Health Equity → Health Equity and the National DPP → Role of Medicaid in Addressing HRSN
The Role of Medicaid in Addressing HRSN
Establishing Medicaid coverage for the National Diabetes Prevention Program (National DPP) lifestyle change program has created partnerships between Medicaid, public health, managed care, health care providers, and community-based organizations (CBOs). Many of these same partners are also involved in efforts to reduce health disparities, address root causes that influence social determinants of health (SDOH) and increase health equity for Medicaid beneficiaries.
A Medicaid Coverage Learning Collaborative webinar below introduces the roles of Medicaid and other partners in that intersection between addressing SDOH and health care needs for Medicaid beneficiaries. It also discusses how the National DPP lifestyle change program, and CDC-recognized organizations that offer it, could play a role in supporting this work.
This page contains the following sections:
- Medicaid Beneficiary Profile
- Addressing HRSN Through Program Supports
- Using Medicaid Policy and Contracting to Advance Health Equity
Medicaid Beneficiary Profile
About one in five people in the United States is enrolled in Medicaid. Medicaid serves as a major source of health care coverage for low-income individuals and people from racial and ethnic minority groups. Medicaid beneficiaries are more likely to have lower health status than those on private insurance, are disproportionately women and people from racial and ethnic minority groups, and often experience multiple health-related social needs (HRSN). The Medicaid Beneficiary Profile below describes demographic characteristics of Medicaid beneficiaries and discusses the HRSN of Medicaid enrollees. You can access a PDF of the Medicaid Beneficiary Profile here.
When compared to adults on private insurance, Medicaid and Children’s Health Insurance Program (CHIP) beneficiaries have a lower health status across many metrics including but not limited to the following:
See CMS’ Medicaid Facts and Figures for more health status information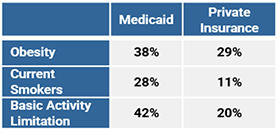
Addressing HRSN Through Program Supports
Some CDC-recognized organizations use program supports to enhance enrollment and retention and address HRSN in ways that are tailored to the individual. In this context, program supports are items, services, and activities that:
- Reinforce information in the curriculum. Examples include measuring cups and cooking demonstrations.
- Remove barriers to participation. Examples include transportation vouchers, weight scales, mobile devices, and prepaid phone minutes or data.
- Address social determinants of health. Examples include access to healthy foods and referrals to community resources.
- Promote social support and connectedness. Examples include one-on-one meetings with the Lifestyle Coach and social media groups.
An evaluation of Medicaid Incentives for the Prevention of Chronic Diseases (MIPCD) grants demonstrated the benefit of using program supports in the National DPP lifestyle change program. Evaluation findings from Minnesota, Montana, Nevada, and New York found that participants receiving program supports had significantly higher attendance (attended 1‒2 more sessions) than control groups without program supports. However, beneficiaries indicated that while program supports served as a hook to get them enrolled, they were not the driver behind continued participation. Reaching goals, starting to feel better, and establishing a relationship with a Lifestyle Coach were what kept them engaged.
To learn more about the characteristics of effective program supports, please visit the Retention page of the Coverage Toolkit.
State Examples
Minnesota
In Minnesota, several CDC-recognized organizations are offering participants a free bag of groceries at each session, a free three-month YMCA membership, free personal training sessions, and material items such as t-shirts and cups.
Mississippi
Mississippi Public Health has collaborated with the Department of Agriculture to expand the Supplemental Nutrition Assistance Program (SNAP) program benefits and deliver additional food to participants in the National DPP lifestyle change program.
Virginia
Virginia is working to roll out an initiative that provides healthy food vouchers and childcare stipends to participants in the National DPP lifestyle program as they meet predetermined milestones.
For additional examples of states utilizing various types of program supports in the National DPP lifestyle change program, please visit the Retention page of the Coverage Toolkit.
Medicaid and Program Supports
Many state Medicaid programs and Medicaid managed care organizations (MCOs) operate beneficiary incentive programs to support healthy behaviors. The supports used in these programs range from reductions in cost sharing (a discount that lowers that amount paid for deductibles, copayments, and coinsurance), to the ability to choose products from catalogues, to gift cards or vouchers for specific vendors (i.e., not redeemable for cash), and more.
It is important to note, however, that there are state and federal regulations regarding how Medicaid beneficiary incentives and program supports can be designed, delivered, and marketed. Rules may also vary on a state-by-state basis and differ depending on what entity (the state, an MCO, Medicaid provider, or other third party) is providing the program supports.
Given the complexity of these regulations, public health and CDC-recognized organizations should coordinate with their state’s Medicaid agency when developing a program support system for Medicaid beneficiaries participating in the National DPP lifestyle change program and beyond. Four benefits to coordinating with the state Medicaid agency are listed below.
First, it is good practice to involve Medicaid program administrators in any initiative that will impact Medicaid beneficiaries. Program administrators can provide valuable feedback on potential impacts the program supports may have on the Medicaid population, help with implementation efforts, provide guidance on any potential federal matching dollars, and facilitate coordination and outreach with Medicaid beneficiaries
Second, many Medicaid programs and MCOs have existing program supports in place. Adding another support may create confusion around the existing programs. Coordination with the Medicaid agency can help ensure that any new program support will align with existing or planned initiatives.
Third, financial eligibility for Medicaid differs by program and population type. Depending on how program supports are structured, they could impact the income calculations and reporting requirements for some beneficiaries in Medicaid and other needs-based programs (i.e., be interpreted as reportable income). While it is unlikely that program supports used for the National DPP lifestyle change program would make an individual ineligible for coverage, it is advisable to work with the state Medicaid agency to ensure the program supports are within any designated limits and will not jeopardize beneficiary eligibility.
Finally, MCOs have specific regulatory and contractual constraints on how to design and notify enrollees of program supports. For example, gift cards and vouchers are subject to applicable state and federal laws and regulations related to Medicaid managed care marketing activities and Social Security Act § 1128A, among others. MCOs and/or the Medicaid agency can provide guidance on these issues.
Using Medicaid Policy and Contracting to Advance Health Equity
Medicaid plays a key role in addressing HRSN. A variety of Medicaid related policy and contracting levers can be used to further health equity, including 1115 demonstration waivers, MCO contracting, and value-added services. Recent federal initiatives such as the U.S. Department of Health and Human Services’ Call to Action to Address HRSN are allowing states additional flexibility to better address social needs within Medicaid and across health care systems.
1115 Waivers
Section 1115 demonstration waivers (1115 waivers) are one example of a policy lever that can be used by states looking to further health equity through addressing HRSN. 1115 waivers provide states with additional flexibility to design, demonstrate, and evaluate new approaches to Medicaid.
In January 2024, CMS approved New York’s request to amend its 1115 waiver to allow the state to “advance health equity, reduce health disparities, support the delivery of HRSN, and promote workforce development.” The amended 1115 waiver includes: investments in HRSN via greater integration between primary care providers and community-based organizations; connecting people to critical housing and nutritional support services; workforce investments with a goal of equitable and sustainable access to care in Medicaid; and developing regionally focused approaches. For more information, see New York’s Medicaid Redesign Team approval letter.
In February 2024, CMS approved Oregon’s structure for how HRSN benefits will be delivered under the state’s 1115 waiver. Covered HRSN services include rent/temporary housing (including navigation services), housing costs (including utilities, moving costs, and housing deposits), meals and food access, and nutrition education. For more information, see Oregon’s HRSN Services Protocol Approval.
To learn about how North Carolina used an 1115 waiver to launch a pilot program examining the impact of providing evidence-based, non-medical services that address HRSN under Medicaid, please see the North Carolina state example on the Attaining Coverage Through a Section 1115 Demonstration Waiver page of the Coverage Toolkit.
More examples are provided in a report prepared by the Center for Health Care Strategies. The report also highlights the following common themes related to HRSN from several 1115 demonstration waivers:
- There is a focus on enhancing care coordination and community partnerships to address HRSN.
- New value-based payment initiatives are being developed and deployed to address HRSN.
- Demonstrations with healthy behavior initiatives do not typically connect to state SDOH initiatives. Fostering connections could save resources and allow demonstrations to build off existing work.
- Additional 1115 demonstrations that test the impact of targeted HRSN initiatives in managed care would be helpful to accelerate work towards health equity.
For more examples of states with approved or pending 1115 waivers that include HRSN or Delivery System Reform please visit the KFF’s Medicaid Waiver Tracker.
MCO Contracting
Contracting levers are important to consider when seeking to address HRSN. A national survey conducted by Manatt on state SDOH initiatives found that most states expect MCOs to address Medicaid members’ social needs, with care management being the most common method. Manatt identified the following key findings regarding what states have done to address HRSN through MCO contracts:
- SDOH requirements in MCO contracts are most commonly related to care management. Common MCO requirements related to SDOH include screening for HRSN, referring to social services, coordinating social services, coordinating with other state and federal programs, and partnering with CBOs to support members’ unmet HRSN.
- Many states utilize MCO contracts to target HRSN initiatives to certain Medicaid subpopulations such as women and children.
- Housing is the most common HRSN to be addressed in MCO contracts, followed by food, employment, transportation, and interpersonal violence.
Additional research and work around MCO contracting has revealed growing opportunities for states looking to address HRSN through contracting. A report prepared by the Center for Health Care Strategies identifies the following common themes around MCO contracting:
- There is a growing focus on SDOH in state managed care contracts.
- Most of these contracts address HRSN through care coordination and care management requirements.
- Innovative states have started to integrate SDOH elements into quality assurance and performance improvement requirements.
- Most states do not prescribe how MCOs can use existing flexibilities under federal law to provide services or interventions that address HRSN.
- Having payment incentives that are linked to HRSN are not yet commonplace.
- Some states provide financial incentives to address Medicaid beneficiaries’ HRSN, but this is still relatively uncommon.
For examples of states that have used Medicaid contracting requirements to address food security please see the National Academy for State Health Policy’s article on how states are advancing access to healthy food.
To learn more about MCO contracting, please visit the State MCO Contracts and Contract Amendments page of the Coverage Toolkit.
Value-Added Services
Value-added services are another policy lever within Medicaid that can be used to address HRSN. Value-added services fall outside direct care costs and are paid for by the MCO. Utilizing value-added services allows MCOs to address members’ service needs that are beyond the scope of what is traditionally covered by Medicaid and is an opportunity for MCOs to address HRSN. Examples of value-added services vary across plans and states, but typically include health education classes, dental and vision programs, or program supports like gym memberships or weight loss classes.
To learn more about how value-added services can address HRSN, please see Academy Health’s white paper, Implementing Social Determinants of Health Interventions in Medicaid Managed Care, and the technical assistance brief developed by Center for Health Care Strategies, Providing Value-Added Services for Medicare-Medicaid Enrollees: Considerations for Integrated Health Plans.
Value-Based Payments
There are a range of value-based payment (VBP) methods that incentivize quality and outcomes, and therefore emphasize preventive services. State Medicaid agencies are increasingly moving towards VBP models. The following VBP models can be used by payers and providers, including Medicaid, to improve outcomes:
- Shared savings model: encourages groups of physicians, hospitals, and other health care providers to come together to provide coordinated, high-quality care.
- Pay for performance: physicians, hospitals, and other health care providers are given financial incentives for meeting performance and quality objectives.
- Bundled payments: health care providers treating a patient for the same or related condition are paid an overall sum for treating the condition, instead of being paid for each service separately.
- Capitated payment models: the health plan enters a contract to provide comprehensive, coordinated care in exchange for a prospective capitation payment from CMS and the state.
- Global budgeting: providers are paid a fixed amount for treating a patient population over a defined period, instead of being paid for each service separately.
Blended Funding
States can blend Medicaid and non-Medicaid funding sources to address HRSN. Medicaid beneficiaries are often interacting with multiple departments and agencies to get social supports. Braiding funding from various sources can provide a coordinated approach within the state umbrella of agencies.
Data and Quality Improvement Strategies
Medicaid can work to identify where there are gaps in HRSN and demographic data and work to fill them by collecting more comprehensive data on HRSN within their populations. Developing a strategy within Medicaid for using data to support efforts around HRSN can also help address quality improvement.
In Lieu of Services and Settings (ILOS)
In January 2023, CMS released additional guidance for states on how to address HRSN through Medicaid, specifically through In Lieu of Services and Settings (ILOS). The guidance provides an innovative option states may consider employing in Medicaid managed care programs to reduce health disparities and address unmet HRSN. ILOS allows immediate or longer-term substitutes for Medicaid State Plan-covered services or settings in cases for which the substitutions can be expected to reduce the future need to utilize the traditional services or settings. CMS suggests that states utilize ILOS to strengthen access to care by expanding setting options and addressing HRSN of Medicaid beneficiaries. When used appropriately, ILOS can improve population health, reduce health inequities, and lower overall health care costs in Medicaid. States should consider the following principles to ensure ILOS are an appropriate and efficient use of Medicaid resources. ILOS must be:
- A means to advance the objectives of a State Medicaid program
- Cost effective
- Medically appropriate
- Provided in a manner that preserves beneficiary rights and protections
- Subject to appropriate monitoring and oversight
- Subject to retrospective evaluation, when applicable
On February 15, 2023, the Center for Health Care Strategies and Health Begins hosted a webinar, New CMS Guidance on Addressing Social Needs Through Medicaid, which provided resources and additional context for states considering the use of ILOS to expand services that address HRSN.
When considering applications for the National DPP lifestyle change program, states may consider how ILOS could be used to reduce barriers for participation in the program and address associated HRSN for program participants.
State Examples of Addressing HRSN Through Medicaid Policy
Arizona
Arizona Health Care Cost Containment System (AHCCCS), Arizona’s Medicaid managed care program, requires that MCOs cover certain non-clinical support services, including therapeutic foster care, housing support, transportation, childcare connections, and more.
Florida
Florida contractually requires MCOs to identify community supports and facilitate referrals for enrollees with identified needs. MCOs must also track the referral in the patient’s records and follow up to ensure receipt of services.
Kansas
KanCare, Kansas’ Medicaid managed care program, collects SDOH data through MCO Health Risk Assessments, member surveys, provider data systems that track National Outcomes Measures (NOMs), and cross-agency data sharing. This data collection informs quality improvement and helps to identify member needs.
New Mexico
New Mexico’s MCO contract stipulates that MCOs provide training to their care coordination teams around stable housing by engaging with a full-time “Supportive Housing Specialist”.
New York
New York’s State Department of Health created the Bureau of Social Care and Community Supports (BSCCS) within the state Medicaid agency, the Office for Health Insurance Programs. BSCCS works to implement VBP initiatives that require MCOs to include at least one SDOH intervention and contract with a CBO. BSCCS was authorized in the 2020-2021 state budget to provide medically tailored meals through an ILOS, allowing MCOs to cover the cost of the medically tailored meals as part of a SDOH pilot. The medically tailored meals program delivers meals that are designed to meet the individual needs of Medicaid members with chronic diseases, including diabetes.
Rhode Island
Rhode Island’s Medicaid “Accountable Entity” program is responsible for identifying the HRSN of Medicaid beneficiaries. Medicaid MCOs sub-contract with Accountable Entities (which are provider organizations) that are responsible for the total cost of care, quality, and outcomes for their attributed populations. Accountable Entities must identify three social needs domains, such as housing stabilization, education, food security, safety and domestic violence, employment, and transportation, and screen for social needs. Closer connections between providers and CBOs are encouraged via a Community Referral Platform, which helps Accountable Entities systematically screen and refer beneficiaries to social service entities and CBOs.
Virginia
Virginia created the Virginia Health Opportunity Index (HOI) to visually demonstrate the impact of SDOH on communities throughout the state, with county, health district, and legislative district dashboards. The HOI includes an overall statewide SDOH measure and 13 different SDOH measures from four domains (Community Environmental Profile, Economic Opportunity Profile, Consumer Opportunity Profile, and Wellness Disparity Profile).









