Medicaid → State Stories of Medicaid Coverage → Michigan
Michigan’s State Story of Medicaid Coverage
Overview
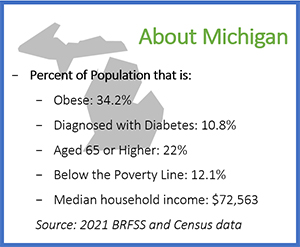
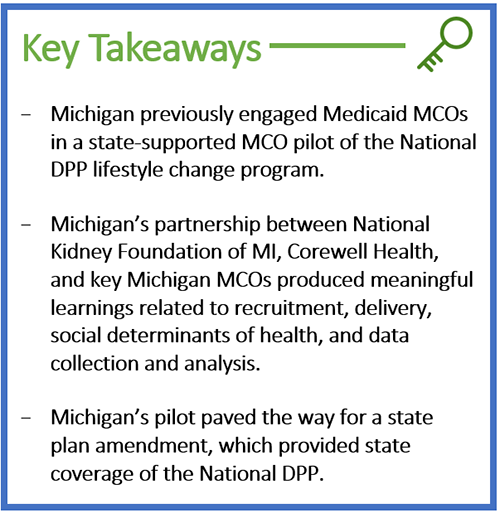
From 2020-2023, the Michigan Department of Health and Human Services (MDHHS) used CDC 1815 funds to partner with two CDC-recognized organizations, Corewell Health (formerly Beaumont Health) and National Kidney Foundation of Michigan (NKFM), to engage Medicaid MCOs through a state-supported pilot of the National DPP lifestyle change program. Michigan used this pilot to understand what was needed to sustainably offer the National DPP lifestyle change program to Medicaid beneficiaries throughout the state. Initially, the pilot launched with UnitedHealthcare Community Plan (UHCCP) working collaboratively with NKFM and Corewell Health to provide the National DPP lifestyle change program for their Medicaid members as part of the pilot. Additional MCOs joined the pilot after one year, including McLaren Health, Blue Cross Complete, and Priority Health. MDHHS offered technical assistance to organizations participating in the pilot to carry momentum and further efforts towards supporting the National DPP lifestyle change program as a statewide Medicaid benefit.
Following the efforts of the state-supported pilot, Michigan enacted coverage of the Michigan Diabetes Prevention Program (MiDPP) under a state plan amendment (SPA), along with a new Medicaid policy, effective July 2023. MiDPP is covered under the “Preventive Services” section and created a new provider type for reimbursement of delivery of the National DPP lifestyle change program by Lifestyle Coaches.
Establishing Coverage
Initial Steps Towards Medicaid Coverage
In 2015, the Diabetes and Other Chronic Diseases Section staff within the Michigan Department of Health and Human Services (MDHHS) began considering policy options to establish Medicaid coverage of the National DPP lifestyle change program in Michigan. However, due to the parallel timing of CMS authorizing the Medicare Diabetes Prevention Program (MDPP), Michigan Medicaid opted to wait to pursue state Medicaid coverage to determine if and how the Medicare benefit might impact the design of a Michigan Medicaid benefit.
State-Supported MCO Pilot of the National DPP Lifestyle Change Program
MDHHS decided to pursue an MCO pilot of the National DPP lifestyle change program in Medicaid, which used CDC’s 1815 funds. A state-supported MCO pilot would give MDHHS an opportunity to collect effectiveness data for the state Medicaid agency, and to test administrative processes and delivery of the National DPP lifestyle change program to Medicaid beneficiaries in Michigan. For general information on state-supported MCO pilots and examples in other states, see the Engaging MCOs to Attain Coverage page.
Recruiting MCOs to Participate in the Pilot
As a first step in MCO recruitment, the MDHHS staff attended a “Pay for Success” convening and a meeting with the Michigan Association of Health Plans (MAHP), where MDHHS, in collaboration with NKFM, pitched the idea of a National DPP lifestyle change program pilot to Medicaid MCOs. Prior to the MAHP meeting, MAHP assisted MDHHS in sending out a survey to the attending MCOs to assess the MCOs’ current efforts around diabetes prevention. The Michigan team considered the survey to be an important step for partner engagement as it allowed them to structure their pilot proposal to complement the work of the MCOs.
The MCO pilot was framed as “free to the MCO” and as an opportunity for MCOs to work with experienced CDC-recognized organizations and receive technical assistance from the state. It was also presented as an opportunity to set up the necessary processes that may be required of MCOs if the program became a statewide Medicaid benefit.
Selecting MCOs
United Healthcare Community Plan (UHCCP) was one of the first MCOs to show interest in piloting the National DPP lifestyle change program to beneficiaries. UHCCP took steps to examine prediabetes data for their membership to determine the current need and potential geographic areas of focus. MDHHS began having conversations with UHCCP to identify a potential CDC-recognized organization to work with.
In addition to UHCCP and the above MAHP meeting, NKFM and MDHHS conducted a readiness assessment with the additional interested MCOs to determine capacity and needs to build a successful pilot. The readiness assessment questions included:
- Have you pulled prediabetes incidence data?
- Do you have staff available?
- Do you have capacity to do outreach?
- Can you offer a data sharing agreement?
MDHHS was encouraged to find that quite a few plans were interested in the pilot. Several factors made these plans a good fit for Michigan’s pilot, including:
- These plans were already pulling data on prediabetes rates for their members or had the ability to easily begin.
- The plans were able to propose a focus on a higher-risk geographic area using this data.
- The plans had staff capacity to assist in identifying and engaging members in the National DPP lifestyle change program.
Conducting the State-Supported MCO Pilot
MDHHS conducted the state-supported MCO pilot of the National DPP lifestyle change program with UHCCP and Corewell (formerly Beaumont) Health from 2020-2023.
MDHHS also partnered with the National Kidney Foundation of Michigan (NKFM) as an additional CDC-recognized organization to deliver the National DPP lifestyle change program to UHCCP members and to engage additional Medicaid MCOs to provide the National DPP lifestyle change program for their members as part of the pilot.
MCOs identified eligible participants, using indicators such as prediabetes diagnosis code, age, and history of gestational diabetes, and then sent initial outreach to members using letters and/or emails. Business associate agreements (BAAs) were formed between the CDC-recognized organization and the MCO to allow sharing of information on eligible members (see the Contracting with CDC-Recognized Organizations page to learn more about contracting between MCOs and CDC-recognized organizations). In some cases, the CDC-recognized organization followed up directly with eligible members after initial contact by the MCO.
Technical Assistance for Pilot Participants
The structure of Michigan’s state-supported MCO pilot was unique because it focused on providing technical assistance to CDC-recognized organizations while also collecting data to support development of a statewide Medicaid benefit. As part of the 1815 requirement, each CDC-recognized organization funded through the pilot was required to submit data on per-participant costs to provide the program. MDHHS also collected evaluation data to assess whether participating organizations were meeting their standards, which include targets for enrollment, attendance, and weight loss. MDHHS modeled these requirements after the current CDC recognition standards.
MDHHS set up a timeline for evaluation that prompted them to give technical assistance to CDC-recognized organizations that were not meeting standards. If CDC-recognized organizations were not reaching standards halfway through the contract year, MDHHS worked with them to create a performance improvement plan. If at the end of the year the CDC-recognized organization had still not achieved the standards, pilot reimbursement was be decreased incrementally. From the health department perspective, this process created a realistic model for pay-for-performance that built capacity for CDC-recognized organizations.
To learn more about evaluation methods and examples of other states that have evaluated the National DPP lifestyle change program, please see the evaluation section of the Data, Reporting, and Evaluation page of the Coverage Toolkit.
Establishing State Medicaid Coverage of the National DPP Lifestyle Change Program
Michigan used data from the pilot to demonstrate why statewide Medicaid coverage of National DPP lifestyle change program should be prioritized by Michigan Medicaid, including cost learnings from the pilot and cost projections for state-wide coverage. Provider, MCO, and internal MDHHS champions helped to showcase the work accomplished during the pilot.
Michigan Medicaid determined to cover the program in fee-for-service Medicaid and to require MCOs to provide the benefit as well. Michigan finalized a SPA, effective as of July 1, 2023, to secure federal Medicaid matching funds for the National DPP lifestyle change program. The SPA creates a new provider type to allow CDC-recognized organizations to be reimbursed by Medicaid.
Implementing Coverage
Benefit Breakdown
Below is an overview of Michigan’s Medicaid benefit which can be found in the Michigan Medicaid Policy MiDPP Bulletin.
| Delivery Methods | The National DPP lifestyle change program may be delivered to Medicaid beneficiaries in person, through distance learning (synchronous audio-visual or audio-only telemedicine), or online. |
| Participant Eligibility |
To be eligible for the National DPP lifestyle change program, Medicaid beneficiaries must be:
A beneficiary whose prediabetes diagnosis changes to diabetes during a MiDPP session may continue a series upon recommendation of their healthcare provider and a referral to DSME initiated. A beneficiary may repeat MiDPP as long as they meet the eligibility guidelines identified above. Beneficiaries must also have a referral to the MiDPP by a licensed healthcare provider, such as a:
|
| Lifestyle Coaches | According to the Policy Bulletin, “A MiDPP provider is the organizational and billing entity, and the MiDPP Lifestyle Coach is the session leader and rendering provider. Each must meet CDC recognition standards, including educational and experience requirements, as well as meet MDHHS provider enrollment requirements. It is the responsibility of the enrolled MiDPP provider to ensure the Lifestyle Coaches affiliated with their programs meet CDC program requirements and are enrolled in Medicaid.” |
| Eligible Providers |
An organization must have preliminary, or full CDC recognition from the Diabetes Prevention Recognition Program (DPRP) to provide the National DPP lifestyle change program to Medicaid beneficiaries. The Diabetes & Kidney Unit (DKU) within the MDHHS Public Health Administration (PHA) will monitor MiDPP providers and Lifestyle Coaches for compliance to CDC recognition requirements. Once the MiDPP provider is approved by the DKU, provider enrollment may be initiated in the Michigan Medicaid Community Health Automated Medicaid Processing System (CHAMPS). An enrolling provider must have a Type 2 (Organization) National Provider Identification (NPI) number and the Lifestyle Coach must have a Type 1 (Individual) NPI number before enrolling in CHAMPS. |
| Reimbursement, Coding, and Billing |
MiDPP claims are submitted by the MiDPP provider with the approved MiDPP Healthcare Common Procedure Coding System (HCPCS) diagnosis code of Z71.89: Other Specified Counseling. Additional codes identify weight loss and beneficiary session attendance either as a Core Session in months 1- 6 or a Core Maintenance Session in months 7-12. Michigan’s fee schedule can be accessed here:
Total possible reimbursement per participant: $768 (not including Bridge payment) Federally Qualified Health Center (FQHC), Rural Health Clinic (RHC), Tribal Health Center (THC), and Tribal FQHC Reimbursement for MiDPP services are reimbursed at the Medicaid Fee Screen reimbursement rate and are not eligible for the Prospective Payment System (PPS) or the All-Inclusive Rate (AIR). For more information on FQHC billing, visit the Engaging Federally Qualified Health Centers page of the Coverage Toolkit. Of note, additional changes to the reimbursement schedule to align with MDPP are planned for July 1, 2024. |
Lessons Learned
Best Practices for Engaging MCOs During the MCO Pilot
MDHHS notes several best practices for MCO engagement that contributed to their successful engagement during the MCO pilot, including:
- Leverage existing relationships between MCOs and CDC-recognized organizations.
- Consider CDC-recognized organizations that are in-network with MCOs and if any MCOs have existing data sharing agreements with CDC-recognized organizations.
- Before approaching MCOs about a pilot, consider surveying potential partners about current efforts around prediabetes to understand what each MCO is already doing.
- Consider the audience to approach first within the MCO. Michigan decided to contact the Chief Medical Officers at the MCOs to get leadership buy-in.
- Engage influential community-based partners in the process when approaching MCOs.
- Present to MCOs the national perspective of diabetes and the National DPP alongside the pitch for a pilot. This helps MCOs see where the program can fit within a national perspective and can inspire some competition between states and other health plans.
- To see a list of payers currently covering the National DPP lifestyle change program, visit the Participating Payers and Employers page.
- For materials on making the case for coverage of the National DPP lifestyle change program, visit the Case for Coverage for Medicaid page.
- MCOs participating in a pilot can provide key insights into how the National DPP lifestyle change program can be operationalized in Medicaid, including input on participant identification, enrollment, and retention; promotion of the benefit; and billing and reimbursement processes.
Reflections on Implementing Medicaid Coverage of the MiDPP
In addition to the learnings obtained during the MCO pilot, Michigan noted the following reflections from implementation of the MiDPP benefit in Medicaid.
- Identify champions to assist with educating partners on National DPP efforts. For example, provider, MCO, and internal MDHHS champions helped to showcase the work accomplished during the pilot and emphasize the need for state Medicaid coverage of the National DPP lifestyle change program.
- Emphasize the need to prioritize diabetes prevention efforts. In Michigan, the state Medicaid agency typically engages in 2-3 policy changes per year. To achieve Medicaid coverage of the National DPP lifestyle change program, Michigan partners had to acknowledge competing public health priorities and demonstrate why diabetes prevention should be included among existing efforts. Michigan’s ability to use data from the pilot helped in making the case for prioritizing coverage of the National DPP lifestyle change program.
- Demonstrate cost benefits of the National DPP lifestyle change program. Michigan was able to share cost learnings obtained during pilot work as well as cost projections for state coverage of the National DPP lifestyle change program.
- Showcase the public health role to support Medicaid. Michigan was able to leverage their public health commitment to and expertise in the National DPP by developing internal procedures that outline how public health would support operationalizing the MiDPP benefit.
Additional information on cost analysis for the National DPP lifestyle change program is available on the Cost and Value page of the Coverage Toolkit.









