Medicaid → Medicaid Coverage
Medicaid Coverage
The first page in this Medicaid Coverage section outlines how public health professionals, including state health departments, can collaborate with Medicaid to make the case for coverage of the National Diabetes Prevention Program (National DPP) lifestyle change program.
The second page is the Policy to Payment Roadmap, an overview of the activities involved in coverage and operationalization of the National DPP lifestyle change program benefit in Medicaid.
The next three pages outline ways state Medicaid and federal Medicaid matching funds can be leveraged to cover the program in Medicaid.
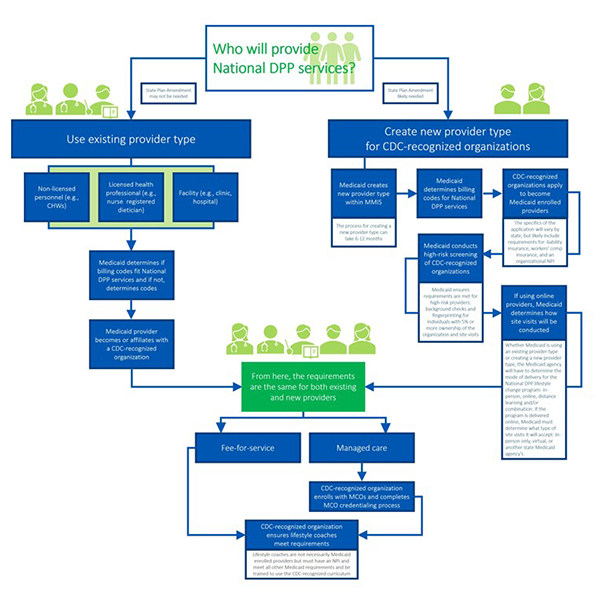
The final two pages describe considerations for determining the Medicaid enrolled provider type that will be delivering the program, and which states are offering the National DPP lifestyle change program as a Medicaid covered benefit.
Please see the Elevator Pitch for Medicaid Coverage of the National DPP Lifestyle Change Program document for talking points on how coverage of the program can benefit Medicaid and the communities being served.
This section is written for public health professionals to provide guidance for working with their Medicaid colleagues to make the case to cover the National DPP lifestyle change program.
The Policy to Payment Roadmap provides a high-level overview of activities that lead to coverage and operationalization of the National DPP lifestyle change program in Medicaid, based on the experiences of states that have achieved Medicaid coverage of the program. It also links to Coverage Toolkit pages where you can learn more about each activity.
This page describes the role a state’s legislature can play in establishing Medicaid coverage for the National DPP lifestyle change program, and how stakeholders can engage with the legislature. It also provides the text of National DPP related legislation from numerous states.
Generally, if the policies or processes a state intends to implement for Medicaid coverage of the National DPP lifestyle change program can be accomplished through the Medicaid State Plan, a state must use the Medicaid State Plan to attain federal Medicaid matching funds for the program. This section provides information on how the National DPP lifestyle change program can be included in the Medicaid State Plan, when a State Plan Amendment (SPA) is necessary, and multiple state examples.
If the policies or processes a state intends to implement for Medicaid coverage of the National DPP lifestyle change program cannot fit within the existing Medicaid program requirements included under the Social Security Act, an 1115 waiver may be an appropriate avenue to attain federal Medicaid matching funds for the program. This section provides information on how the National DPP lifestyle change program can be included in an 1115 waiver, along with state examples.
State Medicaid agencies must decide who will deliver the National DPP lifestyle change program to Medicaid beneficiaries. States have two options: they can use an existing provider type to deliver the program or they can create a new provider type.
This section provides a map showing which states have Medicaid coverage for the National DPP lifestyle change program, and describes key details of that coverage.