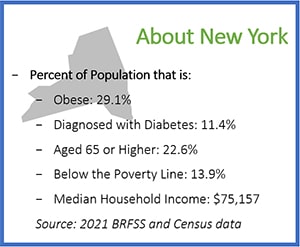
Medicaid → State Stories of Medicaid Coverage → New York
New York’s State Story of Medicaid Coverage
Overview
On April 12, 2019, the New York State (NYS) legislature amended its social services law to include the National Diabetes Prevention Program (National DPP) lifestyle change program within the definition of “standard coverage” for medical assistance for needy persons. Amending the social services law also authorized CDC-recognized organizations to enroll in NYS Medicaid and receive Medicaid reimbursement. This substantial change to NYS Social Services Law allowed for Community Based Organizations (CBOs) to be able to engage Medicaid (both FFS and Medicaid Managed Care (MMC) plans) and enroll as the Medicaid provider of record for the first time and be directly reimbursed for National DPP services rendered to Medicaid members.
To secure Federal Financial Participation (FFP) (federal Medicaid matching funds) for the program NYS Medicaid submitted a Medicaid State Plan Amendment (SPA) to the Centers for Medicare and Medicaid Services (CMS) on June 28, 2019, which was expeditiously approved by CMS on September 4, 2019.
The NYS legislature’s social services amendment allowed for the creation of a new provider type that permits CDC-recognized organizations to enroll as Medicaid providers. NYS Medicaid’s provider enrollment for CDC-recognized organizations became available in November 2019. NYS Medicaid reimbursement for the National DPP program became available as of February 1, 2020 for both Medicaid Fee-For-Service, and MMC members.
Establishing Coverage
- 2014: NYS included evidence-based diabetes prevention activities in its 1115 Delivery System Reform Incentive Payment (DSRIP) waiver. The waiver’s DSRIP Project Toolkit provided a list of clinical improvement activities from which participating providers could choose, including becoming or partnering with a CDC-recognized organization delivering the National DPP lifestyle change program.
- 2015: The NYS Comptroller’s Office of Budget and Policy Analysis published the NYS Comptroller Diabetes Report. The report, intended to provide key measures of the diabetes burden in NYS, found that the NYS Medicaid diabetes-related expenditures increased by 31% between State Fiscal Year (SFY) 2009-2014. The report also found that diabetes-related costs for 460,000 NYS Medicaid members was over $1.2 billion in 2014.
- 2017: NYS Medicaid’s Evidence Based Benefit Review Advisory Committee (EBBRAC), a committee charged with making recommendations regarding coverage of health technology or service for purposes of the medical assistance program took up the subject of the National DPP lifestyle change program at their December 2017 meeting. EBBRAC, in collaboration with the NYS Department of Health (DOH), commissioned the Oregon Health & Science University (OHSU) Center for evidence-based policy to produce a 58-page meta-analysis about diabetes prevention programs in Medicaid. After review and discussion of the analysis, the EBBRAC voted unanimously to recommend Medicaid coverage of the National DPP.
- 2019: On April 12, 2019, NYS passed legislation that allowed for Medicaid’s coverage of the National DPP lifestyle change program within the definition of “standard coverage” for medical assistance for needy persons. The amendment also allowed for the creation of a new provider type, which allows CDC-recognized organizations to enroll as Medicaid providers to deliver the program. The legislation amended the State’s Social Services law and included the following language:
- “PART C Section 1. Subdivision 2 of section 365-a of the social services law is amended by adding a new paragraph (ff) to read as follows: (ff) evidence-based prevention and support services recognized by the federal Centers for Disease Control (CDC), provided by a community-based organization, and designed to prevent individuals at risk of developing diabetes from developing Type 2 diabetes…”
- To learn more, see the NYS example on the Role of the State Legislature in Medicaid Coverage page of the Coverage Toolkit.
- NYS Medicaid submitted a SPA to CMS on June 28, 2019, which was approved on September 4, 2019. Prior to submitting the SPA, the NYS DOH published a Federal Public Notice (FPN) to notify the public of the modification of the Medicaid State Plan to include the National DPP lifestyle change program, and the public was invited to review and comment on the proposed SPA. A copy of the SPA was made available for public review on the Department’s website. The NYS DOH reviewed the feedback that was received from the publication and engaged stakeholders to address their thoughts and/or concerns relative to the development and implementation of the NYS Medicaid program´s coverage of the National DPP lifestyle change program.
- NYS Medicaid’s provider enrollment for CDC-recognized organizations became available in November 2019.
- 2020: NYS began reimbursing for National DPP lifestyle change program for dates of service on or after February 1, 2020.
Implementing Coverage
Benefit Breakdown
Below is an overview of New York State’s Medicaid benefit:
| Delivery Methods | The National DPP lifestyle change program may only be delivered to Medicaid members through in-person delivery. |
| Participant Referral Requirements | A member referral is required for a member to be able to access NYS Medicaid National DPP services. The member’s referral to participate in the National DPP lifestyle change program must be written by a physician, physician assistant (PA), nurse practitioner, or midwife. |
| Lifestyle Coaches | A lifestyle coach may be a physician, non-physician practitioner, or an unlicensed person who has received formal training on a CDC-approved curriculum per requirements specified in the CDC’s Diabetes Prevention Recognition Program (DPRP) Standards and guidelines. Lifestyle coaches are required to obtain and maintain their own National Provider Identification (NPI). |
| Medicaid Enrolled Provider Eligibility | Only organizations that have achieved CDC recognition can be enrolled in Medicaid to bill for providing the National DPP lifestyle change program to Medicaid members. |
| Accepted CDC Recognition Levels | NYS Medicaid recognizes all three CDC-recognition levels (Pending, Preliminary, and Full) and will enroll any organization or individual that has achieved any of these recognition levels as a Medicaid National DPP service provider. |
| Provider Enrollment | In-person CDC-recognized organizations can enroll with Medicaid through NYS’s Electronic Medicaid of New York (eMedNY) system. Medicaid enrolled service providers are eligible to receive reimbursement for National DPP services rendered to Medicaid members. |
| Program Duration | The NYS Medicaid National DPP lifestyle change program follows the established CDC evidence-based program approach of a 12-month program. |
| Program Repeatability | The NYS Medicaid National DPP does not limit program services to once per lifetime. |
| Medicaid Data Submission Requirements | NYS Medicaid does not have any data submission requirements to enroll or participate in the program as a National DPP service provider. |
| Reimbursement, Coding, and Billing | Pursuant to New York’s SPA, the Medicaid FFS rate for National DPP lifestyle change program is 80 percent of the max 2019 two-year Medicare National DPP lifestyle change program rate, which is $689. This equates to a maximum reimbursement of $551 per member over 22 sessions. However, NYS has rounded each session payment up to the nearest dollar, resulting in a total reimbursement amount of $554 per member. The $554 is broken down as follows:
Additional information can be found in the New York State Medicaid DPP FFS Policy and Billing Guidelines. |
Program Features Unique to New York State
Communication and Engagement
NYS has proactively communicated with CDC-recognized organizations regarding how to enroll and bill as a Medicaid provider of the National DPP lifestyle change program. Engaging and communicating with the provider community can increase participant enrollment and retention in the program.
- In developing program policies and fee schedules, NYS Medicaid staff participated in meetings with some long-standing CDC-recognized organization partners to learn about their experiences and identify potential access barriers within the program. This type of open communication with CDC-recognized organizations in NYS helped create a responsive program framework.
- The NYS Medicaid program in collaboration with the NYS DOH Office of Public Health’s Bureau of Community Chronic Disease Prevention provided training and resources relative to Medicaid’s implementation and coverage of the National DPP benefit via a statewide kick-off webinar that was held on November 13, 2019. The webinar provided an overview of the new Medicaid National DPP lifestyle change program structure and covered topics such as: Medicaid National DPP program structure, Medicaid FFS member eligibility requirements, provider enrollment pathways, program reimbursement structure and amounts, and various resources.
- In 2020-2021, the NYS DOH intends to conduct additional National DPP collaborative learning trainings. The goals of these trainings are:
- To increase providers’ knowledge and awareness of the Medicaid program’s coverage of the National DPP lifestyle change program.
- To educate current and potential Medicaid National DPP lifestyle change program delivery organizations about becoming a NYS Medicaid service provider.
- To educate Medicaid enrolled National DPP service providers about contracting with Managed Care Organizations (MCOs); and
- To explore ways to expand the Medicaid National DPP network capacity and discuss collaboration opportunities.
Lessons Learned
NYS received SPA approval from CMS relatively quickly. The state submitted the SPA on June 28, 2019 and CMS approved it on September 4, 2019. Pre-SPA submission calls with NYS’s regional CMS representatives may have expedited NYS’s SPA approval.
Additional Resources
- NYS Medicaid Approved SPA – September 4, 2019
- NYS Medicaid National DPP Provider Enrollment page
- NYS Medicaid Redesign Team (MRT) – Contains additional information pertaining to Medicaid’s coverage of the National DPP lifestyle change program
- NYS Medicaid National DPP FFS Policy and Billing Guidelines
- eMedNY LISTSERV – Providers can sign up for the NYS Medicaid National DPP Listserv, which provides information relative to Medicaid’s coverage and reimbursement for offering the National DPP lifestyle change program to Medicaid FFS and MMC members
- Questions related to NYS Medicaid National DPP should be directed to NDPP@health.ny.gov









