Oregon Medicaid Demonstration Project
Oregon’s Medicaid program, known as the Oregon Health Plan (OHP), is implemented through the Oregon Health Authority’s (OHA) Health Systems Division. To ensure better health and coverage for Medicaid recipients, Oregon created coordinated care organizations (CCOs) in 2014. CCOs, which are similar to accountable care organizations, are collaborations among communities, health care providers, health plans, and hospitals, intended to integrate physical, behavioral, and oral health care under global budgets that incentivize value-based service delivery and patient outcomes for OHP members. CCOs are focused on prevention and helping people manage chronic conditions, such as diabetes, and address chronic disease risk factors. As of December 2018, 571,406 adult Medicaid beneficiaries were OHP members and enrolled in either fee-for-service or one of 16 CCOs.

Oregon implemented the Medicaid Coverage for the National Diabetes Prevention Program (National DPP) Demonstration Project through OHA’s Health Systems Division and Public Health Division. The structure of the Demonstration in Oregon brought together the Health Systems Division’s focus on preventive services and the Public Health Division’s community collaborative infrastructure, the Sustainable Relationships for Community Health (SRCH) model. The SRCH model, used by OHA to advance local health system interventions and promote community‐clinical linkages at the county level, is organized around local public health, CCOs, tribes, clinics, and community-based organizations.
Three of the state’s 16 CCOs (as of 2016) participated the Demonstration to deliver the National DPP lifestyle change program to their Medicaid recipients at risk for type 2 diabetes. The CCOs included FamilyCare Health (FamilyCare), Health Share of Oregon (Health Share), and Trillium Community Health Plan (Trillium). In January 2018, FamilyCare closed its Medicaid managed care plan, and all beneficiaries were transferred to Health Share or other CCOs. Beneficiaries who had been part of the Demonstration through FamilyCare that were transferred to Health Share were able to continue participation in the National DPP lifestyle change program through the same CDC-recognized organizations.
Figure 1. Organization of Oregon’s Medicaid Demonstration Project (Year 2)
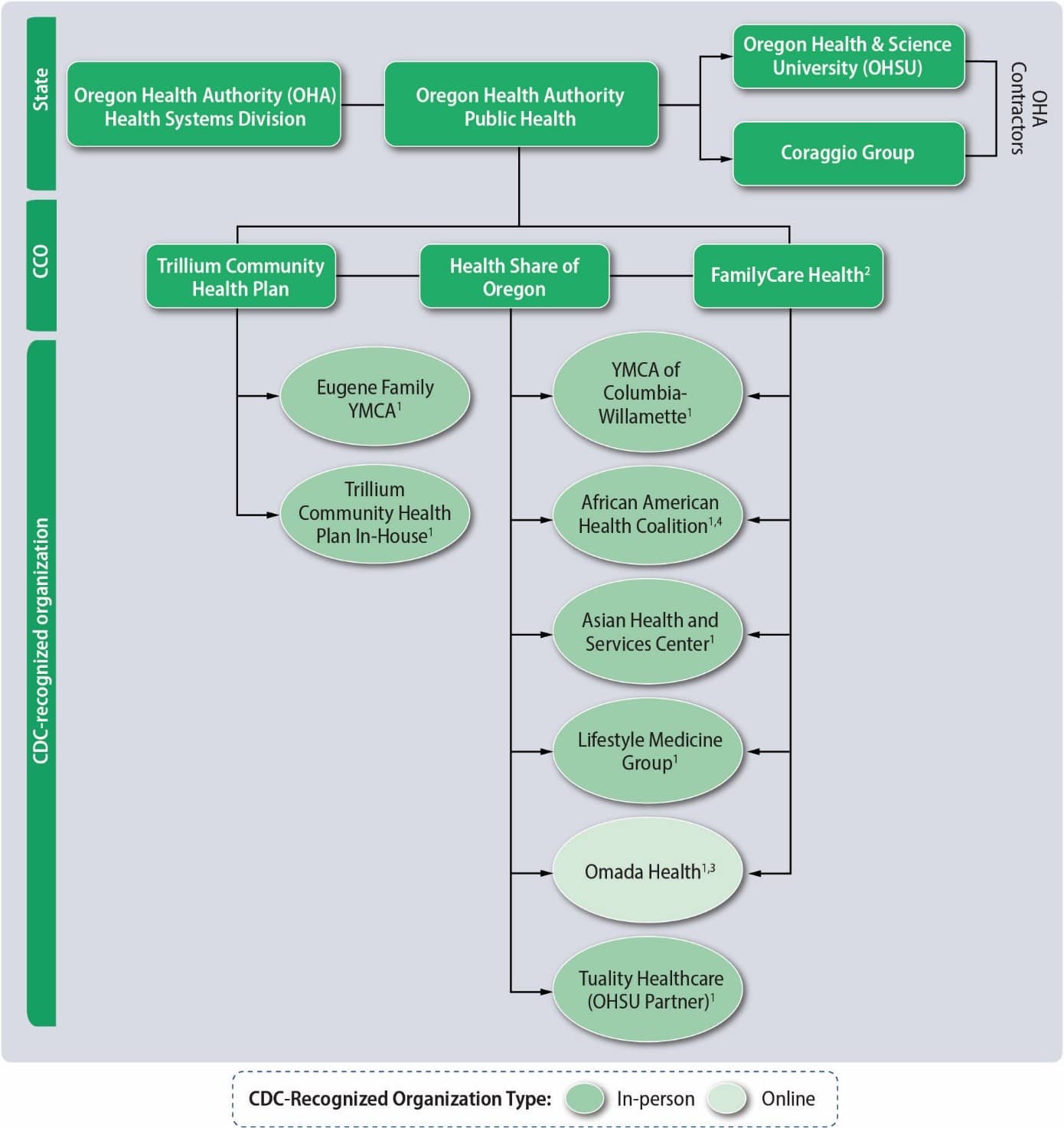
2. Family Care discontinued its Medicaid-National DPP on February 1, 2018.
3. Omada only has one organizational code, even though it works with multiple MCOs and CCOs across states.
4. African American Health Coalition discontinued its portion of the Demonstration; the lifestyle change program participants from this organization completed the classes at the Miracles Club of Portland.
CCOs’ global budgets enable them to use flexible funds and administrative dollars to provide funding to the community to implement evidence-based programing. For the Demonstration, they distributed the grant dollars to community partners to deliver the National DPP lifestyle change program in their service areas. FamilyCare and Health Share used the same CDC-recognized organizations, including the Asian Health Services Center, the African American Health Coalition, the YMCA of Columbia-Willamette, and Lifestyle Medicine Group. In March 2018, the African American Health Coalition closed its doors. CCO members from Health Share and FamilyCare who participated in the Demonstration were transitioned to the Miracles Club, a nonprofit community-based organization serving the African American community in the Portland Metropolitan area. In addition, Oregon Health & Science University’s (OHSU’s) Harold Schnitzer Diabetes Health Center provided a Spanish-language class in Clackamas County for Health Share and FamilyCare members. Health Share and FamilyCare also offered online delivery of the National DPP lifestyle change program through Omada. Trillium Community Health Plan delivered the National DPP lifestyle change program to members in Lane County by offering the program in-house (i.e., Trillium became a CDC-recognized organization) and through the Eugene Family YMCA. In addition to providing a Spanish-language National DPP lifestyle change program (Tuality Healthcare) to Health Share, the Harold Schnitzer Diabetes Health Center at OHSU provided training and technical assistance to CDC-recognized organizations and assisted Health Share with recruitment of eligible Medicaid beneficiaries. The Coraggio Group, a Portland management consulting group, provided coaching and technical assistance to state agencies, CCOs, and other local SRCH partners involved in the Demonstration. The Coraggio Group played an integral role in the annual SRCH institutes, which brought together local SRCH partners involved in the Demonstration as well as other CCOs engaged in related work in chronic disease to develop strategic plans, integrate systems, and share lessons learned.
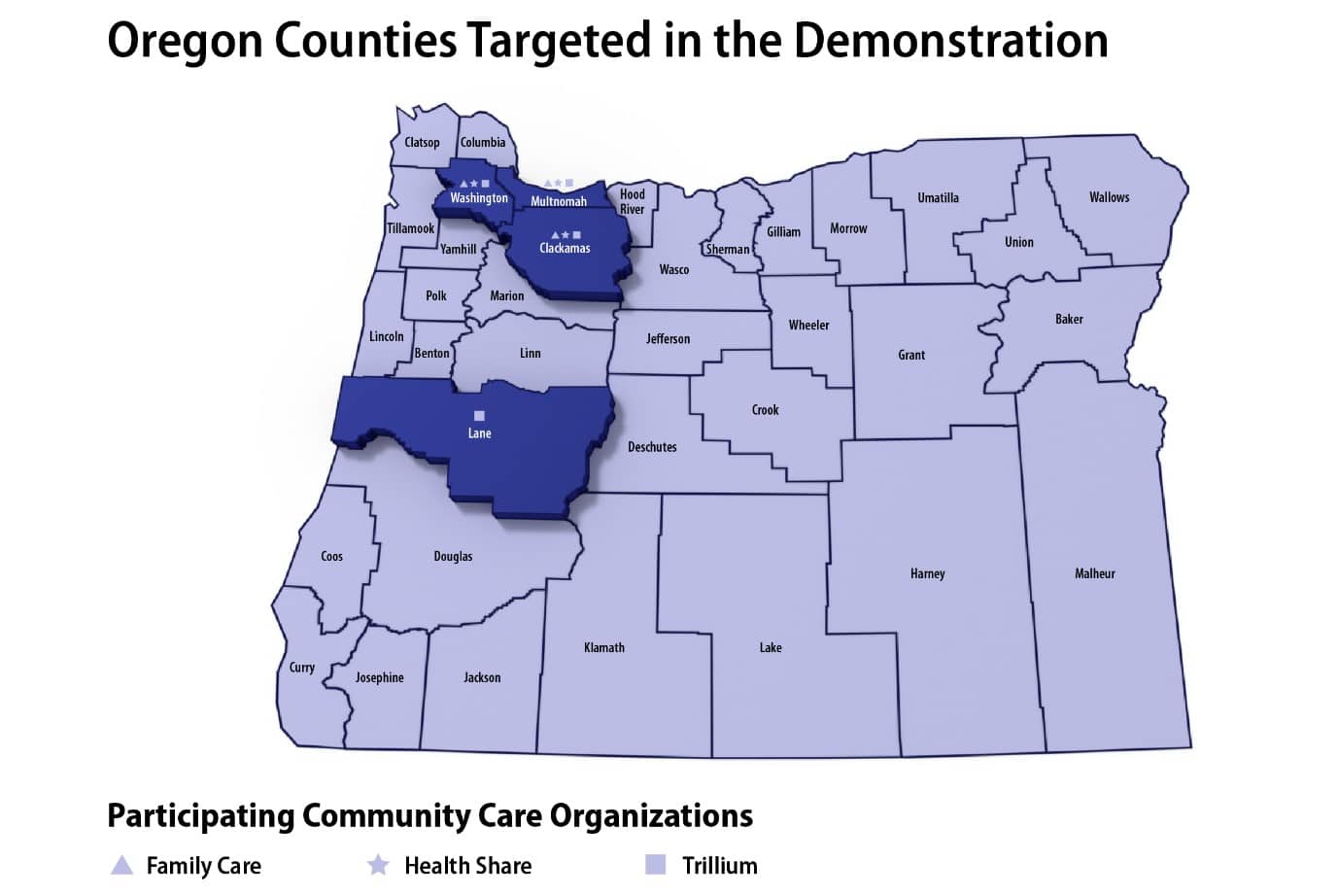
As of June 2016, FamilyCare provided OHP coverage in four counties: Clackamas, Multnomah, Washington, and parts of Marion. FamilyCare had approximately 130,000 OHP recipients in these counties. Health Share had a similar geographic coverage area that included Clackamas, Multnomah, and Washington Counties, with approximately 236,000 OHP members. Trillium covered Lane County, with approximately 100,000 OHP members.
Figure 2. Oregon Counties Targeted in the Demonstration
To learn more about outcomes from the Demonstration, please visit the Evaluation page. Oregon created guides for their CCOs to successfully implement the National DPP lifestyle change program, please find those here.
Sustainability
OHP Medicaid benefits are based on a “Prioritized List of Health Services.” This list ranks both condition and treatment by priority. Oversight of the Prioritized List is led by the Health Evidence Review Commission (HERC), the roles and responsibilities of which were established in Oregon’s section 1115 demonstration waiver in 1994. The HERC is charged with reviewing the Prioritized List every two years and amending it as required. Once amended, the Oregon Legislature decides a funding threshold for coverage based on the state’s budget. In May of 2018, a recommendation was made to the HERC to add the National DPP lifestyle change program to the Prioritized List of Health Services. In August of 2018, the recommendation was approved. Currently, the National DPP lifestyle change program is included on the Prioritized List of Health Services under “Prevention Services with Evidence of Effectiveness.” The National DPP lifestyle change program is within the threshold for funding as approved by the Oregon legislature, and it became a covered Medicaid benefit in Oregon effective January 2019.
The HERC decision means the National DPP lifestyle change program is a covered medical benefit for Oregon’s fee-for-service (FFS) and CCO OHP members. For more information on reimbursement rates, please visit the Oregon reimbursement models on the Reimbursement Models for Medicaid Agencies and MCOs page.
OHA engages multiple stakeholders to support the implementation of the National DPP Medicaid benefit. OHA has been outreaching to health care providers to improve awareness and increase referrals. Efforts are additionally underway to support bi-directional referral systems between health care providers and CDC-recognized organizations that deliver the National DPP lifestyle change program. More information on bi-directional referral systems can be found on the Recruitment and Referrals page. In May 2022, OHA contracted with the Corragio Group to produce a case study about the benefit titled, The Current State of the National Diabetes Prevention Program Oregon Health Plan Benefit. This three-page case study presents the challenges that CCOs have faced in implementing the National DPP lifestyle change program in Oregon, and it offers potential solutions to those challenges that OHA continues to champion throughout the state. To learn more about Oregon’s National DPP lifestyle change program benefit please visit the Oregon Health Authority: National Diabetes Prevention Program webpage.
To learn more about Oregon’s benefit, see Oregon’s 2023 Companion Guide for Coordinated Care Organizations and Oregon Health System Partners Serving Oregon Health Plan Members. Additionally, please watch the June 15, 2023 NACDD webinar, Maryland and Oregon: Journey from Pilot to Performance, minute 30 through 51 in the recording, and please see the summary resource of the presentation.









