with Disabilities: Programs should use a variety of accessible methods to outreach and promote the program(s) to people with disabilities.
- Cost Considerations and Feasibility: Programs should address potential resource implications of inclusion (including staffing, training, equipment, and other resources needed to promote inclusion).
- Affordability: Programs should be affordable to people with disabilities and their families, personal assistants, and caregivers.
- Process Evaluation: Programs should implement process evaluation that includes feedback from people with disabilities and family members, personal assistants, caregivers or other representatives, and a process for making changes based on feedback.
- Outcomes Evaluation: Programs should collect outcomes data, using multiple disability-appropriate measures.
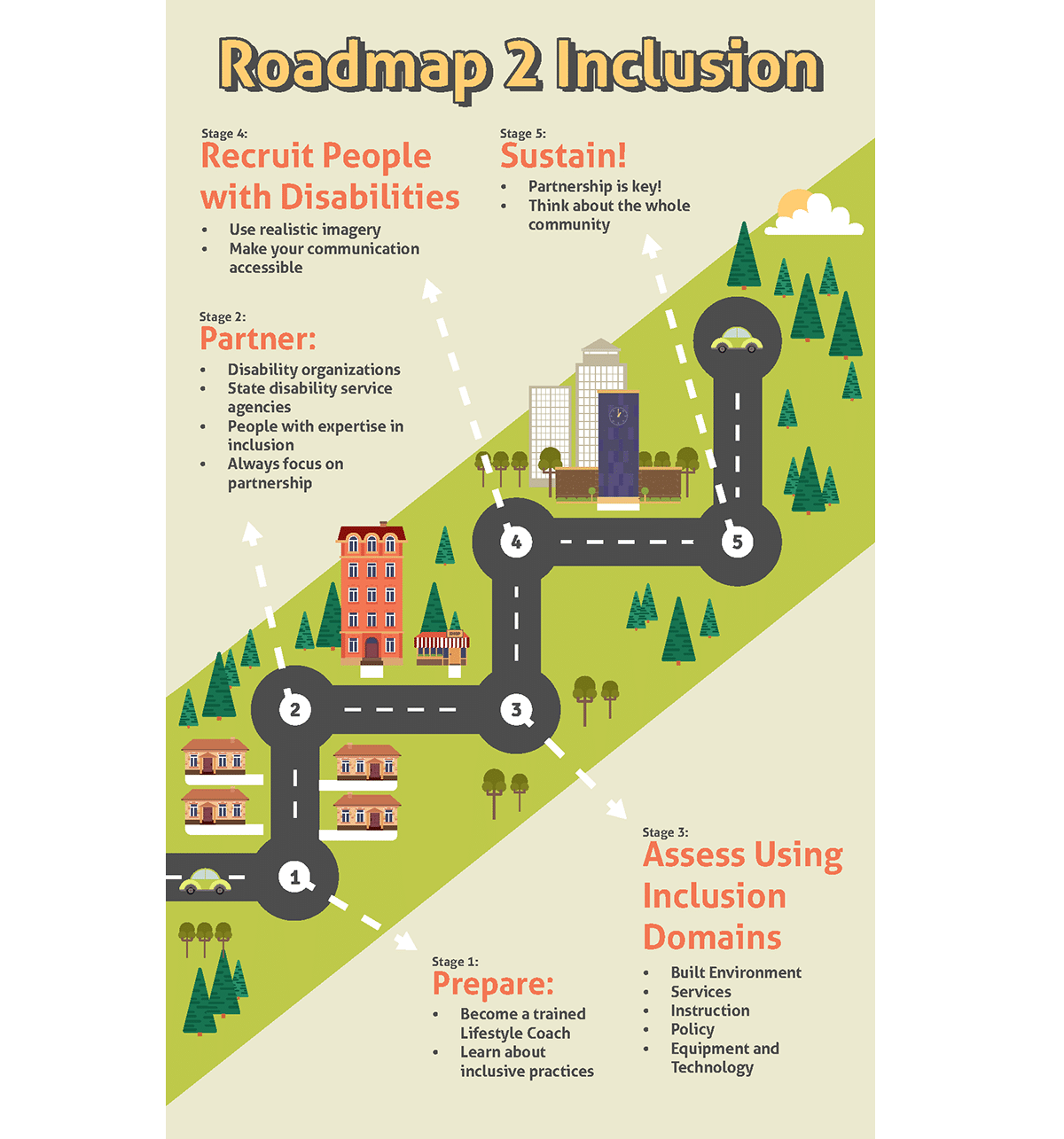
Roadmap 2 Inclusion
The newly released Roadmap 2 Inclusion graphic, developed by The Lakeshore Foundation, describes five stages organizations can use to ensure that their delivery of the National DPP lifestyle change program is inclusive of individuals with disabilities. The five stages are 1) Prepare, 2) Partner, 3) Assess Using Inclusion Domains, 4) Recruit People with Disabilities, and 5) Sustain. Hover over the green plus signs ![]() on the image below to learn more.
on the image below to learn more.
Additional Resources to Support Inclusive Delivery of the National DPP Lifestyle Change Program
For additional information and resources related to disability inclusion, visit the following websites:
- The Lakeshore Foundation: a nonprofit, accessible fitness center and Paralympic and Olympic training center that served as a DP17-1705 national partner organization. Lakeshore provides opportunities for people with a physical disability or chronic health condition to be active through physical activity, research, advocacy, and policy.
- NCHPAD: a CDC-funded public health practice and resource center on health promotion for people with disabilities. NCHPAD seeks to achieve health equity for people with disabilities and chronic conditions through increased participation in all types of physical, wellness, and social activities.
- NCPHAD has also developed an informational video on How to Recruit People with Disabilities for Health Programs.
- The Retention page of the Coverage Toolkit details program adjustments made by partners in Montana to be more inclusive for participants, including training Lifestyle Coaches on disabilities, simplifying language in participant materials and resources, and engaging family and support-systems in National DPP lifestyle change program efforts.
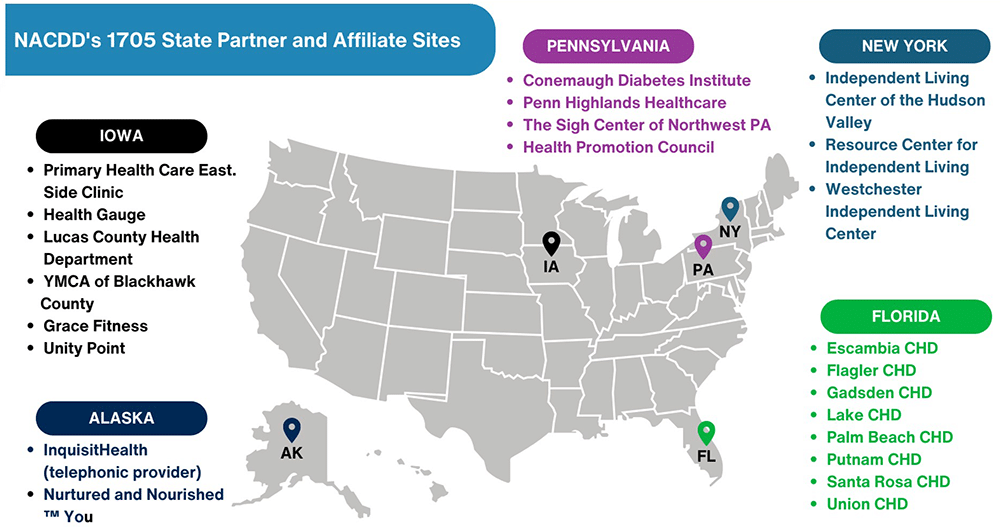
Creating Inclusive Programs: 1705 National Organization Work
From 2017-2022, NACDD was funded as a recipient of CDC’s DP17-705 cooperative agreement, “Scaling the National DPP in Underserved Areas”, to reach people with disabilities with an inclusive National DPP lifestyle change program (to learn more about the CDC’s 1705 grant program, please visit the Additional Initiatives page). NACDD’s national partners in this work include the Lakeshore Foundation, ProVention Health Foundation, InquisitHealth, Virgin Pulse/Welltok, PAC Software, and Hope 80/20. State partners included Alaska Department of Health and Social Services, Iowa Community Hub, Florida Department of Health, New York Association of Independent Living, and Health Promotion Council (PA). Additional state partners and affiliate sites are listed in the map below.
In addition to creating inclusive programs, the objectives of the project included:
- Increase the number of new CDC-recognized organizations that offer the National DPP lifestyle change program
- Increase referrals for the National DPP lifestyle change program by working with health system partners
- Market the National DPP lifestyle change program to drive enrollment
- Retain participants in the National DPP lifestyle change program
- Reimburse for delivery of the National DPP lifestyle change program through public and private payers and employers, and support Medicare Diabetes Prevention Program (MDPP) suppliers
NACDD’s examples of partnership initiatives that took place during the project are provided in the table below.
Technical Assistance Grants
NACDD, in partnership with the Lakeshore Foundation, offered technical assistance to support sustainability through mini-grants. These grants (available only during the DP17-1705 grant cycle) aimed to increase DP17-1705 state affiliate capacity to be accessible and inclusive to adult National DPP lifestyle change program participants with physical and/or sensory disabilities. Conemaugh Health (PA), Palm Beach County Health Department (FL), and CHP Community (IA) received these grants to purchase, store, and distribute wheelchair-accessible scales, develop an inclusive equipment resource catalog, and foster partnerships with local rehabilitation providers and Arc chapters (community-based organizations advocating for and with people with intellectual and developmental disabilities and serving them and their families) to recruit and enroll people with disabilities.
Documenting Program Success
NACDD partnered with the Alaska Department of Health and InquisitHealth to capture a success story video of an InquistHealth telephonic National DPP lifestyle change program participant from rural Alaska. The participant was referred to the program by their health care provider after experiencing two heart attacks and receiving bloodwork results in the prediabetes range. Through participating in the program, the individual lost almost 60 pounds and can now enjoy activities with less stress and fatigue. Additional information on Alaska’s delivery modalities for the National DPP lifestyle change program are available on the Addressing HRSN Through the National DPP Lifestyle Change Program page of the Coverage Toolkit. The success story was also utilized by the Alaska Department of Health in their Fresh Start campaign.
Online Delivery
NACDD partnered with the ProVention Health Foundation to offer the Health and Lifestyle Training (HALT) diabetes software platform that enables any CDC-recognized organization to offer the National DPP lifestyle change program online. The HALT platform empowers CDC-recognized organizations to expand network capacity and affordable access to the National DPP lifestyle change program. NACDD provided users with onboarding training, recruitment and enrollment support, and customized marketing materials. Throughout the project, NACDD trained and onboarded 14 CDC-recognized organizations onto the HALT platform resulting in the enrollment of 245 participants.
Outcomes
Through the work on the DP17-1705 project, NACDD and partners have:
- Worked across five states to support 31 programs in applying for and becoming CDC-recognized to offer the National DPP lifestyle change program.
- Supported four sites in becoming MDPP providers and four sites in becoming Medicaid providers.
- Supported the enrollment of over 1,400 participants with prediabetes into the National DPP lifestyle change program. Twelve percent of participants reported having a disability and achieved an average weight loss of 9.7%, compared to the national average of 5.2%.
- Trained and onboarded 12 CDC-recognized organizations onto the HALT platform, resulting in 10 cohorts with 140 participants.
- Provided at least 10 lifestyle coach trainings to 50+ lifestyle coaches, with a focus on inclusion for people with disabilities.
- Annually provided training, technical assistance, and one-on-one support to the five states and 20+ CDC-recognized organizations to successfully implement work plans addressing the five program objectives listed above, with a focus on inclusion for people with disabilities.
- Created multiple resources and toolkits for states and CDC-recognized organizations to use in reaching and enrolling people with disabilities into the National DPP lifestyle change program (training, intake form, and data collection support; marketing materials; and partnership engagement tools).
Additional information on NACDD partners, success stories, and resources from the DP17-1705 initiative are available on the NACDD Scaling the National DPP in Underserved Areas Diabetes page.









