Medicaid → Medicaid Coverage → Medicaid Coverage Map
Medicaid Coverage Landscape: Map and Visualizations
This page describes the states that have gained Medicaid coverage for the National DPP lifestyle change program. The managers of this website make every attempt to keep this information up to date. However, information is provided with the understanding that it is not guaranteed to be correct or complete and conclusions drawn from this information are the responsibility of the user. This page is updated quarterly in January, April, July, and October. If you have information or coverage updates for any payers, please let us know by filling out the Add or Update a Payer or Employer Form at the bottom of this page. This page is organized into five sections:
- State Medicaid Coverage
- State Medicaid Coverage Map
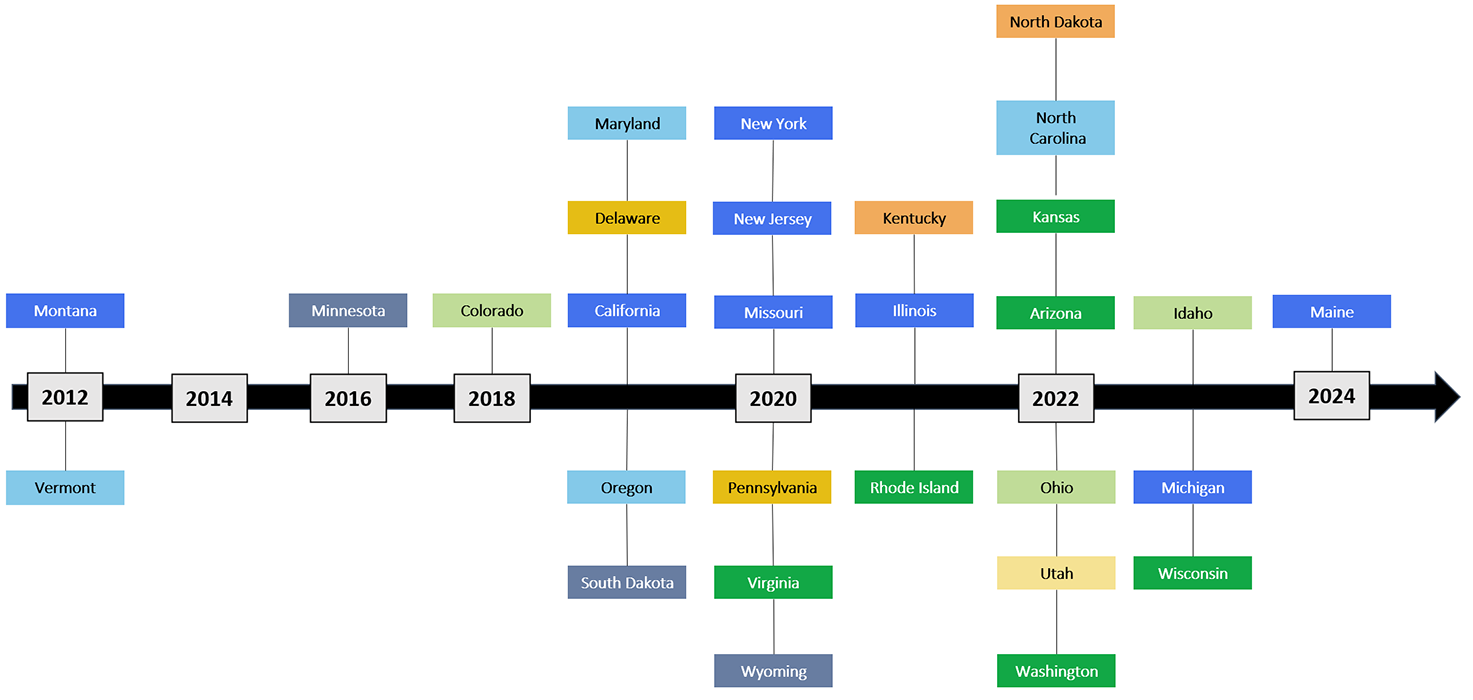
- Medicaid Coverage Timeline: State Effective Dates
- State Medicaid Coverage Filterable Table
- Add or Update a Payer or Employer
State Medicaid Coverage
Since 2012, 29 states have achieved varying levels of Medicaid coverage for the National DPP lifestyle change program. Montana was the first state to achieve coverage. In 2016, NACDD, through CDC funding, awarded Maryland and Oregon a grant to promote Medicaid delivery models for the National DPP lifestyle change program through Medicaid managed care organizations (MCOs) and/or accountable care organizations (i.e., the Medicaid Coverage for the National DPP Demonstration Project).The Demonstration Project has served as a catalyst for further state coverage, generating significant progress in other states. States have been integrating the National DPP lifestyle change program into their Medicaid program through Medicaid State Plans, 1115 waivers, MCO pilots, and additional mechanisms.
States that expanded Medicaid under the Affordable Care Act (ACA) have also seen their diabetes rates increase in their Medicaid populations, underscoring the need to target prevention. The demographics of the covered populations under “traditional” Medicaid programs (i.e., those states that have not expanded Medicaid eligibility) primarily include pregnant women, children under the age of five years, physically and mentally disabled persons who qualify for social security, persons who have substance abuse (addiction) issues, and adults in long-term care. In states that have expanded Medicaid eligibility, the federal government will cover 90% of the cost of direct services provided to newly eligible childless adults up to 138% of the federal poverty level (FPL). These states may be more likely to consider coverage for the National DPP lifestyle change program, as it may be more relevant and financially impactful for their covered population.
Please see the map below for the national picture of Medicaid coverage, and visit the State Stories of Medicaid Coverage page to learn more about these states’ journeys to coverage. Below the map is a definition of each coverage mechanism used to cover the National DPP lifestyle change program in Medicaid.
Resources for making the case for coverage for the National DPP lifestyle change program in Medicaid are available here.
State Medicaid Coverage Map
The map below provides information on which states offer coverage for the National DPP lifestyle change program for Medicaid program enrollees. Click on a highlighted state in the map below to learn more.
Current as of 7/29/2024
Hover over the ![]() for more information.
for more information.
Medicaid Coverage Timeline: State Effective Dates
Print State Medicaid Coverage Timeline
State Medicaid Coverage Filterable Table
The table below can be filtered and ordered to show specific details. To filter, select an option from the drop-down boxes at the top of the table. To clear a selected filter, click on the filter name under the drop-down options. To order ascending/descending, click on the title row of the column by which sorting is desired. There is also a search function that can be used for keyword searching in the table (e.g., searching “2019” will return rows that have 2019 in the row).
| State | Effective Date | Coverage Mechanism | Delivery Method | Eligibility Requirements | Total Possible Reimbursement | Number of Medicaid Beneficiaries in State* | % of Medicaid Population in Comprehensive Managed Care** | State Story Link | |
|---|---|---|---|---|---|---|---|---|---|
| Arizona | 2022 | State-Supported MCO/Value-Based Care Pilot | 2,013,348 | 85% | |||||
| California | 2019 | State Plan Amendment (SPA) (New) | In-person, online, distance learning, and combination | $536 (2-year total) | 13,016,208 | 82% | State Story | ||
| Colorado | 2018 | State Medicaid Agency Decision | 1,316,543 | 10% | |||||
| Delaware | 2019 | Required Statewide MCO Coverage | In-person and online | Medicaid members who have been referred through a physician referral or self-referral | 248,794 | 85% | |||
| Idaho | 2023 | State Medicaid Agency Decision | 375,710 | 7% | |||||
| Illinois | 2021 | State Plan Amendment (SPA) (New) | In-person, online, and distance learning | Medicaid members between 18-64 years old, who are overweight or obese and have elevated blood glucose level or history of gestational diabetes; referral is not required | $670 | 3,143,105 | 74% | State Story | |
| Kansas | 2022 | State-Supported MCO/Value-Based Care Pilot | 413,787 | 88% | |||||
| Kentucky | 2021 | Voluntary MCO Offering | Online (LARK, can contact live Lifestyle Coach but mostly AI-driven) | Online questionnaire based on CDC risk screener (does not ask about A1C) | 1,503,931 | 91% | |||
| Maine | 2024 | State Plan Amendment (SPA) (New) | In-person, online, and distance learning | A MaineCare member meeting the CDC’s National DPP Lifestyle Change Program participant eligibility criteria with a referral from a physician or otherwise qualified provider | $768 (100% Medicare current total reimbursement rate + maximum performance payments per member based on weight loss or HBA1C) | N/A | N/A | ||
| Maryland | 2019 | 1115 Waiver | In-person, online, distance learning, and combination | Medicaid beneficiaries must receive services through a HealthChoice MCO, be between 18-64 years old, be overweight or obese, and have an elevated blood glucose level OR history of gestational diabetes mellitus (GDM) | $670 | 1,483,337 | 85% | State Story | |
| Michigan | 2023 | State Plan Amendment (SPA) (New) | In-person, online, and distance learning | Beneficiaries must also have a referral to the program by a licensed health care provider. | $768 | 2,573,851 | 75% | State Story | |
| Minnesota | 2016 | Medicaid State Plan (Existing) | In-person | Medicaid beneficiaries must have a diagnosis of prediabetes by a qualified physician | $300 | 1,119,244 | 84% | State Story | |
| Missouri | 2020 | State Plan Amendment (SPA) (New) | In-person, online, distance learning, and combination | Medicaid members who are 21 years of age and older who are overweight and have elevated blood glucose level. Services require a referral or prescription from a physician or other licensed practitioner | $577 (1 year plus 4 additional maintenance sessions for qualifying participants) | 939,919 | 70% | ||
| Montana | 2012 | State Plan Amendment (SPA) (New) | In-person and distance learning | Self-referral with physician approval before starting the program | $640 | 263,872 | 0% | State Story | |
| New Jersey | 2020 | State Plan Amendment (SPA) (New) | 1,683,987 | 94% | |||||
| New York | 2020 | State Plan Amendment (SPA) (New) | In-person | A referral must be written by a physician, physician assistant (PA), nurse practitioner, or midwife to participate in the National DPP | $554 | 6,458,770 | 74% | State Story | |
| North Carolina | 2022 | 1115 Waiver | In-person, online ("offered in a community setting, clinical setting, or online, as part of the approved DPP curriculum" | Eligible Medicaid managed care members must live in a Healthy Opportunities Pilot region and have at least one qualifying physical or behavioral health condition and one qualifying social risk factor. | $379 | 2,266,262 | 0% | ||
| North Dakota | 2022 | Voluntary MCO Offering | Coverage extends to Medicaid expansion population only, a total of 26,000 adults as of October 2022 (KFF, 2022) | 94,716 | 23% | ||||
| Ohio | 2022 | State Medicaid Agency Decision | In-person, online | Medicaid members eligibility should align with the National Diabetes Prevention Program requirements. Additionally, a prediabetes risk test is an acceptable eligibliity option for Ohio Medicaid members. | $920 (2-year total in-person), $1,176 (2-year total online) | 2,973,911 | 87% | State Story | |
| Oregon | 2019 | 1115 Waiver | In-person, online, distance learning, and combination | Blood test required (only for those without an overweight or obese diagnosis) | $1,196 (2-year total in-person), $1,176 (2-year total online) | 1,159,844 | 84% | State Story | |
| Pennsylvania | 2020 | Required Statewide MCO Coverage | In-person, online, distance learning, and combination | Medicaid beneficiaries may need to have a referral from a physician to be eligible for the National DPP lifestyle change program. Each MCO determines whether a referral is required. | MCOs determine reimbursement rate | 2,984,420 | 92% | State Story | |
| Rhode Island | 2021 | State-Supported MCO/Value-Based Care Pilot | 309,491 | 86% | |||||
| South Dakota | 2019 | Medicaid State Plan (Existing) | In-person and online | Medicaid beneficiaries must present a South Dakota Mediciad Identification card and have a provider check their eligibility through the state online portal. | $476 (for seven beneficiaries served and one hour total of instruction time) | 123,000 | 65% | ||
| Utah | 2022 | State Legislative Decision | In-person and online | $26.45 per session/$581.90 for 22 sessions | 342,000 | 80% | |||
| Vermont | 2012 | 1115 Waiver | 1,473,316 | 68% | |||||
| Virginia | 2020 | State-Supported MCO/Value-Based Care Pilot | MCOs determine reimbursement rate | 174,068 | 95% | ||||
| Washington | 2022 | State-Supported MCO/Value-Based Care Pilot | 1,830,122 | 88% | |||||
| Wisconsin | 2023 | State-Supported MCO/Value-Based Care Pilot | 1,308,070 | 67% | State Story | ||||
| Wyoming | 2020 | Medicaid State Plan (Existing) | Online, distance learning, and combination | Allowing individuals under 18 years of age to participate. Participants must meet pre-diabetes criteria. Blood test required. | $418 | 62,946 | 0% |
*Source: Medicaid.gov, 2020 Managed Care Summary; Data.Medicaid.gov
**Source: Kaiser Family Foundation, Total Medicaid MCO Enrollment, Timeframe: 2020
A map showing states with Medicaid managed care, and the proportion of state Medicaid beneficiaries enrolled in comprehensive managed care is available here.
If there are additional states or MCOs covering the National DPP lifestyle change program in Medicaid that have not been included above, or if you have coverage updates for any states or MCOs included above, please let us know by filling out the Add or Update a Payer or Employer Form at the bottom of this page.
Add Or Update a Payer or Employer
Know of a payer or employer covering the National DPP lifestyle change program not included on this page? Does a payer or employer need to be deleted from this page?









