Medicaid → State Stories of Medicaid Coverage → Minnesota
Minnesota’s State Story of Medicaid Coverage
Overview
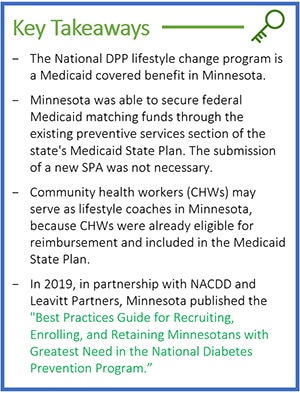
On January 1, 2016, the Minnesota Department of Human Services (referred to throughout this article as DHS or Minnesota Medicaid) began offering the National Diabetes Prevention Program (National DPP) lifestyle change program as a covered benefit for Medicaid beneficiaries through the preventive services section under their existing Medicaid State Plan authority. The state was able to claim federal Medicaid matching funds for the program through Minnesota’s Medicaid State Plan without the submission of a new State Plan Amendment (SPA), because the Medicaid State Plan already included language defining preventive services that was broad enough to encompass the National DPP lifestyle change program and covered services provided by community health workers (CHWs). This approach differs from how other states have claimed federal Medicaid matching funds for covering the National DPP lifestyle change program. For example, Maryland uses an 1115 demonstration waiver, and California and New York had to submit new SPAs. For more information on when a SPA is needed, visit the Attaining Coverage Through a Medicaid State Plan page of the Coverage Toolkit.
Establishing Coverage
The road to Medicaid coverage for the National DPP lifestyle change program involved many different stakeholders and efforts.
Minnesota Diabetes Plan: Early Efforts to Prevent Diabetes
In 2005, the Minnesota Diabetes Program (MDP), with support from the Minnesota Diabetes Steering Committee (MDSC) and funding from the CDC, published the Minnesota Diabetes Plan 2010 Year 1 Progress Report as part of the MDP’s strategic plan to reduce the burden of diabetes in Minnesota. The report cited the costs of diabetes and identified prevention as one of eight key diabetes focus issues for the state.
Medicaid Incentives for Prevention of Chronic Disease: Federal Funding to Support Diabetes Prevention
From 2010 to 2015, DHS and the Minnesota Department of Health (MDH) jointly received a federal grant through the Medicaid Incentives for Prevention of Chronic Disease (MIPCD) program, created by Section 4108 of the Patient Protection and Affordable Care Act (ACA) for states to develop evidence-based prevention programs that provide incentives to Medicaid beneficiaries to participate in and complete programs like the MIPCD. Ten states (California, Connecticut, Hawaii, Minnesota, Montana, Nevada, New Hampshire, New York, Texas, and Wisconsin) were awarded demonstration grants to implement chronic disease prevention approaches for their Medicaid beneficiaries to test the use of incentives to encourage behavior change. Four of the ten states—Minnesota, Montana, Nevada, and New York—used grant dollars to fund incentives specifically for the National DPP lifestyle change program. Minnesota’s program was called “We Can Prevent Diabetes.” Participation in the MIPCD program helped put Minnesota on a path towards Medicaid coverage for the National DPP lifestyle change program. In 2017, DHS, MDH and the HealthPartners Institute published results of the We Can Prevent Diabetes program in a study titled “Financial incentives for diabetes prevention in Medicaid population” in the journal Contemporary Clinical Trials.1 The study examined how financial incentives affect Medicaid beneficiaries’ weight loss and attendance in the National DPP lifestyle change program. The trial demonstrated that a collaborative approach with primary care clinics and CDC-recognized organizations could efficiently identify, enroll, and deliver the 12-month program to Medicaid beneficiaries. Moreover, the trial found that the use of financial incentives may be an avenue for engaging low-income, high-risk patients in lifestyle change. That same year, RTI International published results from all ten states that participated in the MIPCD program. The report discussed key findings from Minnesota’s “We Can Prevent Diabetes” program, including:
- Incentives led to modest but significant increases in the percentage of participants achieving 5% weight loss but had insignificant effects on average weight loss.
- To address accessibility challenges, Minnesota provided participants transportation to their classes either through a shuttle or taxi service or reimbursed participants for public transportation costs.
- High staff turnover negatively impacted enrollment into the program.
- The Lifestyle Coach was a significant reason why participants remained in the program. Lifestyle Coaches from the same population group as targeted participants helped encourage enrollment and retention.
- Incentives to providers enhanced referrals.
Collective Impact Initiative: Cross-Stakeholder Collaboration to Implement Diabetes Prevention
In 2010, the same year MDH and DHS received the MICPD grant, MDH secured an NACDD grant and hired a contractor to initiate a collective impact approach to tackle the diabetes epidemic in Minnesota by aligning efforts, sharing data, and engaging the community. The Minnesota Diabetes Collective Impact Initiative involved about 30 organizations, including Minnesota health insurers and delivery systems, state health care quality improvement and measurement organizations, pharmaceutical organizations, the University of Minnesota, and disability, community, social service, employee union, and employer advocacy organizations. The Minnesota Diabetes Collective Impact Initiative established a mission to become the state with the lowest incidence of and healthiest outcomes for diabetes in the nation. Over time, the mission of the Collective Impact coalition evolved to focus most strongly on diabetes prevention and scaling up the National DPP statewide by encouraging Minnesota payers and employers to move towards health plan coverage and reimbursement for the National DPP lifestyle change program. As a result, efforts were initiated to have Minnesota’s State Employee Group Insurance Program (SEGIP) and Minnesota Medicaid cover the program. In April 2015, SEGIP began offering the program to all state employees and their insured adult dependents, through the online National DPP lifestyle change program provider Omada.
Medicaid Coverage: Achieving Coverage through the State Plan
In 2016, DHS implemented coverage for the National DPP lifestyle change program in Medicaid for their managed care and fee-for-service (FFS) populations as a result of the preventive services section in their Medicaid State Plan and their interpretation of Medicaid’s requirement to cover the United States Preventive Services Task Force (USPSTF) grade A and B recommendations. For more information on the USPSTF recommendations, see the Attaining Coverage Through a Medicaid State Plan page of the Coverage Toolkit.
Implementing Coverage
Benefit Breakdown
Below is an overview of Minnesota’s Medicaid benefit which can be found in the Minnesota Health Care Programs (MHCP) Provider Manual.
| Delivery Methods | The National DPP lifestyle change program may only be delivered to Medicaid beneficiaries in person. |
| Participant Eligibility | To be eligible for the National DPP lifestyle change program, Medicaid beneficiaries must have a diagnosis of prediabetes by a qualified physician, i.e., a person who is licensed to provide health services within the scope of his or her profession under Minnesota Statutes, 147. For purposes of this section, a physician means a licensed Doctor of Medicine or Osteopathy. |
| Lifestyle Coaches | A Lifestyle Coach may be a licensed health professional, a CHW, or an unlicensed individual trained in the CDC curriculum. Minnesota CHWs are trained health educators who have received a valid certificate by completing a statewide 14-credit CHW curriculum at one of seven schools that offer the certificate program. |
| Eligible Providers | An organization must have pending, preliminary*, or full CDC recognition from the Diabetes Prevention Recognition Program (DPRP) to provide the National DPP lifestyle change program to Medicaid beneficiaries.
*Preliminary CDC recognition status language is currently missing from the MHCP Provider Manual, but it may be updated in the future to include it. |
| Reimbursement, Coding, and Billing | CDC-recognized organizations use the National DPP CPT code 0403T for billing. Providers are reimbursed $13.62 per hour per beneficiary under Medicaid FFS (approximately $300 for 22 sessions). Medicaid managed care organizations (MCOs) negotiate payment rates with their network providers. |
Program Features Unique to Minnesota
Trellis Umbrella Hub Arrangement
While Minnesota was an early adopter of Medicaid coverage for the National DPP lifestyle change program, there were challenges with the uptake of the benefit in the state. Community-based organizations (CBOs) faced barriers to delivering the National DPP lifestyle change program, including low enrollments impacting the ability to maintain CDC recognition status, low reimbursement rates, and high administrative burden and costs to recruit and enroll participants. CBOs also faced challenges contracting with MCOs that did not have the capacity to contract with multiple individual delivery organizations. As a result, MDH began exploring pathways to assist these CBOs. With support from CDC and NACDD, MDH funded the operationalization of an umbrella hub arrangement (UHA).
UHAs are led by an umbrella hub organization (UHO); an organization capable of successfully providing technical assistance, administrative support, and guidance to CBOs. MDH partnered with Trellis, an Area Agency on Aging (AAA) and non-profit, to serve as the UHO. Trellis’ business acumen and willingness to create new products, services, and relationships to meet the changing needs of Minnesotans living with prediabetes, made Trellis a prime candidate to serve as a UHO. MDH has supported Trellis and Minnesota CBOs over the last several years in operationalizing the UHA. As a result, Trellis has successfully enrolled as a Medicare Diabetes Prevention Program (MDPP) supplier, a Minnesota Medicaid enrolled provider, and contracted with various Medicaid MCOs and Medicare Advantage (MA) plans for reimbursement for the National DPP lifestyle change program for each of their participating CBOs (also known as subsidiary organizations). Trellis is now exploring pathways to incorporate additional services to expand its existing community care hub (CCH). For more information on Trellis’ UHA story, see the Trellis Spotlight below and on the UHA Spotlights page of the Coverage Toolkit.
Community Health Workers as Lifestyle Coaches
In Minnesota, CHWs may serve as Lifestyle Coaches. Because Minnesota’s Medicaid State Plan already recognized CHWs as eligible to provide a variety of preventive services, the state could use CHWs to administer the National DPP lifestyle change program without seeking a new SPA to claim federal Medicaid matching funds. See the Attaining Coverage Through a Medicaid State Plan page for additional details.
Minnesota Medicaid requires the following of CHWs to deliver the National DPP lifestyle change program:
- CHWs must work under the supervision of a physician, dentist, advanced practice registered nurse (APRN), certified public health nurse (PHN), mental health professional, or registered nurse to provide patient education for health promotion and disease management services.
- CHWs cannot bill Medicaid directly (i.e., they are the rendering provider).
- CHWs must have a valid certificate from the Minnesota State Colleges and Universities (MnSCU), demonstrating that the applicant has completed an approved community health worker curriculum.
- CHWs must be affiliated with a CDC-recognized organization and trained as a Lifestyle Coach.
CHW services are diagnosis-related medical interventions, not social services. Medicaid coverage includes diagnosis-related patient education services, including diabetes prevention and pediatric obesity treatment under specified criteria, including:
- The service involves teaching the patient how to self-manage their health effectively in conjunction with the health care team; and
- The service is provided face-to-face with the recipient (individually or in a group) in an outpatient, home, clinic, or other community setting.
To learn more about CHWs in Minnesota Medicaid please see the CHW section of the MHCP Provider Manual and the Minnesota CHW Toolkit.
Minnesota Best Practices Guide
In 2019, in partnership with NACDD and Leavitt Partners, MDH published the “Best Practices Guide for Recruiting, Enrolling, and Retaining Minnesotans with Greatest Need in the National Diabetes Prevention Program.” While the National DPP lifestyle change program is a covered benefit in Medicaid, CDC-recognized organizations have struggled to recruit and retain Medicaid beneficiaries in the program. The guide compiles evidence-based recommendations and real-life strategies that Lifestyle Coaches use to encourage enrollment in the program and support its successful completion. Some of the topics included in the guide are outreaching to priority populations, partnering with community organizations, establishing referrals with health care systems, demonstrating cultural competency, addressing literacy and language barriers, and using incentives.
In conjunction with the guide, the Minnesota Department of Health released the following videos interviewing Lifestyle Coaches and program coordinators to emphasize the retention strategies detailed in the Best Practices Guide:
- MN National Diabetes Prevention Program Best Practices Guide – Hennepin Health
- MN National Diabetes Prevention Program Best Practices Guide – Recruiting Participants
- MN National Diabetes Prevention Program Best Practices Guide – Keeping Participants Engaged
- MN National Diabetes Prevention Program Best Practices Guide – Lifestyle Coaches
- National Diabetes Prevention Program – Join a Program in Minnesota
Lessons Learned
Defining Clear Steps for Medicaid Reimbursement that Supports Both Health System and Community-Based CDC-Recognized Organizations
When seeking Medicaid reimbursement, there is value to being strategic, conducting pilots, and taking time for learning and relationship building. As part of the planning for implementation of state Medicaid coverage for the National DPP lifestyle change program, it is helpful for Medicaid to work with public health to clearly define the process for provider reimbursement. A clear pathway may include outlining which provider types to use (new or existing provider types) to offer the program, the codes required for Medicaid member diagnosis and referral to the program, and the steps required to submit medical claims for National DPP lifestyle change program services. Minnesota learned that it is important to assure that systems are clearly designed, and that they support both community-based as well as health care delivery CDC-recognized organizations to enroll as Medicaid providers and submit claims. CBOs are often trusted and can reach populations at greatest risk for type 2 diabetes in their local communities.
Next Steps
Because Minnesota Medicaid already covers the National DPP lifestyle change program, the state’s next steps are to increase utilization of the program. One of the state’s strategies is to focus on recruiting trusted and culturally competent CBOs to enroll as Medicaid providers of the National DPP lifestyle change program benefit. Policy changes that Minnesota would like to explore include pursuing a more sustainable Medicaid reimbursement rate, and expanding Medicaid coverage to include online and distance learning program delivery options.
Additional Resources
Best Practices Guide for Recruiting, Enrolling, and Retaining Minnesotans with Greatest Need in the National Diabetes Prevention Program
MHCP Provider Manual which includes the Minnesota Medicaid National DPP Lifestyle Change Benefit
Minnesota CHW Toolkit
Minnesota Medicaid CHW Benefit, Provider Manual
References
1Financial incentives for diabetes prevention in a Medicaid population: Study design and baseline characteristics. Contemp Clin Trials. 2017 Feb;53:1-10. doi: 10.1016/j.cct.2016.11.007. Epub 2016 Nov 23.