Medicaid → State Stories of Medicaid Coverage → Montana
Montana’s State Story of Medicaid Coverage
Establishing Coverage
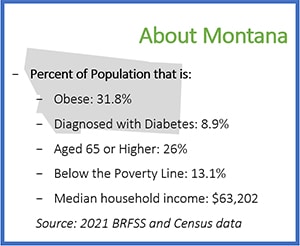
Montana began exploring Medicaid coverage of the National Diabetes Prevention Program (DPP) lifestyle change program in 2011. The process started by convening individuals from the Montana Diabetes Program, administered by the Public Health and Safety Division, and Montana Medicaid. During this first meeting, administrators, bureau chiefs, and program staff discussed the following evidence supporting the effectiveness of the National DPP lifestyle change program:
- The diabetes disease burden for Medicaid enrollees, demonstrated by a Medicaid survey and Behavioral Risk Factor Surveillance System data
- Randomized control trials showing the effectiveness of the program in preventing diabetes and improving health outcomes (program effectiveness studies can be found here)
- Successful program results in Montana
- The demonstrable cost effectiveness or cost savings of the program (cost effectiveness studies can be found here and here)
A key step in advancing Medicaid coverage of the National DPP lifestyle change program was the collaborative relationship between the Public Health and Safety Division and Montana Medicaid, which are both housed within the Montana Department of Public Health and Human Services and located in the same building. The two groups worked together on a Centers for Medicare and Medicaid Services (CMS) Medicaid Incentives to Prevent Chronic Diseases (MIPCD) grant from 2011‒2016, and Medicaid created a “liaison to public health” position in 2014. Staff from both groups met weekly to discuss progress and address the needs of the MIPCD grant.
In 2012, Montana made amendments to its Medicaid administrative rules on general and preventive Medicaid services and submitted a State Plan Amendment (SPA) to CMS adding a benefit that encompassed the National DPP lifestyle change program. The SPA was updated in 2016 and allows the following:
- A. Services to prevent diabetes and cardiovascular disease provided to people at risk for diabetes and cardiovascular disease:
- Group nutrition counseling to prevent diabetes and cardiovascular disease
- B. Providers
- Physicians,
- Mid-level practitioners,
- Registered dieticians who also hold a current Montana license as a nutritionist,
- Hospitals,
- Federally Qualified Health Centers,
- Rural Health Clinics,
- Indian Health Services/Tribal Health Services,
- Groups/Clinics, or
- Public Health Departments.
Listed providers will provide services for reimbursement under the diabetes and cardiovascular disease prevention program. Services for the program are limited to group nutrition and lifestyle counseling to prevent diabetes and cardiovascular disease.
A physician or mid-level practitioner supervising a provider not listed above, such as a licensed nurse, a certified diabetes educator, or an exercise physiologist, will assume professional liability for care of the patient and will furnish services within his or her scope of practice under state law.
Results
General Results
Over the past 10 years, Montana’s National DPP lifestyle change program has served 8,800 Medicaid and non-Medicaid participants. Program results from 2008‒2016 show that 64% of participants met their goal of 150 minutes of physical activity per week, 47% lost at least 5% of their body weight, 33% lost at least 7% of their body weight, and 23% lost at least 9% of their body weight after ten months in the program (when considering participants who attended four or more sessions). The average weight lost per participant was 12 pounds. While these results are not Medicaid specific, they demonstrate the success of the National DPP lifestyle change program overall in Montana.
Medicaid Population Results
A study conducted in 2012‒2013, comparing the results of Medicaid and non-Medicaid participants in Montana, revealed that significant weight loss was achieved among Medicaid members even though Medicaid participants achieved lower weight loss compared to non-Medicaid participants (an average of 6.6 pounds of weight loss compared to 11.9 pounds in the non-Medicaid group). The study results showed the Medicaid beneficiaries can be recruited and retained into the National DPP lifestyle change program.
Return on Investment
Montana has found the average participant cost to cover the National DPP lifestyle change program for Medicaid and Medicare is $500 per year, which is significantly less than the estimated cost of providing diabetes care over 3-year period ($8,010 or roughly $2,670 per year).
An evaluation of the return on investment from offering the National DPP lifestyle change program to a cohort that included some Medicaid participants that was experienced by the Providence Medical Group Endocrinology, Diabetes and Nutrition Center can be found here.
Program Features Unique to Montana
Telehealth Delivery
Montana uses several approaches to deliver the National DPP lifestyle change program. In addition to on-site program delivery, Montana has developed a robust telehealth delivery system, where the National DPP lifestyle change program can be delivered simultaneously to an on-site group and a remote group, or just to a remote group. The National DPP lifestyle change program is currently offered at 19 on-site locations, 13 telehealth sites, and three satellite sites.
Montana conducted a study on telehealth delivery of the National DPP lifestyle change program, which found no statistical differences in the number of sessions attended or weight loss between the telehealth and the onsite groups. Montana’s telehealth study can be found here.
The keys to success of Montana’s telehealth delivery system include:
- Finding a remote site that is a quiet location with the right technology
- Having the lifestyle coach make an in-person visit to the remote location to establish rapport with the group
- Setting up the system so that the lifestyle coach can see the remote participants
- Having the lifestyle coach respond to remote participants’ journals each week
- Having a telehealth site coordinator at the remote site to set up the room, weigh participants, collect journals, assist in group discussions, and encourage participants to engage in the session
- Giving the remote participants time to have their own group discussion and to then share their learnings with the on-site participants
Montana’s telehealth delivery system allows a larger number of Medicaid enrollees to participate in the National DPP lifestyle change program and still meet Montana’s SPA requirement that lifestyle coaches be trained professionals. For example, if a medical professional isn’t available in a remote geographic area, a telehealth site virtually accessing a licensed lifestyle coach can be opened and supported by a telehealth site coordinator who does not need to be a medical professional.
Rigorous Evaluation
Montana consistently publishes studies to evaluate the effectiveness of its delivery of the National DPP lifestyle change program. In addition to the Medicaid population study and the telehealth study already mentioned, Montana has studied program adaptations for the Medicaid population, such as entering a joint-use agreement with a hotel pool, providing farmer’s market tokens, giving participants cooking demonstrations, and developing alternate tracking tools for participants with low literacy skills. Montana also studied the effectiveness of the program for individuals with disabilities, the effects of financial incentives for program participants, and differences in program effectiveness based on age. Conducting and publishing these studies provides evidence to allow for program improvements and encourages others in and outside the state to cover the program.
To learn more about evaluation methods and examples of other states that have evaluated the National DPP lifestyle change program, please see the evaluation section of the Data, Reporting, and Evaluation page.
Recruitment & Referral
Montana conducts concerted recruitment efforts by proactively providing Medicaid providers and beneficiaries information on the National DPP lifestyle change program. Montana’s recruitment strategies have included mailings and direct phone calls to both providers and beneficiaries, with a particular emphasis on connecting with providers. A full description of Montana’s recruitment strategies can be found here.
In Montana, individuals can self-refer to the National DPP lifestyle change program based on their CDC/ADA Prediabetes Risk Test results alone. However, all participants are required to obtain medical clearance from their health care provider prior to beginning the program and a blood test is collected at baseline, six months, and twelve months.
Reimbursement
Montana Medicaid uses a fee-for-service reimbursement model, meaning that Medicaid providers who offer the National DPP lifestyle change program are reimbursed directly by Medicaid on a per session basis. Effective September 1, 2018, Montana Medicaid reimburses $29.10 per individual per group session attended using the 0403T code. Medicaid reimburses for the National DPP lifestyle change program at the same rate for both in-person visits and those offered via telehealth. If a Medicaid beneficiary attending the National DPP lifestyle change program stops participating, they can re-enroll in the program as long as they are still Medicaid eligible and eligible for the program.
Coding and Billing
Specific claim submission requirements in Montana are based on whether the National DPP lifestyle change program is delivered by a public health entity or at a hospital. Requirements for claims submission vary by the type of entity providing the National DPP lifestyle change program. Providers have 365 days from the date of service to submit claims.
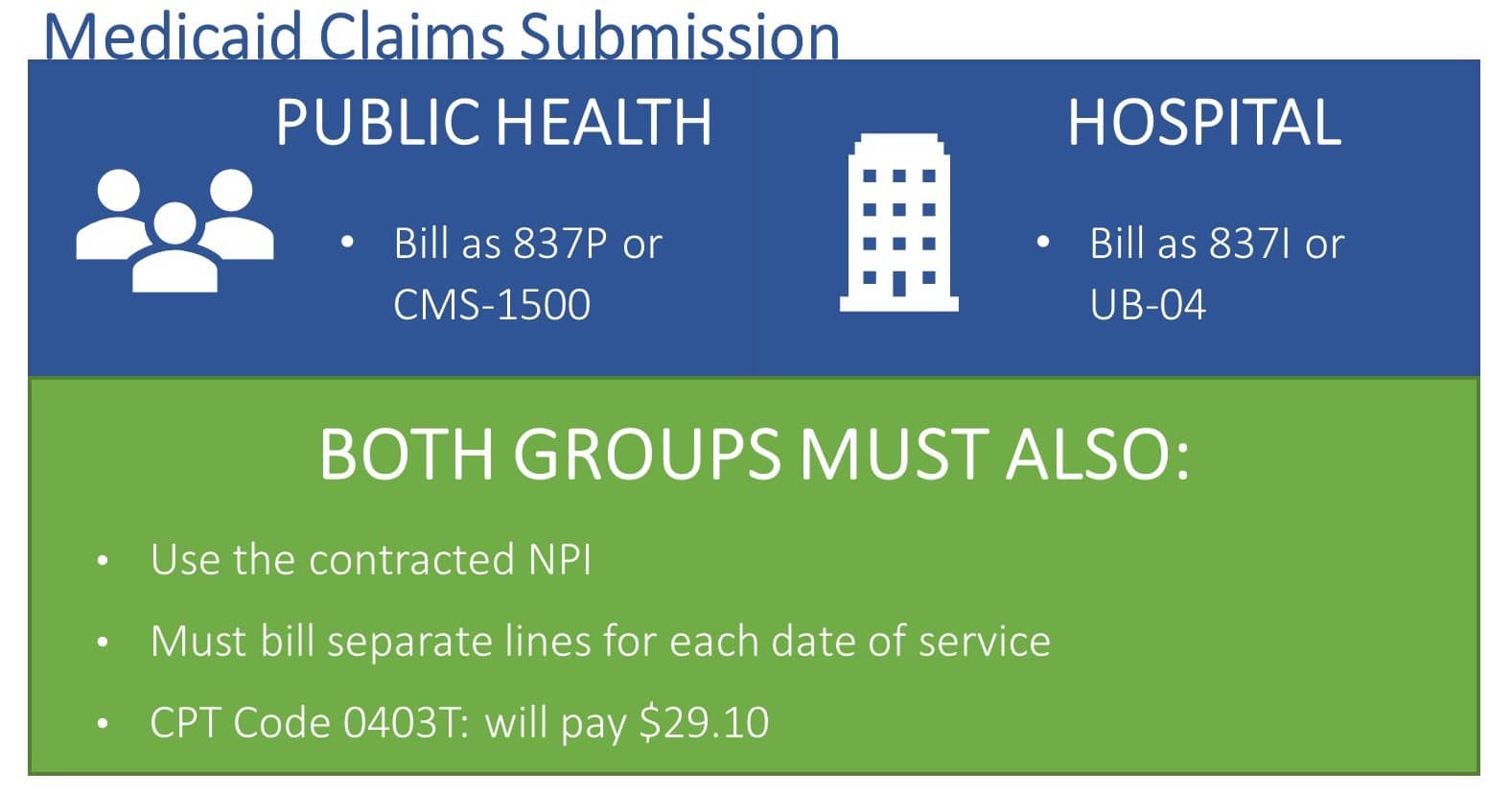
Medicaid providers who offer the National DPP lifestyle change program in Montana have found the Medicaid billing process to be difficult to learn. To help solve this issue, Montana’s Medicaid program staff are available via phone to provide answers to specific billing questions and Medicaid providers who offer the National DPP lifestyle change program have also been providing technical assistance to one another.
Data and Reporting
All 19 of the National DPP lifestyle change program sites contracted with the Montana Department of Public Health and Human Services use the same web-based data reporting system to track participant demographic information, data required by CDC, and indicators such as weight, tobacco use, medications, and BMI at the beginning of the program and after six and twelve months. The web portal allows lifestyle coaches to update the data from any location. The Montana Department of Public Health & Human Services can access de-identified outcomes from these data.
The National DPP site can use the data collected to gain recognition from the CDC’s Diabetes Prevention Recognition Program (DPRP). Montana has designed the system to collect and report the variables according to the CDC’s DPRP data dictionary. At this time, the Montana Diabetes Program does not report the data to Montana Medicaid.
Additional Resources
- Montana National DPP Lifestyle Change Program Story Map
- Montana Diabetes Program
- Telehealth Delivery of the Diabetes Prevention Program to Rural Communities
- Effectiveness of an Adapted Diabetes Prevention Program Lifestyle Intervention in Older and Younger Adults
- Expanding Health Insurance Coverage in California for the National Diabetes Prevention Program – see “Appendix 1: The Path to Medicaid Coverage for the DPP in Montana”
- Montana State Plan Amendment









