Medicaid → State Stories of Medicaid Coverage → Illinois
Illinois State Story of Medicaid Coverage
Overview
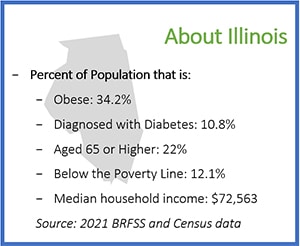
Illinois’ efforts surrounding Medicaid coverage for the National Diabetes Prevention Program (National DPP) lifestyle change program began in 2014, shortly after the Centers for Medicare and Medicaid Services (CMS) issued the rule change that allows Medicaid services to be provided by non-licensed staff and paved the way for Medicaid reimbursement to CDC-recognized organizations. Illinois began their journey by convening partners including the Illinois Department of Public Health (IDPH), Illinois Public Health Institute (IPHI), Illinois Department of Healthcare and Family Services (HFS), and Illinois managed care organizations (MCOs) to begin conversations around the creation of a new benefit. These conversations continued through 2017 with various sources of grant funding. Illinois then participated in CDC’s 6|18 Initiative from late 2019 through 2021, which provided the state direct technical assistance from CDC and NACDD, and opportunities for group-based learning around Medicaid coverage of the National DPP lifestyle change program.
Illinois’ path to coverage for the National DPP lifestyle change program involved launching a unique MCO mock claims pilot with the objective of identifying effective recruitment strategies and testing claims and data sharing processes. This pilot began in October 2020 and continued through October 2021.
With support from NACDD and CDC, IDPH, IPHI and HFS worked with stakeholders and consultants to develop recommendations for submitting a state plan amendment (SPA) to secure Federal Financial Participation (FFP) (federal Medicaid matching funds) for the National DPP lifestyle change program, as well as a plan to operationalize the benefit. Illinois’ SPA can be accessed here. Medicaid coverage for the National DPP lifestyle change program in Illinois became effective on August 1, 2021.
Establishing Coverage
The road to Medicaid coverage for the National DPP lifestyle change program in Illinois involved many different partners and combined efforts. This included an MCO pilot, as well as a SPA.
- 2014: IPHI received a $5,000 grant from County Rankings and Roadmaps to begin discussion around Medicaid coverage for the National DPP lifestyle change program. Initial convenings with IDPH, IPHI, HFS, MCOs, and CDC-recognized organizations initiated a roadmap to coverage for the state.
- 2016: IDPH participated in IPHI-led convenings and workgroup meetings with HFS and MCOs that led to the development of resources that furthered state Medicaid coverage initiatives, including a roadmap to Medicaid coverage for chronic disease prevention and management programs.
- 2018: Illinois was awarded cooperative agreement funding from CDC to work towards coverage for the National DPP lifestyle change program. IDPH received funding from a CDC 1815 grant and the Chicago Department of Public Health, with IPHI as its bona fide agent, received funding from a CDC 1817 grant. Later that year, IDPH and HFS collaboratively applied for the 6|18 Initiative led by CDC and NACDD.
- 2019: In December 2019, IDPH, in collaboration with IPHI and HFS, began participating in the 6|18 Initiative to develop strategies and incorporate best practices for Medicaid coverage for the National DPP lifestyle change program. Throughout the 6|18 Initiative, Illinois received individual and group-based technical assistance from CDC and NACDD and learned from other states’ experiences. Involvement in this initiative led to development of recommendations to submit a SPA to CMS to secure federal Medicaid matching funds for the National DPP lifestyle change program, as well as an operational plan for rolling out and sustaining the benefit. To learn more about SPAs, visit the Attaining Coverage Through a Medicaid State Plan page of the Coverage Toolkit.
- 2020: Illinois launched a unique MCO mock claims pilot in October 2020, which was funded by Meridian Health Plan of Illinois (“Meridian”) (an MCO) in partnership with IPHI. The CDC-recognized organizations that participated in the MCO pilot were Federally Qualified Health Centers (FQHCs) in the state. The four participating FQHCs received funding from Meridian to participate in the pilot, in addition to funding from IPHI to run the classes. The pilot identified effective recruitment strategies and implemented claims and data sharing processes. This process revealed opportunities for growth in systems related to data sharing, referrals, engagement, and Medicaid eligibility. To learn more about the role MCOs can play in promoting Medicaid coverage for the National DPP lifestyle change program, visit the Engaging MCOs to Attain Coverage page of the Coverage Toolkit.
- 2021: Illinois Medicaid coverage for the National DPP lifestyle change program went into effect on August 1, 2021. A public notice of coverage for the National DPP lifestyle change program and Diabetes Self-Management Education and Support (DSMES) services was published on August 2, 2021, and the provider notice was issued on August 21. Illinois was awarded a one-year funding and technical assistance opportunity from NACDD for the Medicaid Beneficiary Enrollment Project (MBEP) to support enrollment in the National DPP lifestyle change program. Illinois then awarded ten CDC-recognized organizations with $10,000 each to focus on building their infrastructure and workflows for the program. This was supported by CDC funds received from the NACDD MBEP and CDC 1817 grants.
- 2022: Illinois’ SPA was approved by CMS on February 4, 2022 and can be viewed here. A second provider notice of coverage was published on July 29, 2022 describing billing updates for the National DPP lifestyle change program and DSMES services in Illinois.
Implementing Coverage
Below is an overview of the Illinois Medicaid benefit:
Benefit Breakdown
| Delivery Methods | The National DPP lifestyle change program may be delivered to Medicaid beneficiaries in-person, online, or through distance learning. Services rendered via a real-time interactive audio-only telecommunications system are also covered. |
| Lifestyle Coaches | “Providers of these services include physicians, nonphysician licensed practitioners and unlicensed practitioners under the supervision of a [National] DPP service provider or licensed practitioner. For [National] DPP services delivered by unlicensed Lifestyle Coaches, the supervising practitioner will assume professional liability for the care of the patient and furnish services with its scope of practice according to state law.” (Illinois Medicaid SPA) |
| Medicaid Enrolled Provider Eligibility | Only organizations that have achieved CDC recognition can be enrolled in Medicaid to bill for providing the National DPP lifestyle change program to Medicaid beneficiaries. |
| Accepted CDC Recognition Levels | Illinois Medicaid recognizes all three CDC-recognition levels (pending, preliminary, and full) and will enroll any organization or individual that has achieved any of these recognition levels as a Medicaid CDC-recognized organization. |
| Provider Enrollment | CDC-recognized organizations can enroll with Medicaid through the Illinois Medicaid Program Advanced Cloud Technology (IMPACT) system. This Medicaid management information system supports provider enrollment and claims processes for Medicaid. Any FQHC, rural health clinic, or encounter rate clinic, even if already enrolled in IMPACT, must create a separate enrollment, and obtain a separate national provider identifier (NPI) to bill for diabetes prevention services. Medicaid enrolled CDC-recognized organizations are eligible to receive reimbursement for National DPP services rendered to Medicaid beneficiaries. |
| Program Duration | The Illinois Medicaid National DPP lifestyle change program follows the established CDC evidence-based program approach of a 12-month program. |
| Program Repeatability | Illinois Medicaid does not limit participation in program services to once per lifetime. |
| Medicaid Data Submission Requirements | Illinois Medicaid requires CDC-recognized organizations to provide their DPRP code when applying to become a Medicaid-enrolled provider and reaffirm their code every year. Beyond their recognition status, organizations are not required to submit participant data to Medicaid. |
| Participant Referral Requirements | Health care providers and MCOs can recommend Medicaid beneficiaries to the program, however, a formal referral is not required to participate. Eligible participants can directly enroll with a CDC-recognized organization by supplying blood test results from within the past year indicating a diagnosis of prediabetes or gestational diabetes mellitus. |
| Reimbursement, Coding, and Billing |
The Illinois Medicaid rates for reimbursement for the National DPP lifestyle change program are session and performance-based for both in-person and online programs. Maximum Medicaid reimbursement for the National DPP lifestyle change program in Illinois is $670 per member. The reimbursement is broken down as follows:
|
Program Features Unique to Illinois
MCO Mock Claims Pilot
Illinois’ MCO mock claims pilot ran from October 2020 to October 2021 and was funded by Meridian in partnership with IPHI. The objectives of this pilot were to identify effective recruitment strategies and test claims and data sharing processes. The goal was to learn how stakeholders work together to provide the National DPP lifestyle change program and to use a mock claims process to prepare organizations for achieving Medicaid coverage of the National DPP lifestyle change program. No actual money was exchanged as part of the process. This unique pilot helped to shape and test the recommended National DPP lifestyle change program Medicaid benefit design.
Online Resource: Chicago CARES to Prevent Diabetes
The Chicago Department of Public Health, in partnership with IPHI, created a website called Chicago CARES to Prevent Diabetes to support their diabetes prevention initiative. The website, which is available in both English and Spanish, presents educational health information, including factors that increase risk for developing prediabetes and type 2 diabetes. In addition to details on the National DPP lifestyle change program, the site displays written testimonials from participants and information on existing programs in the Chicago area. The site also includes information for CDC-recognized organizations, including training videos, customizable tools, and frequently asked questions surrounding Medicaid coverage and enrollment. Funding for this website came from a CDC 1817 grant.
Lessons Learned
- The ongoing engagement of partners and the committed effort through various policy and state agency staff changes is essential to achieving Medicaid coverage for the National DPP lifestyle change program.
- The close partnership between Illinois’ governmental agencies and the non-governmental public health advocacy organization, IPHI, increased buy-in among decision makers across public and private sectors.
- The MCO pilot demonstrated the importance of facilitating communication between staff from MCOs and CDC-recognized organizations, especially as related to billing and claims processes. Building workflows among all partners allows for appropriate engagement with participating members and care coordinators. Engaging all relevant MCO staff early in the evaluation process can facilitate more effective testing of each piece of the pilot.
- Recruitment typically requires the identification of many eligible members to end up with a sufficient number of enrollees for each cohort. Broad outreach and establishing a referral program are beneficial to implementation of the National DPP lifestyle change program.









