Screening and Identification for Medicaid Agencies and MCOs
States and Medicaid managed care organizations (MCOs) can identify prospective participants for the National Diabetes Prevention Program (National DPP) lifestyle change program based on participant eligibility criteria.
This page contains the following topics:
- Eligibility Requirements for the National DPP
- Medical Claims or Electronic Health Records
- Tracking Progress Through Claims
- Identification by Providers
- Health Information Exchange Engagement
Eligibility Requirements for the National DPP
To be eligible for referral to the National DPP lifestyle change program, individuals must meet the following requirements:
- All of a program’s participants must be 18 years of age or older. The program is intended for adults at high risk of developing type 2 diabetes.
- All of a program’s participants must have a body mass index (BMI) of ≥25 kg/m2 (≥23 kg/m2, if Asian American).
- All of a program’s participants must be considered eligible based on either:
- A blood test result within one year of participant enrollment. Blood test results may be self-reported for CDC recognition purposes. Participants enrolled in the Medicare Diabetes Prevention Program (MDPP) cannot self-report blood test results; lab results must be provided. Blood test results must meet one of the following specifications:
- Fasting glucose of 100 to 125 mg/dl (Centers for Medicare and Medicaid Services-CMS- eligibility requirement for MDPP participants is 110 to 125 mg/dl);
- Plasma glucose of 140 to 199 mg/dl measured 2 hours after a 75 gm glucose load;
- HbA1C of 5.7 to 6.4; or,
- Clinically diagnosed gestational diabetes mellitus (GDM) during a previous pregnancy (allowed for CDC recognition and may be self-reported; not allowed for MDPP participants); or
- A positive screening for prediabetes based on the Prediabetes Risk Test online. Note: The risk test is not an option for eligibility for MDPP participants.
- Participants cannot have a previous diagnosis of type 1 or type 2 diabetes prior to enrollment.
- Participants cannot be pregnant at time of enrollment.
- A health care professional may refer potential participants to the program, but a referral is not required for participation in a CDC-recognized program.
To be eligible for the National DPP lifestyle change program, individuals must have one of the blood test results described above, be previously diagnosed with gestational diabetes, or score positive for prediabetes on the CDC/ADA Prediabetes Risk Test. The CDC Diabetes Prevention Recognition Program (DPRP) standards require that at least 35% of a program’s participants be diagnosed with prediabetes through blood testing (or have a history of gestational diabetes). The remaining participants in the group can be considered eligible for the program based on their scores on the CDC/ADA Prediabetes Risk Test. The CDC/ADA Prediabetes Risk Test is a brief seven question survey that allows one to gauge their risk of having prediabetes. Regularly scheduled biometric screenings may be an opportunity to determine if an individual is eligible.
Medical Claims or Electronic Health Records
States and their MCOs have leveraged electronic health record data (EHR) and/or medical claims data to proactively identify individuals who are, or may be, eligible for the program. For instance:
- Maryland uses ICD-10 codes from claims data to identify individuals who fit the eligibility criteria. The codes are able to flag individuals who, for example, individuals who are overweight or obese, who have elevated glucose levels, or have a history of gestational diabetes. See the table below for a list of codes that can be used in this type of search.
- Denver Health and Hospital Authority (Denver Health) developed a patient registry based on EHR data. That registry included individuals at risk for type 2 diabetes based on program eligibility criteria. The registry was then used to conduct targeted recruitment and referral efforts. Denver Health is a Colorado-based safety net health system; nearly half of its National DPP lifestyle change program participants had Medicaid coverage. The participants were highly diverse, and the average participant age was 50.
Suggestions from the American Medical Association (AMA) on how health care providers can use their EHR for screening and identification of potential participants for the National DPP lifestyle change program can be found here.
Querying a Medical Claim or EHR
There are several billing and procedure codes that could be pulled from a medical claims database or EHR to identify potentially eligible individuals. For example, a query could be set up to pull information required for program eligibility. In instances where a specific lab value is required for inclusion, the actual lab value should be pulled. The program eligibility criteria for the National DPP lifestyle change program are listed below, with potential codes and other query-able elements listed in the columns to the right of each criteria. The presence of an x at the end of the code indicates there are multiple code modifiers or options for each of those codes.
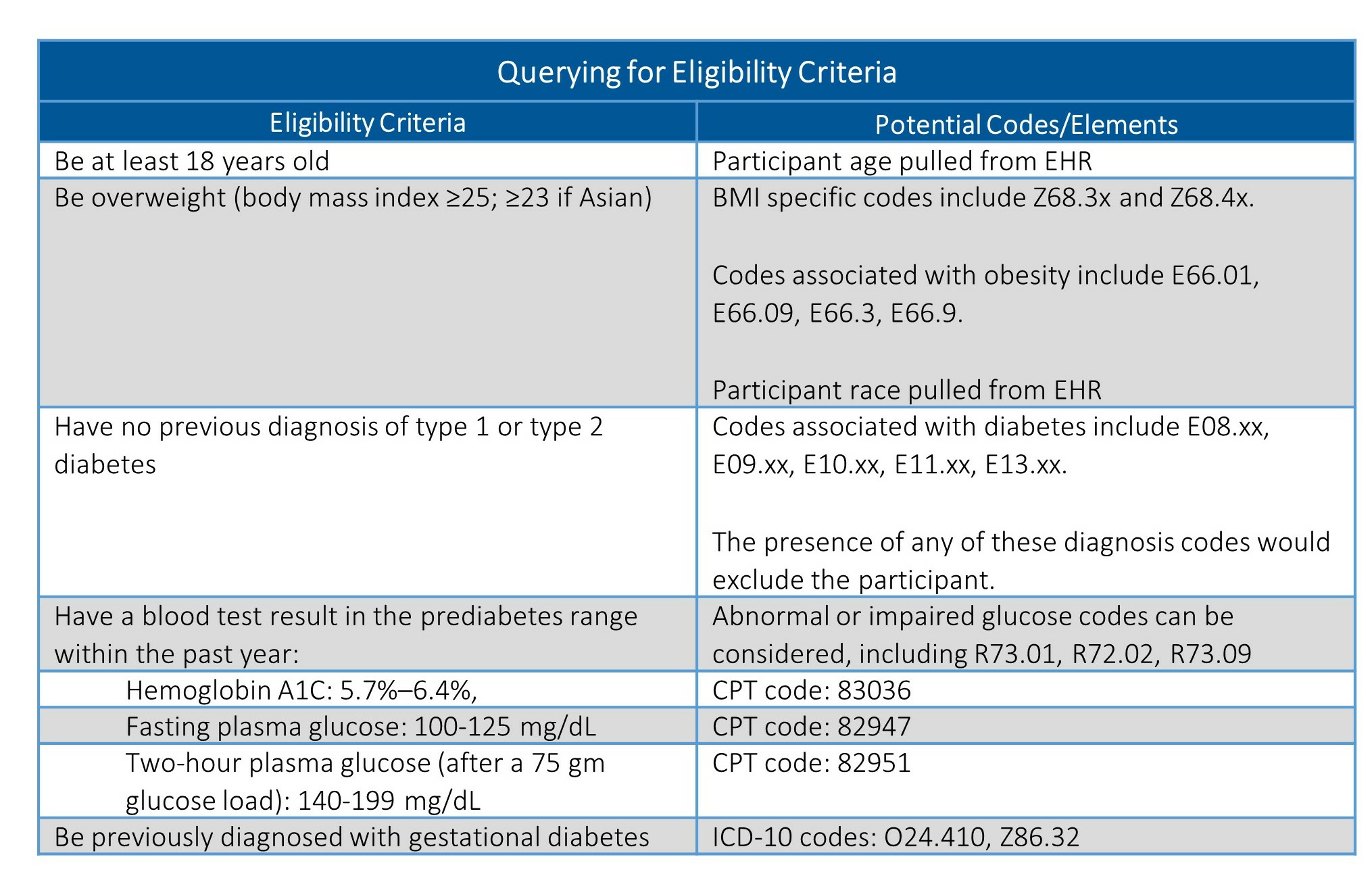
A description of many of these codes, as well as applicable office visit or procedure codes, can be found on the AMA’s list of codes to use when screening for prediabetes and diabetes. While the ICD-10 and CPT codes should be consistent across facilities, how databases are structured and queried is likely to vary. It is important to engage a database expert within your organization early in this process to understand how best to refine your query.
Risk Stratification
Once this data is collected, it could then be stratified to determine which individuals are at the highest risk of developing diabetes and could most benefit from this program. Below is an example risk stratification which could be used to assess potential participants and how broadly or narrow a plan may want to extend access to the program.

Tracking Progress Through Claims
A subject’s participation in the program can also be tracked by following the submission of claims as they are received. This provides information on whether or not the participants are both attending and meeting milestones in the program.
For more information on coding for the National DPP lifestyle change program in a claims system, see the Coding and Billing page of the Coverage Toolkit.
Identification by Providers
In other states and implementations, providers have been trained to assist in identifying individuals at risk for type 2 diabetes.
Minnesota
The Minnesota Department of Health, in concert with its partners, enacted the following identification strategies:
- Trained and supported clinic physicians and other providers to identify Medicaid patients at risk and refer them to the program
- Trained and supported clinic support staff such as laboratory personnel, medical assistants, and community health workers to identify potentially eligible participants
YMCA
The YMCA of the USA implemented the National DPP lifestyle change program with Medicare beneficiaries, through support from the Centers for Medicare and Medicaid Innovation’s Health Care Innovation Awards, and reported using the following identification strategies:
- Engaged health systems in mining medical records for candidates
- Looked within the YMCA membership for potential candidates
For more information see the YMCA of the USA DPP 2015 Annual Report. For additional data reports from this project, see CMS’ Health Care Innovation Awards page.
function goToLink() {
window.open(‘https://innovation.cms.gov/innovation-models/health-care-innovation-awards#:~:text=The%20Health%20Care%20Innovation%20Awards,those%20with%20the%20highest%20health” rel=”noopener” target=”_blank’);
}
Health Care Provider Videos – Prediabetes and the National DPP
These videos were developed to encourage health care teams to work together and with their patients to identify prediabetes and increase referrals to the National DPP lifestyle change program. These videos were created by NACDD in collaboration with the AMA and through support from the CDC, Division of Diabetes Translation.Team-Based Care: Clinical Care Management and the National DPP
This video, based in a hospital, highlights the responsibility of care management in implementing and sustaining effective diabetes prevention strategies by health care providers, including referrals to the National DPP lifestyle change program.
Timing: 3:18 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Team-Based Care: Clinical Care Team Roles and Responsibilities for Diabetes Prevention
This video, based in a clinical setting, explores the different roles health care team members can play in identifying patients with prediabetes and providing care and follow-up, including referrals to the National DPP lifestyle change program.
Timing: 4:05 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Clinical Care: Prediabetes Identification and Treatment
This video illustrates how health care providers can help their patients address prediabetes through referral to the National DPP lifestyle change program.
Timing: 4:18
Audience: Clinical Care team (physician, nurse practitioner, physician’s assistant, nurse, medical assistance, care manager, care coordinator, etc.)
Health Information Exchange Engagement
To reduce type 2 diabetes rates, Maryland Medicaid has worked closely with Chesapeake Regional Information System for our Patients (CRISP), the state designated health information exchange (HIE), to identify individuals eligible for participation in the National DPP lifestyle change program and facilitate referrals through a closed-loop electronic referral process.
CRISP uses various data sources to identify individuals with prediabetes who are likely eligible for the National DPP lifestyle change program. CRISP then generates a “Care Alert” for these individuals that communicates eligibility to their health care provider(s). CRISP also uses monthly “SmartAlerts” to alert MCO case management teams of potentially eligible individuals on their rosters. CRISP’s closed-loop (i.e., bi-directional) referral tool (eReferral) allows health care teams to refer eligible individuals to outside organizations offering the National DPP lifestyle change program, and to receive referral status and enrollment updates on the referred individuals.
To learn more about Maryland’s CRISP prediabetes flag and eReferral tool, please see the CRISP Prediabetes Flag and eReferral Overview document and please watch the June 9, 2022 NACDD General Member Webinar, Making an Impact on Population Health: Utilizing a State-wide Health Information Exchange to Promote the National Diabetes Prevention Program.