Recruitment & Referral
Recruitment and referral efforts are critical to the sustainability of the National Diabetes Prevention Program (National DPP) lifestyle change program. Various strategies and resources can be utilized to improve recruitment of program participants and increase the number of referrals to the program. Organizations are also encouraged to implement processes to better understand participant readiness and promote retention in the National DPP lifestyle change program. More information on retention strategies is available on the Retention page of the Coverage Toolkit.
This page provides guidance and resources for incorporating or improving recruitment and referral strategies, as well as understanding how to communicate with participants based on their readiness to change. The page is divided into the following sections:
- Recruitment
- Recruitment Resources
- Recruitment Strategies in Practice
- Referrals
- Bi-Directional Referrals Between Health Care Providers and CDC-Recognized Organizations
- Referral Strategies in Practice
- Participant Readiness
Recruitment
Entities promoting the National DPP lifestyle change program will need to consider appropriate and effective recruiting strategies to maximize participation in the program. Recruitment for the National DPP lifestyle change program may occur at many levels, from direct outreach to potential participants to indirect outreach to health care providers and provider associations (see the figure below). Outreach efforts may be broad enough to reach an entire population or be geared toward specific groups.
Some recruiting strategies may prove to be more time- and cost-effective than others. For example, efforts to engage a health care provider to recommend the program to patients who are eligible for the National DPP lifestyle change program may be more cost-effective than sending direct mailings to potentially eligible members.
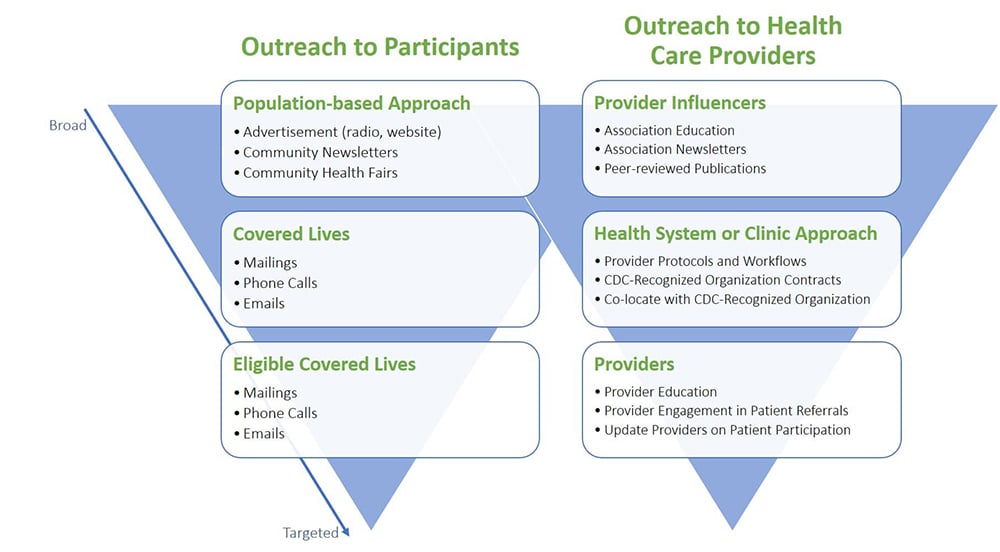
Multiple combinations of the following strategies have been used to encourage participation in the National DPP lifestyle change program:
- Direct mailings
- Phone calls
- Follow-up contact with interested individuals
- Brochures in clinics or community centers
- Advertisement through local media outlets (posters, radio, community newsletters)
- Community health fairs and wellness events, sometimes held in partnership with local clinics
- Health care provider referrals
- Peer reviewed studies
Recruitment Resources
CDC’s Division of Diabetes Translation has developed a number of resources to support recruitment of National DPP lifestyle change program participants. These include:
- A tip sheet that provides lessons learned and insights on recruiting participants into the program. The tip sheet can be accessed here.
- The Path 2 Prevention (P2P) resource, which is intended to bridge the gap between the CDC’s Prediabetes Risk Test and enrollment in the National DPP lifestyle change program. See the infographic for more information.
- A Virtual Recruitment Toolkit. Virtual recruitment has become increasingly important as a result of the COVID-19 pandemic and as digital technology and the internet have become universal tools to communicate with people. The toolkit offers guidance on how to recruit program participants in a virtual or remote environment.
- The Recruitment and Promotional Materials Catalogue. CDC has developed a catalogue of resources (i.e., campaigns and advertisements, sample newsletter articles, social media posts, postcards, radio scripts, and more) focused on supporting organizations scaling the National DPP in underserved areas across the country. The priority populations served by these resources include: Medicare beneficiaries, men, African Americans, Asian Americans, Hispanics, American Indians, Alaska Natives, Pacific Islanders, and noninstitutionalized people with visual impairments or physical disabilities.
- The Program Champion Strategy Toolkit can help Lifestyle Coaches reach new participants through relationship-building and storytelling. By planning virtual “coffee dates” or creating engaging videos to share on social media, program champions can reach potential participants in the community—even when face-to-face time is limited.
- The Discovery Session Facilitator’s Guide for Live Video Conferencing provides step-by-step instructions for conducting Discovery Sessions when face-to-face meetings are not possible. The Discovery Session is a 60-minute introductory session (also known as “session zero”) designed to help CDC-recognized organizations recruit and enroll participants into the National DPP lifestyle change program.
- The Monthly Promotional Materials incorporate U.S. holidays and awareness events into National DPP recruitment materials to help engage participants using relevant topics. These resources include modifiable social media posts and images, public service announcement live announcer scripts, articles, e-newsletters, and more.
CDC has also developed resources to assist organizations in developing and promoting general marketing materials, as well materials aimed at recruiting priority populations. A comprehensive list of all available marketing materials is available here. Included in this list is a set of three videos of participant testimonials. These videos offer real-life examples of participant experiences with the National DPP lifestyle change program.
Michael Jones: “The motivation for me is to watch my children grow and be here for them. And that starts with taking care of myself and my body.”
Timing: 3:25
Suzi Gomez: “I prevent type 2 diabetes so I can keep traveling, taking pictures, and enjoying my family the rest of my life.”
Timing: 1:58
Cynthia Johnson: “It’s not about how long you live, it’s about how well you live.”
Timing: 2:19
The experiences of three additional participants in the National DPP lifestyle change program can be found here.
NACDD has generalized the MCO Phone Call Script for Outreach to Medicaid Beneficiaries that was developed by the Virginia Department of Health MCO pilot. It gives example language for an MCO or other partner to perform initial outreach about the National DPP lifestyle change program to Medicaid beneficiaries identified with prediabetes or at high risk for developing type 2 diabetes.
Recruitment Strategies in Practice
Minnesota
The Minnesota Department of Health, in concert with its partners, used several recruitment strategies. Over time, they determined that in-person recruitment by clinic staff, especially primary care providers, was the most effective way to recruit Medicaid beneficiaries to the National DPP lifestyle change program. The Minnesota Department of Health also used the following recruitment strategies:
- Mailed engaging postcards to Medicaid beneficiaries about the opportunity to participate in the National DPP lifestyle change program.
- Communicated about prediabetes and the National DPP lifestyle change program opportunity through local media outlets including bus stations, local radio, and community newsletters.
- Partnered with clinics to provide National DPP lifestyle change program-related information at community health fairs and other events.
In 2019, NACDD, Leavitt Partners, and the Minnesota Department of Health partnered to compile evidence- and experience-based best practices on recruitment, enrollment, and retention into a single Best Practices Guide. The guide is written for lifestyle coaches and program coordinators who serve low income, Medicaid-eligible participants. However, many of the principles discussed in the guide could be used by any stakeholder working to increase recruitment, enrollment, and retention in the National DPP lifestyle change program and would apply to all eligible participants.
In conjunction with the Best Practices Guide, the Minnesota Department of Health released a series of videos interviewing lifestyle coaches and program coordinators that emphasized the strategies discussed in the guide. The recruitment strategies mentioned in the video series include:
- Utilizing community health workers (CHWs) as lifestyle coaches to reach National DPP lifestyle change program participants.
- Engaging with partners and building relationships with health care providers, including health care providers during their training, such as nursing students.
- Encouraging enrollment through a video directed to potential program participants.
Montana
A program manager from the Montana Department of Public Health and Human Services (DPHHS) described their recruiting efforts as follows:
Outreach to Medicaid Passport Providers (i.e., health care providers enrolled to deliver Medicaid services)
Health care providers who were enrolled to deliver Medicaid services received a mailing that included a cover letter signed by the state medical officer, a report showing National DPP lifestyle change program outcomes, a brochure explaining the program, and a sample referral form. In subsequent years members of the Montana DPHHS did mailings coupled with direct phone outreach (facilitated by a contractor) to speak to the health care providers about the National DPP lifestyle change program. The program manager indicated that her understanding was that the best way to promote the program was through health care providers.
Direct Outreach to Medicaid Beneficiaries Based on Claims Data
Medicaid beneficiaries with claims data that indicated they may be eligible for the National DPP lifestyle change program received a mailing that included a cover letter and brochure about the program. In subsequent years members of the Montana DPHHS did direct outreach to Medicaid beneficiaries by phone. They indicated on the phone that they could set the beneficiary up with a Lifestyle Coach who could contact them, and then the Montana DPHHS followed up with interested individuals with a postcard. The program manager noted that when using this method several individuals needed to be contacted to generate an enrollee in the National DPP lifestyle change program, and the Montana DPHHS was challenged to meet its enrollment goal. She also noted that this type of outreach may not be feasible for large populations of individuals with prediabetes.
Frequent communication
Members of the Montana DPHHS made numerous presentations to coalitions and health care provider groups. They also created general brochures that were distributed to local CDC-recognized organizations and displayed in public places.
Peer-reviewed research
Once a year the Montana DPHHS published a publication in a peer reviewed journal to show program outcomes.
Maryland
Maryland participated in the Medicaid Coverage for the National DPP Demonstration Project funded by CDC and managed by NACDD. Some lessons learned from the Demonstration regarding recruitment and enrollment include:
- Recruitment and retention success depended heavily on the participating MCOs’ traditional communication vehicle with its members. For example, while text messages worked well with one MCO that frequently communicated via text, texts from another MCO that did not traditionally communicate via text resulted in many confused members and was not successful.
- When reaching out to members, mentioning the beneficiary’s health care provider’s name resulted in more referrals.
- Targeted mailers provided an initial touch point with eligible members, but it was more successful to follow the mailers up with a live or automated phone call.
- Class reminders from the MCO or CDC-recognized organization sent via phone and/or email prior to the first class and before every class helped recruit and retain participants.
- Enlisting a health care provider champion helped with marketing the National DPP lifestyle change program. For example, one MCO had a medical assistant who was eligible for the National DPP lifestyle change program working on recruiting efforts. This person was a powerful advocate because they could speak about the program from personal experience.
Oregon
Health Share of Oregon was one of the Coordinated Care Organizations that participated in the Medicaid Coverage for the National DPP Demonstration Project funded by CDC and managed by NACDD. Below are some of Health Share of Oregon’s best practices and lessons learned about recruitment.
Best Practices:
- Hold a “session zero” to introduce the program and develop commitment among participants.
- Connect with potential participants at community events (e.g., farmers’ markets, neighborhood events/fairs, etc.).
- Recruit potential participants through relevant media (e.g., Chinese language newspaper).
- Ensure that individuals doing cold calls about the National DPP lifestyle change program are familiar with the program.
- Educate health care providers about the National DPP lifestyle change program and partner with clinics to perform outreach.
Lessons Learned:
- Word of mouth can be effective in some communities.
- Clinic referrals can be challenging. Start with one health care provider who can be a program champion.
- It can be difficult to obtain health care provider support for a short-term program, especially when it is only available to a subset of patients (e.g., Medicaid beneficiaries).
- It is helpful to have pre-existing contracts or relationships with the organizations/clinics from which you are recruiting.
- The recruitment window should be long enough to set up smooth procedures and processes.
- Outreach through cold calls may not be the most productive outreach method.
- It is helpful to have one universal referral form, and a central hub and point person for referrals and filling classes.
Commercial Health Plans
One commercial insurer employs multiple recruitment strategies to reach out to eligible individuals. It holds wellness events to help identify individuals who are eligible for the program and to encourage participation. To reach those who do not attend the wellness events, a direct mail campaign is employed, followed by an email blast. The insurer found that the direct mail and email combination was much more effective than direct mail alone.
Another insurer, after identifying eligible individuals and notifying health care providers of patient eligibility, sends personalized letters to patients that includes their health care provider’s name. The letter indicates that the health care provider understands that the patient has prediabetes and would benefit from participation in the program. Health plan staff note that referencing the health care provider in this context significantly increases the individual’s likelihood of participating. The insurer then reports information on participating patients back to the health care provider.
Anthem Colorado
Anthem Colorado markets the National DPP lifestyle change program through multiple avenues. The most effective has been working with health care providers to generate referrals. Anthem Colorado also encourages employers to promote the program, sends emails to employees, and holds health fairs at worksites where employees can participate in a biometric screening to determine eligibility. Finally, Anthem Colorado markets the National DPP lifestyle change program on the Anthem website.
Omada
Omada is a CDC-recognized organization that delivers the National DPP lifestyle change program through an online format. Omada outreaches to potential participants using a variety of methods including email (where possible), direct mail, and on-site marketing at workplaces. It also promotes direct point of care referrals among health care providers.
Solera Health
Solera Health, a preventive care benefits manager, contracts with health plans and employers that cover the National DPP lifestyle change program. It manages all recruitment into the program and reaches out through a variety of methods based on the sponsoring entity and the contact data available. Methods used to engage members include email, text messaging, phone calls, and internal communications. Solera is also integrated into several benefit aggregators and health management platforms that identify qualified individuals. Members qualify either based on blood test results or based on the online CDC diabetes risk questionnaire. Once qualified, a series of questions are asked to match participants with their best-fit diabetes prevention program. Solera has found that 70% of individuals who go through this full process ultimately enroll.
Medicaid Coverage for the National DPP Demonstration Project Recruitment Brief
NACDD, with funding from the Division of Diabetes Translation at CDC, led the Medicaid Coverage for the National DPP Demonstration Project with Maryland and Oregon to show how state Medicaid agencies and state health departments can collaborate to implement, deliver, and sustain coverage of the National DPP lifestyle change program.
A summary of strategies used in the Demonstration to support recruitment can be found in the Medicaid Coverage for the National DPP Demonstration Project Recruitment Brief. This resource includes strategies for state Medicaid agencies, state health departments, MCOs, accountable care organizations (ACOs), and CDC-recognized organizations.Referrals
Many entities promoting the National DPP lifestyle change program have found that individuals are more likely to enroll in the program when referred by their health care provider. However, despite the strong evidence base supporting the effectiveness of the National DPP lifestyle change program in preventing type 2 diabetes, the number of health care provider referrals to the program have remained low. For example, a national survey of 2,341 individuals that were eligible for the National DPP lifestyle change program based on self-reported data found that only 4.2% reported ever being referred to the program, and that 25% of the individuals who had never been referred were interested in the program.
Why aren’t more health care providers referring to the National DPP lifestyle change program?
While a number of barriers to referrals exist, an initial barrier is health care provider awareness of and perspective on prediabetes and the National DPP lifestyle change program. For example, a national survey of 1,000 primary care physicians found that, of the 298 physicians who responded to questions about prediabetes, only 31% knew the correct value for A1C tests and only 42% knew the correct fasting glucose levels for a proper prediabetes diagnosis. On average, the physicians surveyed correctly chose only 10 of 15 prediabetes risk factors, most often missing the risk factors of being African American or American Indian race. More information about this study can be found here.
Additionally, some health care providers have perspectives that likely hinder referrals to the program, such as concerns about over diagnosing prediabetes, or that their patients lack the motivation to be successful in the National DPP lifestyle change program. Concerted efforts to educate health care providers about prediabetes and the National DPP lifestyle change program is likely necessary to increase the number of health care provider referrals.
Health care providers can be educated about the National DPP lifestyle change program through regular communication channels, in-clinic presentations, or through member associations. The American Medical Association (AMA) has tips on how to present to health care providers to increase awareness, engagement, and education on the National DPP lifestyle change program, as well as a presentation template for making the business case to health care providers to offer the National DPP lifestyle change program to patients. The AMA also offers health care providers an interactive guide designed to assist with a type 2 diabetes prevention strategy in clinical systems. To learn more about the guide, see this video.
Once health care providers understand the importance of referring to the National DPP lifestyle change program, system-level changes will also likely be necessary to support referrals, such as developing a streamlined process to create and transmit the referral, creating point of care or care management processes to identify patients who are eligible for the program, and setting up a bi-direction referral system with CDC-recognized organizations. To learn more about these system-level changes, see the How Referrals Work and the Bi-directional Referrals Between Health Care Providers and CDC-Recognized Organizations sections below.
The AMA has collaborated with health care organizations across the country to build sustainable diabetes prevention strategies. In 2017, the AMA formed the Diabetes Prevention Best Practices Workgroup (DPBP) with representatives from 6 health care organizations actively implementing diabetes prevention. Workgroup members distilled their strategies into best practice recommendations for three strategy maturity phases. The full study is available here.
CDC has developed a marketing and promotion resource titled Strategies that Work: Engaging Health Care Providers as Program Promotion Partners, available here*. For more helpful resources, visit the National DPP Customer Service Center’s National DPP Resources for Engaging Health Care Providers page.
Health Care Provider Videos – Prediabetes and the National DPP
These videos were developed to encourage health care teams to work together and with their patients to identify prediabetes and increase referrals to the National DPP lifestyle change program. These videos were created by NACDD in collaboration with the AMA and through support from the CDC, Division of Diabetes Translation.Team-Based Care: Clinical Care Management and the National DPP
This video, based in a hospital, highlights the responsibility of care management in implementing and sustaining effective diabetes prevention strategies by health care providers, including referrals to the National DPP lifestyle change program.
Timing: 3:18 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Team-Based Care: Clinical Care Team Roles and Responsibilities for Diabetes Prevention
This video, based in a clinical setting, explores the different roles health care team members can play in identifying patients with prediabetes and providing care and follow-up, including referrals to the National DPP lifestyle change program.
Timing: 4:05 (Note: both Team-Based Care videos are the same until 1:16)
Audience: Clinical Care team (physician, medical assistant, front desk staff, care manager, practice manager, care coordinator, nurse, provider, etc.)
Clinical Care: Prediabetes Identification and Treatment
This video illustrates how health care providers can help their patients address prediabetes through referral to the National DPP lifestyle change program.
Timing: 4:18
Audience: Clinical Care team (physician, nurse practitioner, physician’s assistant, nurse, medical assistance, care manager, care coordinator, etc.)
How Referrals Work
There are two steps for a health care provider to make a referral to a CDC-recognized organization:
- Create a referral form
- Transmit the referral to the CDC-recognized organization
Much of the information in this section is based on an AMA, CDC, and YMCA webinar that was held September 24, 2018 called “Bi-Directional Referrals to the National Diabetes Prevention Program.”
Create a Referral Form
The National DPP lifestyle change program referral form should include up-to-date information about the patient and the referring health care provider. It is especially helpful to include the health care provider’s patient’s preferred contact method and the lab test results or diabetes risk test results that were used to establish eligibility for the program. An example referral form from the AMA can be found here.
Health care providers are more likely to refer individuals to the National DPP lifestyle change program if the referral process is simple and convenient. Perhaps the easiest referral method is to generate an electronic referral form directly within the electronic health record (EHR). The electronic referral form may include fields that are automatically populated with EHR data, such as the lab test results. Suggestions from the AMA on how health care providers can optimize their EHR to increase referrals to the National DPP lifestyle change program can be found here.
Alternatively, a paper referral form can be used. While paper forms are less convenient, they are a simple way to get referrals started if a health care provider’s EHR is not set up to generate an electronic referral form. One organization that was not able to generate electronic referral forms within the EHR developed a “smart phrase” that pulled key referral information from the EHR into a text document that could be printed.
Transmit the Referral to the CDC-Recognized Organization
Once the referral form is created, there are several methods to transmit the referral to the CDC-recognized organization, including by electronic transmission, autofax, and manual fax.
Electronic transmission is the easiest transmission method for health care providers to use, but the most challenging to set up. It requires an electronic interface between the health care provider’s EHR system and the CDC-recognized organization’s EHR or data management system. One health care provider and CDC-recognized organization were able to share referrals through electronic transmission by using the EHR’s direct messaging feature.
Some organizations have found the use of autofax to be a more practical approach because it is easier to set-up than electronic transmission. The electronic referral form is still generated within the EHR, and then the referral form is faxed automatically to the specified location.
The final option is to print the electronic referral form and manually fax it to the CDC-recognized organization. A paper referral form can also be manually faxed. This approach is less convenient for the health care provider and does not automatically record the referral within the EHR, however, it requires a minimal investment of time and resources to set-up.
Referral Workflow
Health care providers may choose one of the following approaches to referring to the National DPP lifestyle change program:
- Point of care approach: In this approach, health care providers refer patients to the National DPP lifestyle change program in person when a patient comes for an appointment. Other members of the care team can be used to streamline the referral process. For example, an EHR alert could be set up to alert health care providers that a patient coming into the office is eligible for a referral to the National DPP lifestyle change program. A medical assistant could then prepare the referral form during the rooming process, so it is ready before the patient arrives and only requires approval by the health care provider.
- Care management approach: Under this approach, health care providers proactively identify patients who are eligible for the National DPP lifestyle change program and contact them to refer them to the program. For example, a letter could be sent to individuals eligible for the National DPP lifestyle change program stating that their health care provider recommends them for the program. When this approach is taken, it may be the first time the individual is learning of their prediabetes diagnosis, so it is important to explain what prediabetes is and invite the individual to contact their health care provider for more information. The AMA has developed sample patient outreach letters and materials in English and Spanish that health care providers can give patients to educate them about prediabetes and the National DPP lifestyle change program.
Whatever methodology is chosen for referring individuals to the National DPP lifestyle change program, the Participant Identification and Engagement Workflow can be an important resource for defining and communicating that referral process to applicable entities. This tool is meant to assist state partners in brainstorming and developing individual workflows related to participant identification, outreach, referral, and engagement, as well as screening for health-related social needs (HRSN). Please visit the Medicaid and HRSN page to learn more about the role of Medicaid in addressing HRSN. Additional information on developing process workflows, including examples, are available on the Screening and Identification page of the Coverage Toolkit.
Bi-Directional Referrals Between Health Care Providers and CDC-Recognized Organizations
A key way to encourage health care providers to continue to refer individuals to the National DPP lifestyle change program is to create a bi-directional referral system, meaning a referral system where the health care provider receives information back from the CDC-recognized organization regarding the status of any referrals. CDC-recognized organizations can share information such as whether a referred individual was successfully contacted, whether the referred individual enrolled in the National DPP lifestyle change program, and the referred individual’s progress in the program. By providing this information, the CDC-recognized organization can build rapport with the health care provider and the health care provider can see first-hand evidence of the effectiveness of the National DPP lifestyle change program.
Health care providers and CDC-recognized organizations should work together when developing a bi-direction referral system to determine the desired frequency and level of detail of referral progress reports. A sample progress report from the AMA can be found here. Some health care providers have found it helpful to receive progress reports at the following milestones:
- When referred individuals enroll in the National DPP lifestyle change program;
- 8 weeks after the program start;
- 16 weeks after the program start;
- 6 months after the program start; and/or
- At program completion.
In the progress report, the health care provider may want to know about:
- The referred individual’s program attendance;
- The referred individual’s progress in meeting their weight loss and minutes of physical activity goals (e.g., a table with the individual’s weekly progress compared to their goal); and
- Any remarkable qualitive successes (e.g., completed their first 5k, lowered their medications, etc.).
Health care providers can also help increase retention by encouraging their patients who are attending the National DPP lifestyle change program to keep going, or by contacting patients who have missed multiple classes.
Challenges to Implementing Bi-Directional Referrals
Competing Priorities
Competing Priorities
- Currently, most health care systems are working on new processes to move from volume to value-based care. While health care providers recognize that diabetes prevention should be part of that transition, they are busy with other system changes and may not have time to set up a bi-directional referral system.
- Health care providers’ patients are often focused on concerns other than diabetes prevention when they come into the office.
- There are currently no available quality measures to measure a health care system’s progress in diabetes prevention, which results in less incentive to engage in this effort. However, the AMA is in the process of developing quality measures for diabetes prevention. We will continue to update this site as information becomes available. Additional information on the development of a prediabetes quality measure can be found here.
Resources Needed
Resources Needed
- Launching a referral system can require an investment of time from several staff members, particularly if an electronic referral system is used. Some considerations include:
- Who provides administrative and IT support?
- Who identifies individuals that qualify for the National DPP lifestyle change program?
- Who generates the referral?
- Who provides patient education?
- Who communicates the progress of participants in the National DPP lifestyle change program between the health care practice and the CDC-recognized organization?
- Resources will also be needed to train the health care team how to use the referral system.
EHR Sophistication
EHR Sophistication
- EHR sophistication varies among health care providers and CDC-recognized organizations.
- Most EHR vendors offer some functionality to create referrals for CDC-recognized organizations, but it almost always requires customization. Such customization can require significant resources or may take too long to implement.
- Health care providers often prefer to use their EHR to generate referrals, rather than an external application. However, health care providers may be willing to use an external application if it addresses other high priority health conditions as well as prediabetes.
Interoperability
Interoperability
- Lack of Health IT (HIT) interoperability is one of the biggest barriers to electronic transmission of referrals.
Data Security/Handling
Data Security/Handling
- Many data security concerns can be overcome by the execution of a business associate agreement between the health care provider and the CDC-recognized organization.
- Referrals could have HIPAA implications that health care providers should discuss with their legal representation.
- Some health care providers will want to integrate data from the CDC-recognized organization into the EHR, while others will want the data tagged as outside information. For example, the EHR can be updated with new patient weights submitted by the CDC-recognized organization.
Bi-Directional Referral Best Practices
- Use project management principles to approach the development of a bi-directional referral system and pick an appropriate project team to support the work.
- Identify a health care provider champion who is passionate about diabetes prevention, can co-lead the project, and can help educate fellow clinicians and leadership.
- Tie bi-directional referral efforts into existing organizational priorities. For example, if health care providers have already committed to type 2 diabetes management, use the type 2 diabetes management infrastructure for diabetes prevention.
- Explore other referral management solutions within the organization. For example, is another department using a solution that would be helpful?
- Involve stakeholders early in the referral system planning process. For example, health care providers and CDC-recognized organizations should work together to develop a bi-directional referral system designed for the information to be shared.
- Build trainings on the referral system into standing meetings with staff.
- Take a phased approach. Leverage technology where possible, but if you need to get going, start with the low-tech version.
To learn about Maryland’s bi-directional referral system, please see the Maryland CRISP example below.
Referral Strategies in Practice
ACPM Demonstration
The American College of Preventive Medicine (ACPM) established a demonstration project to fund clinical practices to develop and implement protocols for screening, testing, and referring patients to the National DPP lifestyle change program. ACPM has published two case studies that document the approaches, barriers, scalability plans, and lessons learned from six health care organizations from various types of organizations. The case studies can be found here and here.
Denver Health
Denver Health used a variety of recruitment methods and found health care provider referrals to be the best source for enrolling at-risk individuals. Approximately 1 in 10 at-risk individuals would enroll (i.e., verbally commit to participating in a session) when contacted by a lifestyle coach, whereas nearly 1 in 2 individuals would enroll if referred by their health care provider.
Denver Health identified individuals eligible for the National DPP lifestyle change program using EHR data, and invited the eligible individuals’ health care provider to refer their patients to the program. National DPP lifestyle change program staff then followed up with those patients by phone, indicating that the patient had been referred by their health care provider. This proved to be a highly effective referral and recruitment process.
Denver Health took a number of steps to promote health care provider referrals. In an article published in Association of Diabetes Care and Education Specialists (ADCES) in Practice (formerly American Association of Diabetes Educators (AADE) in Practice), authors Natalie Ritchie and Tamara Swigert of Denver Health summarize their health care provider engagement strategies as follows:
- Teach health care providers about the National DPP lifestyle change program using in-clinic presentations.
- Notify health care providers of new classes and referral processes.
- Create a diabetes risk registry to identify eligible patients for health care providers.
- Actively prompt health care providers to refer eligible patients.
- Provide regular updates on patient progress.
Anthem Colorado
Health care providers in Anthem Colorado’s network play a significant role in referring patients to the National DPP lifestyle change program. 70-80% of Anthem’s primary care physicians are in a value-based payment arrangement, in which the physicians may earn shared savings by reaching cost and quality targets. This means that many of their processes are focused on improving patient outcomes and decreasing the total cost of care. The National DPP lifestyle change program fits well within this focus, so physicians are supportive of referring patients to the program. Anthem markets the program to health care providers through its website, in regular formal communications, and in engagements with the value-based care physicians. An integrator that oversees the program for Anthem works directly with the health care providers on outreach activities, which typically results in an increase in referrals and enrollment.
Montana
A program manager from the Montana Department of Health and Human Services indicated that it is valuable to have good relationships with health care provider champions who can promote the program, and who can encourage local health care providers to make referrals. She also expects that making ties with medical associations for purposes of promoting the program to health care providers would also be helpful. Find more information on the Montana Diabetes Prevention Program here and on the Montana State Story page.
Maryland CRISP
To reduce type 2 diabetes rates, Maryland Medicaid has worked closely with Chesapeake Regional Information System for our Patients (CRISP), the state designated health information exchange (HIE), to identify individuals eligible for participation in the National DPP lifestyle change program and facilitate referrals through a closed-loop electronic referral process.
CRISP uses various data sources to identify individuals with prediabetes who are likely eligible for the National DPP lifestyle change program. CRISP then generates a “Care Alert” for these individuals that communicates eligibility to their health care provider(s). CRISP also uses monthly “SmartAlerts” to alert MCO case management teams of potentially eligible individuals on their rosters. CRISP’s closed-loop (i.e., bi-directional) referral tool (eReferral) allows health care teams to refer eligible individuals to outside organizations offering the National DPP lifestyle change program, and to receive referral status and enrollment updates on the referred individuals.
To learn more about Maryland’s CRISP prediabetes flag and eReferral tool, please see the CRISP Prediabetes Flag and eReferral Overview document and please watch the June 9, 2022 NACDD General Member Webinar, Making an Impact on Population Health: Utilizing a State-wide Health Information Exchange to Promote the National Diabetes Prevention Program.
Participant Readiness
To support enrollment of eligible participants in the National DPP lifestyle change program, staff can use the stages of change to understand participant readiness throughout the recruitment process. The Diabetes Training and Technical Assistance Center (DTTAC) has developed a resource, Tips for Exploring Readiness to Engage in the Lifestyle Change Program, which provides descriptions and suggestions for implementation related to the six stages of change, which include:
- Pre-contemplation – Unaware of the problem or has no interest in change
- Contemplation – Aware of the problem and beginning to think about change
- Preparation – Realizes benefits of making changes and thinking about how to change
- Action – Has made overt change in the last six months
- Maintenance – Has maintained changed behavior for more than six months
- Relapse – Returned to old behaviors
Once staff are familiar with the stages of change, organizations can implement readiness assessments to determine which stage participants are in. Readiness assessments could include survey methods similar to the DTTAC Readiness to Change Questionnaire, Montana’s Participant Readiness to Change Questionnaire, or Iowa’s Diabetes Prevention Program Considerations for Readiness. Staff can consider including readiness assessments in participant enrollment paperwork as shown in the DTTAC Participant Enrollment forms (available in both English and Spanish). After conducting a readiness assessment, any communication with eligible participants can be tailored to appropriately match the individual’s current stage of change. Lifestyle Coaches interested in understanding and implementing readiness assessments and other retention techniques can visit DTTAC’s Common Ground online learning community.
Additional information on providing tailored communication based on readiness level is also available in the P2P resource, described in the Recruitment Resources section above. The P2P can be used to guide potential participants who are in the contemplation stage into the preparation and action stages by providing answers to common questions and addressing potential barriers to enrollment.
Motivational Interviewing
When discussing change through evidence-based interventions, it is also helpful for recruitment staff to understand the benefit of incorporating motivational interviewing techniques into conversations with potential and current program participants. Motivational interviewing is a communication style designed to strengthen personal motivation for and commitment to a specific goal by exploring a person’s reasons for change in an atmosphere of acceptance.
*This resource was supported by Cooperative Agreement Number NU58DP006364-03-00, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services