Medicaid → Medicaid Coverage → Attaining Coverage Through a Section 1115 Demonstration Waiver
Attaining Coverage Through a Section 1115 Demonstration Waiver
After a state has made the decision to cover the National Diabetes Prevention Program (National DPP) lifestyle change program in Medicaid, either through legislation or administrative rules, the state will determine how to claim federal Medicaid matching funds for the program. The most common way to claim federal Medicaid matching funds is by including the benefit in the Medicaid State Plan. If the policies or processes the state intends to implement for the National DPP lifestyle change program cannot be accomplished through the Medicaid State Plan, the state may choose to use a section 1115 demonstration waiver (1115 waiver) or another mechanism (see the Engaging MCOs to Attain Coverage page for examples of other mechanisms).
This page describes how the National DPP lifestyle change program can be included in an 1115 waiver, and includes the following topics:
- What is a Section 1115 Demonstration Waiver?
- Section 1115 Demonstration Waiver Examples
- 1115 Waiver Considerations
- About Delivery System Reform Incentive Payment (DSRIP) 1115 Demonstration Waivers
- DSRIP 1115 Demonstration Waiver State Examples
What is a Section 1115 Demonstration Waiver?
Section 1115 of the Social Security Act (the Act) gives the Secretary of Health and Human Services (the Secretary) the authority to approve experimental, pilot, or demonstration projects that promote the objectives of the Medicaid program. This section allows the Secretary to waive compliance with the Medicaid program requirements of section 1902 of the Act, as necessary to carry out the demonstration project. In addition, section 1115 allows the Secretary to provide federal Medicaid matching funds for demonstration costs that would not otherwise be considered federally matchable expenditures.
1115 waivers provide states with additional flexibility to design, demonstrate, and evaluate new approaches to Medicaid such as:
- Expanding eligibility to individuals who are not otherwise Medicaid or CHIP (Children’s Health Insurance Program) eligible;
- Providing services not typically covered by Medicaid;
- Using innovative service delivery systems that improve care, increase efficiency, and reduce costs.
Section 1115 waivers are used to make broad changes applicable across a state’s Medicaid program as well as more targeted changes applicable only to specific services or populations. Some state examples that demonstrate the diverse nature of the 1115 demonstrations include Arizona’s, which has its entire Medicaid program authorized under an 1115 demonstration, while Maine has an 1115 waiver specific to its low-income HIV/AIDS population, and several states maintain 1115 demonstrations just to cover family planning services and supplies.
Generally, if the policies or processes a state intends to implement for the National DPP lifestyle change program can be accomplished through the Medicaid State Plan, a state must use that mechanism. However, if the policies or processes a state intends to implement cannot fit within the existing Medicaid program requirements included under the Social Security Act, an 1115 waiver may be appropriate. For example, if a state currently offers managed care through an 1115 waiver and wants to offer the National DPP lifestyle change program to only Medicaid beneficiaries under managed care, the state could apply to amend the existing 1115 waiver to include the National DPP lifestyle change program.
While the primary purpose of the Medicaid program is to furnish medical assistance to low-income individuals and families, there are some other general criteria the Centers for Medicare and Medicaid Services (CMS) uses to determine whether Medicaid/CHIP program objectives will be met under the section 1115 demonstration waiver. These criteria include whether the demonstration will:
- Increase and strengthen overall coverage of low-income individuals in the state;
- Increase access to providers as well as stabilize and strengthen provider networks available to serve Medicaid low-income populations in the state;
- Improve health outcomes for Medicaid and other low-income populations in the state; and
- Increase the efficiency and quality of care for Medicaid and other low-income populations through initiatives to transform service delivery networks.
Demonstrations must also be “budget neutral,” meaning that over the course of the demonstration, federal Medicaid expenditures will not be more than what federal spending would have been without the waiver.
Generally, 1115 waivers are approved for an initial five-year period. The waiver can be renewed for an additional three to five years, depending on the populations served, and there is no limit on the number of times the waiver can be renewed. States commonly request and receive extension approvals. However, the waiver process can be burdensome on a state and there is no guarantee of reauthorization.
For more information about 1115 waivers, see the “1115 Waiver Considerations” section below or About Section 1115 Demonstrations from Medicaid.gov.
What are Federal Medicaid Matching Funds?
Medicaid services are paid for through funding from both state and the federal governments; the federal government matches state Medicaid spending according to a formula set in federal Medicaid law.
Federal Medicaid matching funds can be claimed for both direct service costs as well as administrative costs. The amount the federal government reimburses for direct service costs ranges from 50% to 100%, depending on the state’s Federal Medical Assistance Percentage (FMAP), the type of service delivered, and the location where the service is provided. Administrative costs are generally shared between the federal government and the state at a rate of 50/50, or in some cases at a higher rate of 75/25 or 90/10.
To claim federal Medicaid matching funds for the National DPP lifestyle change program, a state must have approval from the federal government through a Medicaid State Plan, a section 1115 demonstration waiver, or another mechanism (see the Engaging MCOs to Attain Coverage page for examples of other mechanisms).
A state could also choose to provide Medicaid coverage of the National DPP lifestyle change program using only state funds.
Section 1115 Demonstration Waiver Examples
Maryland
Attaining Federal Medicaid Matching Funds through a Section 1115 Waiver
HealthChoice, first implemented in 1997 under the authority of Section 1115 of the Social Security Act, is Maryland’s statewide Medicaid managed care program. Effective January 1, 2022, CMS approved and renewed Maryland’s HealthChoice 1115 waiver for a period of five years.
History of National DPP coverage in Maryland Medicaid: Maryland, along with Oregon, participated in the CDC-funded, NACDD managed Medicaid Coverage for the National DPP Demonstration Project from July 2016 to January 2019 that sought to demonstrate how state Medicaid agencies and state health departments can collaborate to implement, deliver, and sustain coverage of the National DPP lifestyle change program for the Medicaid population. To continue to pursue sustainable coverage of the program after the Demonstration concluded, Maryland submitted an amendment to their existing §1115 HealthChoice demonstration waiver.
On March 18, 2019, CMS approved an amendment to Maryland’s §1115 HealthChoice demonstration waiver, authorizing Maryland Medicaid to cover the National DPP lifestyle change program for eligible HealthChoice beneficiaries enrolled in managed care organizations (MCOs), effective July 1, 2019. That first waiver amendment that included the National DPP extended through December 31, 2021. The Code of Maryland Regulations, which outlines all required Maryland HealthChoice benefits, was also amended to include the program at this time.
To continue to receive federal Medicaid matching funds for the National DPP lifestyle change program for Medicaid managed care enrollees when the §1115 waiver expired December 31, 2021, Maryland pursued a renewal to the waiver, and on January 1, 2022, CMS approved and renewed Maryland’s §1115 demonstration wavier for five years. After 2026, Maryland could again pursue a renewal to the waiver or extend coverage of the program to fee-for-service (FFS) Medicaid beneficiaries and attain federal Medical matching funds by submitting a state plan amendment (SPA) to the Medicaid State Plan.
Although there are several ways a state could receive federal Medicaid matching funds when covering the National DPP lifestyle change program for Medicaid beneficiaries, Maryland chose a §1115 waiver due to the waiver’s flexibility to further test and evaluate the effectiveness of the program on the Medicaid managed care population.
To approve §1115 waivers and waiver amendments, CMS must determine that they promote the goals of the Medicaid program, which may include improving health outcomes and lowering spending. Each §1115 waiver includes a list of Special Terms and Conditions (STCs) that detail the budget neutrality of the demonstration, the extent of federal involvement in the demonstration, and the evaluation process for determining the demonstration’s spending and enrollment. Maryland is required to evaluate the National DPP component of the §1115 waiver according to the evaluation standards described in the STCs of the waiver. Moreover, in the STCs of Maryland’s National DPP waiver amendment, CMS stated it will “test the impact DPP has on all-cause hospital admission, medications, total cost of care, incidence of diabetes, and utilization of emergency medicine services.” Evaluating the impact of the National DPP lifestyle change program on these broader federal and state goals informs whether the demonstration was budget neutral and may help inform the return on investment of the program. Additional information on evaluation of the National DPP lifestyle change program can be found on the Data, Reporting, and Evaluation page of the Coverage Toolkit.
Maryland’s §1115 Waiver Language
Maryland’s waiver allows for all CDC approved delivery modes including in-person, online, distance learning, and combination, and allows delivery of the National DPP lifestyle change program to eligible Medicaid managed care enrollees between 18-64 years in age. Some of the key National DPP related language used in the approved waiver includes the following from the STCs:
“HealthChoice Diabetes Prevention Program (DPP). Effective July 1, 2019, the HealthChoice Section 1115 demonstration benefit package will include National Diabetes Prevention Program (National DPP) services. The specific program requirements are set forth in the National Diabetes Prevention Program (National DPP) administered by the CDC, including “Centers for Disease Control and Prevention Diabetes Prevention Recognition Program Standards and Operating Procedures (OMB No. 0920-0909).”
Eligibility Requirements:
Under the HealthChoice DPP, Medicaid eligible beneficiaries who receive services through HealthChoice managed care organizations (MCOs) and meet the CDC eligibility criteria are eligible for HealthChoice DPP services.
HealthChoice DPP Eligibility Criteria (Per currently-effective CDC Diabetes Prevention Recognition Program (CDPRP) standards):
- Receive services through a HealthChoice MCO;
- Between 18-64 years old;
- Overweight or obese (Body Mass Index (BMI) of ≥ 25 kg/m2; ≥ 23 kg/m2 if Asian); AND
- Elevated blood glucose level OR History of gestational diabetes mellitus (GDM)
Eligibility Exclusion:
Consistent with the CDC National DPP eligibility criteria, participants cannot have a previous diagnosis of type 1 or type 2 diabetes prior to enrollment. Individuals who are currently pregnant are not eligible for National DPP services.
HealthChoice DPP Services:
The HealthChoice DPP will provide services through any or all of the delivery modes outlined in the currently-effective CDC DPRP standards.
This expenditure authority for the HealthChoice DPP is conditioned on it not seeking funds for the HealthChoice DPP from a different funding source.”
North Carolina
North Carolina’s Healthy Opportunities Pilot
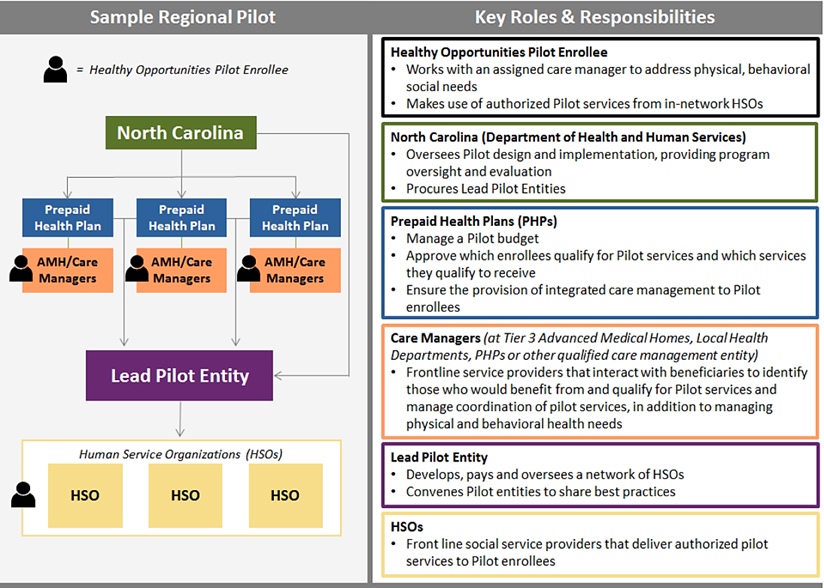
North Carolina Department of Health and Human Services (NCDHHS) recently launched the Healthy Opportunities Pilots, a program working in conjunction with the state’s transition to managed care to test and evaluate the use of Medicaid to pay for a select set of evidence-based interventions designed to address non-medical factors that drive health outcomes and costs. The program launched through a section 1115 waiver that runs through October 31st, 2024. CMS authorized up to $650 million in state and federal Medicaid funding for the pilots, which will cover the cost of delivering the non-medical services (including the National DPP lifestyle change program) and support capacity building needed to launch the program.
Pilot Regions and Eligibility
The pilot area will include up to three regions and is expected to serve approximately 25,000 to 50,000 beneficiaries, or about 1-2% of total Medicaid enrollees in the state. To be eligible for the pilot, individuals must be enrolled in a managed care plan (also called Prepaid Health Plans or “PHPs” in North Carolina) and must have at least one physical or behavioral risk factor and at least one social risk factor as defined by the Department (described on page 11 of this report). To maximize the impact of limited pilot funding, services are intended to be provided to members expected to benefit most, as determined by the PHPs.
Connecting Members to Pilot Services
The Healthy Opportunities Pilots will cover the cost of 29 interventions listed in the Department’s Pilot Services Fee Schedule. The services were selected based on their potential to improve health outcomes and/or lower health care costs. Services address housing, food, transportation, and interpersonal violence/toxic stress needs of qualified Medicaid members. The National DPP lifestyle change program is included under the food category. The graphic below outlines key roles and responsibilities and the process for how members are connected to the services they need. The lead pilot entity (now referred to as Network Leads) allows the Human Service Organizations (HSOs) (also known as community-based organizations (CBOs)), which could be a CDC-recognized organization providing the National DPP lifestyle change program, to invoice for services that the lead pilot entity then turns into claims to get payment from the PHPs. This payment pulls from the $650 million allocated for the pilots. The pilot payment facilitation process is similar to how umbrella hub organizations facilitate payment for subsidiary organizations.
More information on North Carolina’s section 1115 waiver and their Healthy Opportunities Pilot can be found at the links below:
- NCDHHS:
- Kaiser Family Foundation:
Oregon
Oregon Health Plan Health Evidence Review Commission and Prioritized List of Health Services
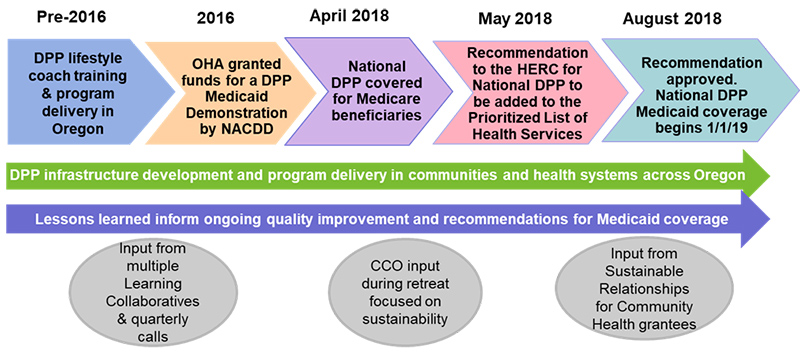
The graphic below shows the sequence of events that led to coverage of the National DPP lifestyle change program in Oregon’s Medicaid program, known as the Oregon Health Plan (OHP). These events follow the process established in Oregon’s 1115 waiver to add new covered benefits to the OHP.
Oregon Health Authority Coordinated Care Organizations
The OHP is administered through Coordinated Care Organizations (CCOs) in addition to the fee-for-service plan. A CCO is a network of all types of health care providers (physical health, addictions and mental health care, and dental care providers) who work together in their local communities to serve people who receive health care coverage under the Medicaid OHP. CCOs have similar features as ACOs and MCOs. To learn more about CCOs visit the OHP CCO page here.
Oregon created CCOs in 2014 to better serve the Medicaid population. CCOs are collaborations among communities, health care providers, health plans, and hospitals, and they are intended to integrate health care under global budgets that incentivize value-based service delivery and patient outcomes for OHP members. CCOs are focused on prevention, helping people manage chronic conditions, such as diabetes, and addressing chronic disease risk factors.
CCOs have multiple pathways to fund the National DPP benefit, which are outlined in section IV of the 2023 Companion Guide for Coordinated Care Organizations and Oregon Health System Partners Serving Oregon Health Plan Members (Companion Guide). For example, CCOs may choose to cover the program through the traditional medical billing model using CPT codes. Alternatively, a CCO may choose to implement the National DPP lifestyle change program in a community-based organization (CBO). A CCO may be motivated to contract with community-based organizations based on their expertise in serving OHP members in culturally specific manners, such as deploying lifestyle coaches who are bilingual or community health workers (CHWs). The CCO can choose to fund the National DPP lifestyle program through a CBO with an alternative payment method (APM) or value-based payment model (VBP), or by characterizing the funding as Health-Related Services (HRS). The CCOs can choose to categorize the expenses through a CBO as HRS, as long as the funds are not for covered services (for example, National DPP lifestyle change program participants that are both non-CCO members and CCO members, but the CCO members do not meet all the screening, diagnosis and eligibility for the National DPP lifestyle change program as a covered service). HRS are non-covered services offered as a supplement to covered benefits under OHP’s Medicaid plan to improve care delivery and overall member wellbeing and community health. CCOs can choose to use multiple funding pathways to meet membership, provider network, and community needs.
Eligibility Requirements Per Oregon’s Prioritized List of Health Services
To be eligible for referral to a CDC-recognized National DPP provider, patients must meet the following requirements for OHP payment:
- Be at least 18 years old and
- Be overweight or obese (body mass index ≥25; ≥23 if Asian; BMI percentile ≥85th percentile for ≤19 years old) and
- Have no previous diagnosis of type 1 or type 2 diabetes and
- Not have end-stage renal disease and
- For members with a prediabetes or gestational diabetes diagnosis, one of the following is required: (Have a blood test result in the prediabetes range within the past year)
- Hemoglobin A1C: 5.7%–6.4% or
- Fasting plasma glucose: 100–125 mg/dL or
- Two-hour plasma glucose (after a 75-gram glucose load): 140–199 mg/dL, or
- Have a previous diagnosis of gestational diabetes
As referenced in Guideline Note 179 and Guideline Note 5 of Oregon’s Prioritized List of Health Services, participant eligibility for the National DPP lifestyle change program is dependent upon:
- Prediabetes diagnosis (ICD10 R73.03), or
- Diagnosis or past history of gestational diabetes (ICD-10 Z86.32), or
- Diagnosis of obesity or overweight (E66.01 –E66.9 (obesity) codes).
- For a prediabetes diagnosis, participants need to have a blood test result within the prediabetes range within the past year to be eligible for services.
- Participants who qualify for the National DPP through the CDC prediabetes risk test will also need to meet the Oregon Health Plan eligibility criteria as outlined in Guideline Note 179 listed in previous paragraph.
For more information on Oregon’s benefit, see Oregon’s Companion Guide. Member eligibility information starts on page 17.
Including the National DPP Lifestyle Change Program in Performance Improvement Projects (PIPs)
OHA contractually requires each CCO to address four quality improvement focus areas from a list of quality improvement focus areas provided in Oregon’s 1115 waiver. Three of these four projects may serve as a CCO’s Performance Improvement Projects (PIPs). CCOs are required to participate in the statewide PIP for the “integration of health” focus area and have the flexibility to determine their additional quality project focus areas. The National DPP lifestyle change program is specifically enumerated as an example intervention in the “Addressing population health issues” focus area. Specific language from the Special Terms and Conditions (STCs) of Oregon’s 1115 waiver is included below:
- “24 b. CCO quality and access measurement. CCOs will be accountable for metrics for quality and access as described in Section VII and Attachment E, including measures to track progress in the quality improvement focus areas, measures to track quality broadly, and measures to track access. Specific measures, timeframes, and CCO reporting requirements will be determined by the state in consultation with CMS.
- ii. Menu-set of CCO quality improvement focus areas. OHA will ensure that each CCO will commit to improving care in at least 4 of the following 7 focus areas, which have the significant potential for achieving the demonstration’s goals of improving the patient experience of care, improving population health, and reducing per capita Medicaid expenditure trend. Three of these four projects may serve as a CCO’s Performance Improvement Projects in accordance with 42 CFR 438.358 and 438.240. Attachment E provides further details on each of these focus areas. The state and CCOs may add to this menu of focus areas but should review Attachment E and provide a similar level of detail for anything not on the Demonstration Approval Period: January 12, 2017 through June 30, 2022 Page 25 of 287 list below. The state will update the Performance Improvement Projects in Attachment E within 90 days of the demonstration approval.
- Reducing preventable rehospitalizations.
- Addressing population health issues (such as diabetes, hypertension and asthma) within a specific geographic area by harnessing and coordinating a broad set of resources, including community workers, public health services, aligned federal and state programs, etc. …” Bolding added for emphasis.
- ii. Menu-set of CCO quality improvement focus areas. OHA will ensure that each CCO will commit to improving care in at least 4 of the following 7 focus areas, which have the significant potential for achieving the demonstration’s goals of improving the patient experience of care, improving population health, and reducing per capita Medicaid expenditure trend. Three of these four projects may serve as a CCO’s Performance Improvement Projects in accordance with 42 CFR 438.358 and 438.240. Attachment E provides further details on each of these focus areas. The state and CCOs may add to this menu of focus areas but should review Attachment E and provide a similar level of detail for anything not on the Demonstration Approval Period: January 12, 2017 through June 30, 2022 Page 25 of 287 list below. The state will update the Performance Improvement Projects in Attachment E within 90 days of the demonstration approval.
- “Attachment E: Menu Set of Quality Improvement in Focus Areas… Goal: Addressing population health issues… Example Interventions: Activities for improving the selected discrete health issue could be integrated with existing efforts at the community level through local public health, local health initiatives with community health centers. Specific intervention examples would be National Diabetes Prevention Programs, Million Hearts campaign, and case management program, including targeted outreach calls.” Bolding added for emphasis.
Vermont
Statewide Reform through an 1115 Waiver
In 2005, CMS approved Vermont’s 1115 waiver. The Vermont “Global Commitment to Health” Medicaid 1115 waiver uses a multi-disciplinary approach to promote basic principles of public health, public-private partnerships, and program flexibility. The most recent version of the waiver extends through 2021.
The waiver allows the state to invest in broader population health initiatives that benefit both Medicaid and non-Medicaid beneficiaries. These investments can be made if the state provides essential Medicaid benefits and keeps overall Medicaid expenditures below a pre-determined, baseline spending cap.
The state uses some of these investment funds to deliver self-management programs under the State of Vermont’s Blueprint for Health (Blueprint) initiative. This initiative provides grant funding to local communities to design and implement strategies for improving health and wellbeing. Through the Blueprint, the state is delivering six chronic disease prevention and self-management programs or “workshops,” including the National DPP lifestyle change program. Other programs include the Stanford Self-Management Programs (Chronic Disease, Pain, and Diabetes), tobacco cessation programs, and the Wellness Recovery Action Plan (WRAP).
The state delivers and pays for the National DPP lifestyle change program using Blueprint grant dollars, which come from 1115 waiver savings (measured from a pre-determined baseline). Due to the unique funding mechanisms and structure outlined in the 1115 waiver, the National DPP lifestyle change program is available and free to any person in Vermont who wants to participate.
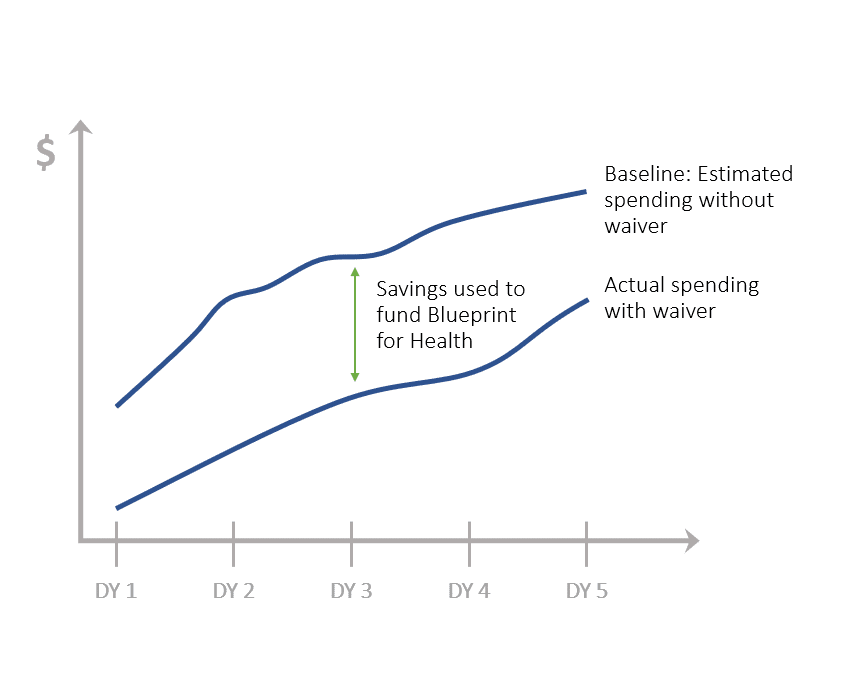
DY = Demonstration Year (year of operation under the 1115 waiver). For illustrative purposes only. Not reflective of actual savings achieved or dollars flowing to the State of Vermont’s Blueprint for Health.
Funding and support for the National DPP lifestyle change program in Vermont comes in two forms:
1. Infrastructure funding. Payments are provided through health service area* grants. These grants include at least $45,000 per year for self-management programs. The payments support program implementation costs and lifestyle coach stipends and are used to implement all state-sponsored chronic disease prevention and self-management programs. Each health service area is required to offer at least three continuous National DPP lifestyle change programs per year.
-
- The health service area grant recipients have relationships with their local providers that allows them to support providers in utilizing electronic health records to develop patient panels from which to recruit eligible program members.
*(Blueprint health service areas are state-defined geographical boundaries that dictate the coverage areas of Blueprint Community Health Teams. These teams are responsible for helping to determine and meet the needs of the local population.)
2. Technical assistance capacity payments. These payments are made to an administrative organization that works in partnership with the Blueprint and Department of Health to provide program technical assistance on a statewide basis, including: (1) leadership, lifestyle coach, and curriculum training for the National DPP lifestyle change program; (2) quality improvement activities; (3) marketing, recruitment, and retention support; and (4) data aggregation, tracking, and submission. Technical assistance was managed by the YMCA of Greater Burlington through the first three quarters of 2017. The University of Vermont Medical Center took over program technical assistance beginning October 1, 2017 (Blueprint for Health In 2017 Annual Report).
The State of Vermont (managed through the Blueprint for Health, Department of Vermont Health Access) serves as the CDC-recognized organization, meaning it collects, aggregates, and submits data to the CDC from each of the National DPP lifestyle change programs operated by the 14 health service areas. The state is in the process of receiving full CDC-recognition.
Benefits to this approach include:
- As a state-based organization, the Blueprint can ask its community partners (e.g., Area Agencies on Aging, libraries, medical providers, etc.) to help recruit people to the program.
- The Blueprint works with employers across the state, including the Vermont state employee plan, to promote participation. For example, the Blueprint worked with an employer to provide employees with release time to participate in the National DPP lifestyle change program.
Ensuring Covered Services are Included in Medicaid Managed Care
Following the decision to cover the National DPP lifestyle change program and the approval of a section 1115 demonstration waiver, states should also ensure the program is included in any relevant MCO regulations that outline required covered services in managed care. For example, Maryland has a Code of Maryland Regulations that outlines all required Maryland HealthChoice (Maryland’s managed care program) benefits. When the National DPP lifestyle change program was added as a covered benefit in Maryland Medicaid via a section 1115 demonstration waiver, these regulations were amended to include the program. Other states may not specify this level of program detail through regulation, but may require that MCOs cover “all state plan services” or give their Medicaid agencies the discretion to determine what services to include in the MCO contracts and which ones to carve out.
States should seek to understand their unique regulatory environment to determine what steps, if any, are necessary to ensure coverage of the National DPP lifestyle change program in managed care once it becomes an approved benefit through an 1115 waiver.
1115 Waiver Considerations
12-Month Continuous Eligibility 1115 Waivers
One challenge to covering the National DPP lifestyle change program in Medicaid is the high rate of churn among Medicaid beneficiaries, particularly those closest to the eligibility income limit. Churn is defined as the repeated movement of families and individuals on and off benefit coverage over time as their income falls below and increases above the eligibility income limit.
Medicaid churn rates vary substantially by state and are dependent on the qualifying level of income for Medicaid eligibility. Some states report churn rates as low as 2%, while other research has found rates to be as high as 40%.
Given the National DPP lifestyle change program is a year-long program, it may be difficult to manage the participating populations if there is a high rate of churn even if strong recruitment and retention processes are implemented.
To mitigate this issue, one option states may want to consider is seeking an 1115 waiver that would allow for 12-month continuous eligibility for its adult Medicaid population. While the Affordable Care Act (ACA) restricts states from requiring Medicaid beneficiaries to renew coverage more than once every 12 months, beneficiaries are still required to report changes in income that may cause them to lose coverage. States with approved 12-month continuous eligibility waivers are able to provide a full year of coverage regardless of changes in income or household size.
As of January 2019, a Kaiser Family Foundation report on Medicaid and CHIP shows New York and Montana provide 12-month continuous eligibility to parents and other adults under section 1115 waiver authority. Utah’s 1115 waiver also provides 12-month continuous eligibility for adults age 19-24 without dependent children, with effective incomes of up to 5% of the federal poverty level, and who meet specified criteria in one of three subgroups: (1)individuals experiencing chronic homelessness, (2) individuals involved in the justice system and needing substance use or mental health treatment, or (3)individuals needing substance abuse or mental health treatment.
Budget Neutrality
Demonstrations must also be “budget neutral” to the federal government, meaning that over the course of the demonstration, federal Medicaid expenditures will not be more than what federal spending would have been without the waiver. CMS’s determination that a demonstration is expected to be budget neutral is based on forecasts, using reasonable projections of future spending and enrollment trends. CMS monitors budget neutrality throughout the demonstration period, and also performs a formal adjudication at the end of the demonstration period to determine whether the state’s actual spending has remained within the specified limit. In 2018, CMS issued a letter to State Medicaid Directors detailing CMS’s approach for calculating budget neutrality.
In calculating the cost savings from implementing the National DPP lifestyle change program, states will need to estimate how many Medicaid enrollees have prediabetes as well as the type 2 diabetes-related costs that could be averted by implementing the National DPP lifestyle change program (see the Cost and Value page of the Coverage Toolkit for more information on estimating the cost-effectiveness or cost-savings of the program, as well as the Screening and Identification page for more information on identifying Medicaid enrollees eligible for the program).
These estimates are then included in the budget neutrality calculations to show the difference between expenditures “with waiver” v. “without waiver.” Budget neutrality must be achieved within a five-year period if pursuing an 1115 waiver.
An additional consideration exists for those states that have implemented, or plan to implement waivers to reform the broader Medicaid delivery system and promote population health. The National DPP lifestyle change program would align well with an overarching strategy for reform and enhance prevention efforts. In this case, the National DPP lifestyle change program can be accommodated into the budget neutrality calculations for the full waiver, meaning that savings generated from a different program could be used to offset any costs incurred by the National DPP lifestyle change program within the first five years of the demonstration.
Budget neutrality calculations are specific to the state, the waiver application, and the number of Medicaid reforms being sought. Most state actuaries have experience developing budget neutrality calculations and CMS is available to provide technical assistance to individual states to identify elements needed to demonstrate budget neutrality. In 2018, CMS launched a new monitoring tool, a standardized budget neutrality reporting form, that consolidates financial data for each demonstration into a unified report. States upload the tool into the Performance Metrics Database & Analytics system as they do for their other monitoring and evaluation reports.
Timeline
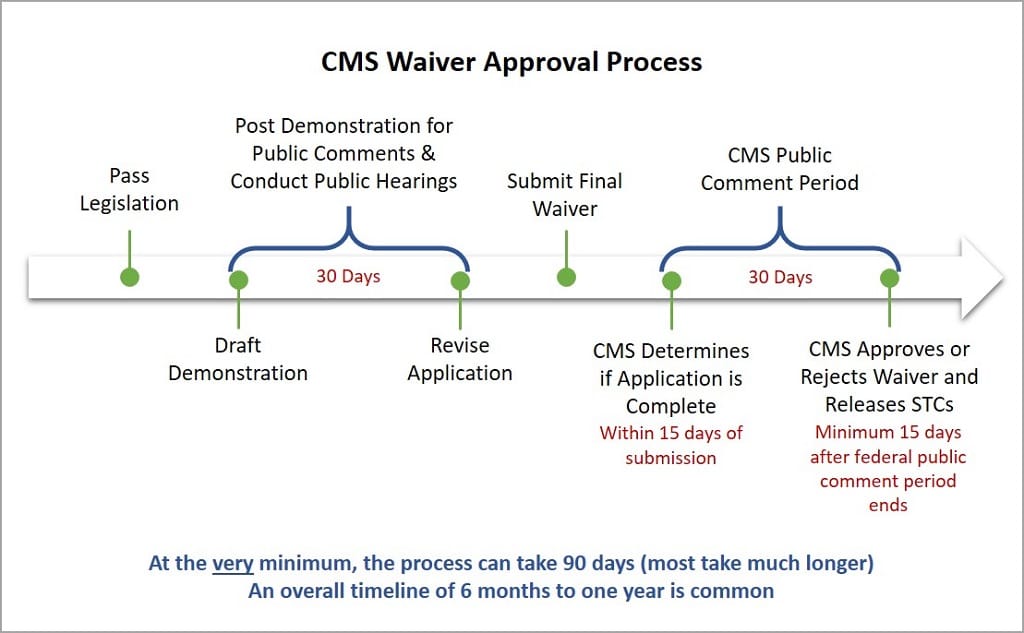
Generally, 1115 waivers are approved for an initial five-year period. The waiver can be renewed for an additional three to five years, depending on the populations served, and there is no limit on the number of times the waiver can be renewed. States commonly request and receive extension approvals. However, the waiver process can be burdensome on a state and there is no guarantee of reauthorization.
About Delivery System Reform Incentive Payment (DSRIP) 1115 Demonstration Waivers
In Delivery System Reform Incentive Payment (DSRIP) 1115 waivers, participating providers or payers develop project plans with specific goals for delivery and payment system improvement. The project plans outline plans for program implementation and delivery and are approved by the state and CMS.
The National DPP lifestyle change program was included in the New York and Texas DSRIP 1115 demonstration waivers. The goal of DSRIP 1115 waivers in many states has been to reform the Medicaid program’s delivery and payment system to better focus on improving population health, care quality, patient experience, and reducing costs. DSRIP programs offer the potential of driving value and improved health outcomes in Medicaid by linking payment to the achievement of specific milestones.
The 2015 Medicaid and CHIP Payment and Access Commission (MACPAC) Report provided an in-depth analysis of the DSRIP waiver approach. The report expressed optimism towards DSRIP waivers and their ability to “fundamentally change Medicaid’s role from financing medical care to driving system change towards value and improved health outcomes.” However, the report also discussed challenges states report with implementing the waivers, including finding a sustainable source of non-federal share funding and the substantial resources needed to implement delivery changes.
It is important to note that programs and system reforms included in these project plans are not always reimbursed through payments for specific services received by Medicaid beneficiaries. Instead, participating providers and payers have received financial support for program implementation and delivery from a pool of state and matching federal dollars established by CMS. Continued receipt of dollars is generally dependent on meeting pre-determined measures and milestones.
The caution with using a DSRIP 1115 waiver approach is that the demonstration is time-limited, and, in the past, CMS has expressed disinclination to renew these types of programs without some additional guarantee of sustainability. Additionally, the amount of funding and the approval of new DSRIP waivers may be impacted by the current administration’s priorities.
To continue covering the services provided by National DPP lifestyle change programs once the DSRIP 1115 demonstration has ended, a state would need to find an alternative method to draw down federal Medicaid matching funds, or participating providers and payers would need to find alternative financing for the program.
DSRIP 1115 Demonstration Waiver State Examples
New York
Attaining Federal Medicaid Matching Funds through a DSRIP 1115 Waiver
In 2014, New York State (NYS) initially began coving the National DPP lifestyle change program in Medicaid by including the program into the state’s DSRIP 1115 waiver. The waiver required participating providers to include at least five but no more than 11 projects chosen from the three different domains, as required by the state Medicaid agency. The National DPP lifestyle change program was an optional project for providers to pursue under Domain 3 (clinical improvement projects). Language from the DSRIP Project Toolkit is as follows:
“Project Title: Implementation of evidence-based strategies in the community to address chronic disease—primary and secondary prevention projects. (adult only)
Objective: These projects are focused on improving patient self-efficacy and confidence in self-management and engagement of the at-risk population in primary and secondary disease prevention strategies.
Rationale and Relationship to Other Projects: While Project 3.c.i is focused on practice improvement focused on diabetes care, this project focuses on developing community resources that will work collaboratively with community practitioners to assist patients with primary and secondary preventive strategies to reduce their risk factors for diabetes and ameliorate the long-term consequences of diabetes and other co-occurring chronic diseases.”
For more information, see NYS’s DSRIP Project Toolkit.
Attaining Federal Medicaid Matching Funds through a SPA
On April 12, 2019, the NYS legislature amended its social services law to include the National DPP lifestyle change program within the definition of “standard coverage” for medical assistance for needy persons. Amending the social services law also authorized CDC-recognized organizations to enroll in NYS Medicaid and receive Medicaid reimbursement. This substantial change to NYS Social Services Law allowed for community based organizations to be able to engage Medicaid (both FFS and Medicaid managed care plans) and enroll as the Medicaid provider of record for the first time and be directly reimbursed for National DPP services rendered to Medicaid members.
To secure federal Medicaid matching funds for the program NYS Medicaid submitted a SPA to CMS on June 28, 2019, which was expeditiously approved by CMS on September 4, 2019. Additional details about NYS’s coverage of the National DPP lifestyle change program can be found on the New York State Story of Medicaid Coverage and the Attaining Coverage through a Medicaid State Plan pages of the Coverage Toolkit.
Texas
Attaining Federal Medicaid Matching Funds through a DSRIP 1115 Waiver
In 2011, CMS approved Texas’ DSRIP 1115 waiver. The waiver includes two funding streams, one for uncompensated care delivered to patients without insurance and another for the DSRIP program that provides innovative health care initiatives to Medicaid beneficiaries. In Texas, regions have more flexibility in proposing these innovative, DSRIP-funded projects rather than selecting from a predetermined menu. For example, San Antonio’s public health department in Region 6 launched the Community Diabetes Project in 2013, which implemented the National DPP lifestyle change program by establishing an agreement between the City of San Antonio Metropolitan Health District and the national YMCA Diabetes Prevention Program to offer the program to the San Antonio community.
San Antonio sought over three million dollars through Texas’ DSRIP 1115 waiver over a five-year period to implement this program. In addition to those on Medicaid, the program is provided to uninsured and underinsured individuals.
In December 2017, CMS approved a five-year renewal of Texas’ DSRIP 1115 waiver; however, the waiver renewal decreased federal matching funds for the state’s DSRIP program between year one and year four, eliminating federal funding for DSRIP in the fifth year. Texas is in the process of making transition plans on which areas to sustain and how to replace the lost funding. There is some uncertainty about how the funding will eventually be structured as the state’s DSRIP Transition Plan does not require Texas to sustain specific DSRIP projects or core activities nor does it require Texas to sustain a certain level of funding to support ongoing transformation efforts. However, while not explicitly discussing the National DPP lifestyle change program, the public health section of the DSRIP Transition Plan includes a program proposal to “continue to support valuable local public health initiatives, including traditional and enhanced services, such as…chronic disease such as diabetes, crisis care, and/or health promotion activities to prevent severe and/or disabling preventable conditions.”









