Medicaid Coverage for the National DPP Demonstration Project

The Challenge
“You want to pull in communities of color or other historically marginalized communities…Being able to include them at the beginning of the process, and also be aware of the capacity that’s needed, and the capacity that is present. And how can the larger organizations – the larger health care organizations, clinics, and other institutions – actually support … the community-based organizations, and utilize the skill and knowledge that’s present in those places, as well as the community to be able to support the curriculum.”
– Oregon Coordinated Care Organization (CCO)
Launching Medicaid coverage for a year-long lifestyle change program can be a complex and multi-faceted process that involves partners at the federal, state, and community levels. In recent years, a growing number of Medicaid agencies have been exploring options for establishing, operationalizing, and sustaining coverage of the National DPP lifestyle change program within their state. Other state partners, including State Health Departments, managed care organizations (MCOs), community-based organizations, and health care organizations, also play a vital role in meeting this need.
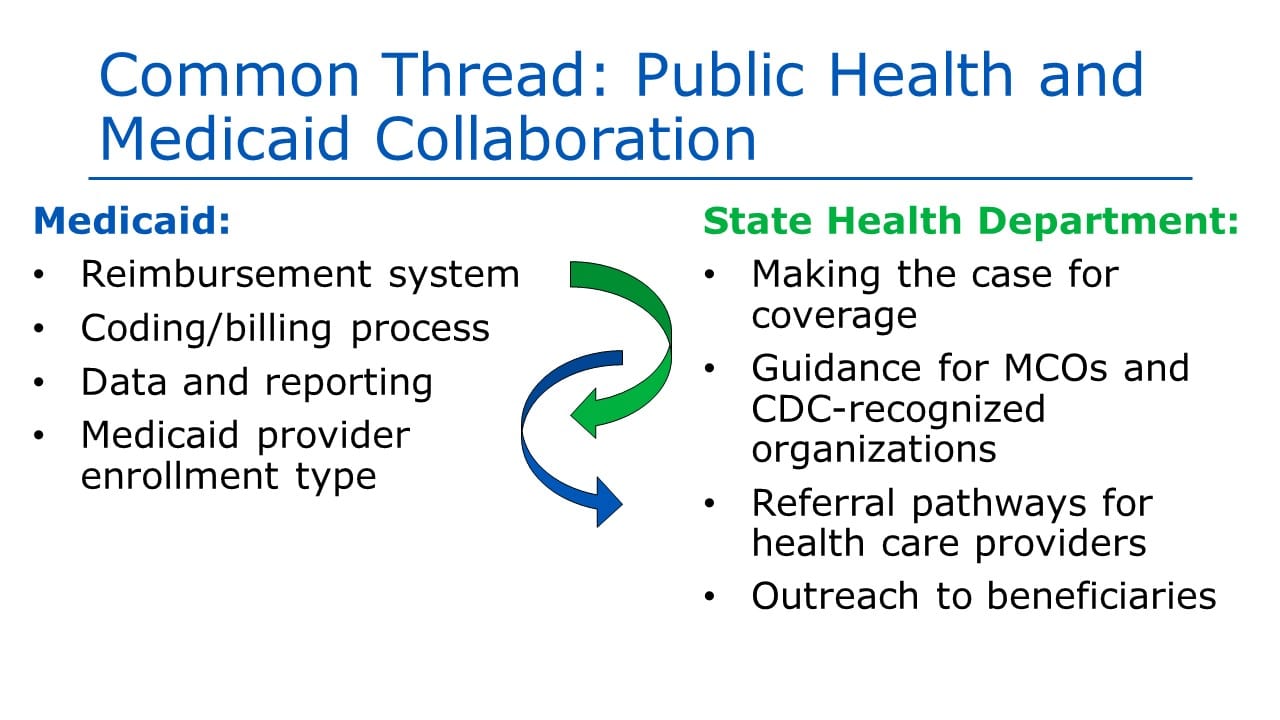
Communication and collaboration between Medicaid agencies and State Health Departments is especially important in this work. Until recently, and in many states, these two agencies did not traditionally collaborate with one another; yet for a shared goal such as Medicaid coverage, they both can play very important roles.
As shown in the diagram below, Medicaid may:
- Affect policy decisions
- Set up reimbursement systems
- Establish coding and billing processes, and
- Determine Medicaid provider enrollment types.
State Health Departments may take on the roles of:
- Making the case for coverage of the program, both to the Medicaid agency and also to MCOs and other state partners
- Translating details of the Medicaid policy and providing guidance to MCOs and CDC-recognized organizations
- Establishing and operationalizing referral pathways for health care providers, and
- Conducting outreach to beneficiaries once a benefit is finalized.
“… [the Demonstration] has worked really well to get all of us together at the table for our [National DPP] collaboratives where we’re all putting aside our individual roles and coming together across the CCOs and with the state and the county and the [National DPP] suppliers to think big picture and unpack together some of the bigger challenges.”
– Oregon CCO
Content last updated: June 26, 2020













