Medicaid → Medicaid Coverage → Attaining Coverage Through a Medicaid State Plan
Attaining Coverage Through a Medicaid State Plan
After a state has made the decision to cover the National Diabetes Prevention Program (National DPP) lifestyle change program in Medicaid, either through legislation or administrative rules, the state will determine how to claim federal Medicaid matching funds for the program. The most common way to claim federal Medicaid matching funds is by including the benefit in the Medicaid State Plan. If the policies or processes the state intends to implement for the National DPP lifestyle change program cannot be accomplished through the Medicaid State Plan, the state may choose to use a section 1115 demonstration waiver or another mechanism (see the Engaging MCOs to Attain Coverage page for examples of other mechanisms).
This page describes how the National DPP lifestyle change program can be included in a state’s Medicaid State Plan, and includes the following topics:
- What is a Medicaid State Plan and a State Plan Amendment?
- When is a State Plan Amendment Needed?
- Medicaid State Plan Examples
- Other Program Costs
- Obtaining an Additional 1% Federal Medicaid Match: U.S. Preventive Services Task Force (USPSTF)
What is a Medicaid State Plan and a State Plan Amendment?
A Medicaid State Plan is a written agreement between a state and the federal government outlining the details of the state’s Medicaid program, including benefits, provider rate methodologies, and who is eligible for coverage. It gives an assurance that a state will abide by federal rules, which allows the state to claim federal Medicaid matching funds. See California’s Medicaid State Plan for an example of how a Medicaid State Plan is organized.
To make changes to the Medicaid State Plan, a state submits a state plan amendment (SPA) to the Centers for Medicare and Medicaid Services (CMS) for review and approval. An approved SPA results in permanent changes to the state’s Medicaid program, and may include content such as the addition of new populations or providers, changes in benefit coverage, changes in what administrative expenditures the state expects the federal government to pay for (such as processing claims, care coordination, risk stratification, transportation, etc.), and changes in reimbursement methodologies.
CMS’ SPA review and approval process can be relatively quick for standard changes, most of which are enacted by the state in advance of formal approval by the federal government. These changes are effective back to the first day of the quarter in which the SPA was submitted. For less common changes, a state can support the likelihood of a SPA being approved in a timely way by engaging in calls with CMS prior to submission. This allows the state and CMS to discuss potential concerns with the SPA and gives the state the opportunity to make changes. The pre-SPA submission calls New York held with its regional CMS representatives aided in the expedited approval of the SPA, which took just over two months after the SPA was submitted.
It is important to note that CMS’ approval of SPAs is guided by the statutory and regulatory terms and conditions of the Medicaid program including, but not limited to:
- Comparable benefits must be available to all eligibility groups to which the benefit package applies;
- Benefits must be offered statewide; and
- Beneficiaries must have the freedom to choose their provider (some exceptions exist with managed care).
A searchable list of SPAs that have been approved by CMS can be found here.
A state could also consider using a 2703 Medicaid Health Home SPA to secure federal Medicaid matching funds for the National DPP lifestyle change program for a subset of the Medicaid population.
What are Federal Medicaid Matching Funds?
Medicaid services are paid for through funding from both state and the federal governments, where the federal government matches state Medicaid spending according to a formula set in federal Medicaid law.
Federal Medicaid matching funds can be claimed for both direct service costs as well as administrative costs. The amount the federal government reimburses for direct service costs ranges from 50% to 100%, depending on the state’s Federal Medical Assistance Percentage (FMAP), the type of service delivered, and the location where the service is provided. Administrative costs are generally shared between the federal government and the state at a rate of 50/50, or in some cases at a higher rate of 75/25 or 90/10.
To claim federal Medicaid matching funds for the National DPP lifestyle change program, a state must have approval from the federal government through a Medicaid State Plan, a section 1115 demonstration waiver, or another mechanism (see the Engaging MCOs to Attain Coverage page for examples of other mechanisms).
A state could also choose to provide Medicaid coverage of the National DPP lifestyle change program using only state funds.
When is a State Plan Amendment Needed?
A state that wants to use a Medicaid State Plan to claim federal Medicaid matching funds for covering the National DPP lifestyle change program must determine whether:
- There is existing language in the Medicaid State Plan that would include the National DPP lifestyle change program in the way the state intends to implement it.
- If this is the case, a SPA is not needed to claim federal Medicaid matching funds for the program.
- E.g., Minnesota did not need a new SPA because the Medicaid State Plan already included language defining preventive services that was broad enough to encompass the National DPP lifestyle change program and covered services provided by community health workers (CHWs).
OR
- Changes need to be made to the Medicaid State Plan to include the National DPP lifestyle change program in the way the state intends to implement it.
- If this is the case, the changes can be made through a SPA.
- E.g., See the State Plan Amendment Examples section below for details on California’s, Montana’s, and New York’s approved SPAs.
There are a variety of reasons why a state may need to make changes to the Medicaid State Plan through a SPA to claim federal Medicaid matching funds. Two of the most common are:
- The Medicaid State Plan does not include language on services that would allow for coverage of the National DPP lifestyle change program for the target population(s).
- The Medicaid State Plan does not currently permit Medicaid reimbursement of the health care providers or organizations that the state intends to allow to deliver the National DPP lifestyle change program to Medicaid beneficiaries.
Other information that would be detailed in a National DPP lifestyle change program SPA includes the reimbursement rate, the date program coverage becomes effective, and program training requirements.
1. The Medicaid State Plan does not include language on services that would allow for coverage of the National DPP lifestyle change program for the target population(s).
If there is not an existing preventive service in the Medicaid State Plan that would incorporate the National DPP lifestyle change program for the desired populations, a SPA may be needed to claim federal Medicaid matching funds.
In Medicaid, “preventive services” are defined as services recommended by a physician or other licensed practitioner to:
- Prevent disease, disability, and other health conditions or their progression;
- Prolong life; and
- Promote physical and mental health and efficiency. (42 CFR 440.130(c))
To qualify for Medicaid coverage, preventive services must be medical or remedial in nature, which means they must:
- Involve direct patient care; and
- Be for the express purpose of diagnosing, treating or preventing illness, injury, or other impairments to an individual’s physical or mental health.
Preventive services must also meet additional provisions outlined in the State Medicaid Manual, Chapter 4, Section 4385. For example, nonmedical preventive services that are applied at the community level or that address broader social or environmental concerns are not covered by Medicaid (e.g., counseling on the importance of smoke detectors, dust-mite proof bedding, lead abatement activities, and community water fluoridation).
Qualifying National DPP Lifestyle Change Program Services
Services provided through the National DPP lifestyle change program that qualify for Medicaid coverage as preventive services include:
- Intensive behavioral counseling; and
- Other preventive services for the express purposes of preventing type 2 diabetes.
California’s SPA and New York’s SPA are examples of how the National DPP lifestyle change program aligns with 42 CFR 440.130(c).
Preventive services are subject to the general terms and conditions of the Medicaid program including, but not limited to:
- Comparable benefits must be available to all eligibility groups to which the benefit package applies;
- Benefits must be offered statewide; and
- Beneficiaries must have the freedom to choose their provider (some exceptions exist with managed care).
Coordinating with Public Health
Coordinating the provision of preventive services with other state and federal programs, like public health, can help avoid duplication of services. Generally, coordination can be achieved through the establishment of interagency agreements, informal cooperative arrangements, and increased referrals between the Medicaid agency and other programs that offer preventive care.
2. The Medicaid State Plan does not currently permit Medicaid reimbursement of the providers or organizations that the state intends to allow to deliver the National DPP lifestyle change program to Medicaid beneficiaries.
A state will need to seek a SPA if the Medicaid State Plan does not currently permit Medicaid payment to the health care providers or organizations the state intends to reimburse for delivering the National DPP lifestyle change program to Medicaid beneficiaries.
Both health professionals and non-licensed personnel can be National DPP lifestyle change program lifestyle coaches. However, the types of providers and organizations that can become Medicaid enrolled providers and be reimbursed by Medicaid is determined by each state. Some states use existing Medicaid enrolled provider types, such as community health workers (CHWs), nurses, registered dieticians, clinics, or hospitals (see the Minnesota example below). Other states create a new provider type (see the New York SPA below for an example).
For more information on using an existing provider type or creating a new provider type, see the Determining the Medicaid Enrolled Provider Type page. Additional information on utilizing CHWs as lifestyle coaches can be found on the Use an Existing Provider Type page.
State Plan Amendments: Preventive Services Rule Change
In states where it is necessary to change or broaden the state Medicaid authority to cover non-licensed personnel to serve as lifestyle coaches, states could consider a SPA based on CMS’ Preventive Services Rule Change.
Under the Preventive Services Rule Change to 42 CFR 440.130(c) issued by CMS in 2013, states can offer Medicaid services that are provided by non-licensed staff. Under the old rules, preventive services could only be provided by a physician or “other licensed practitioner (OLP) of the healing arts” to qualify for Medicaid reimbursement. The amended rule allows other practitioners to provide and be reimbursed as long as they are furnishing preventive services “recommended by a physician or other licensed practitioner of the healing arts acting within the scope of authorized practice.” How the term recommended is interpreted will vary on a state-by-state basis and be defined through SPA language. Some states may require that the services be ordered by licensed health professionals, while others may require some type of supervision by a physician or nurse practitioner.
States pursuing a SPA based on the Preventive Services Rule Change will need to define the preventive services being covered, the provider qualifications, the process for ensuring that appropriate services are being delivered by qualified providers, and the reimbursement methodology. Any required education, training, experience, credentialing, or registration information should also be included. For an example, see New York’s SPA below.
For more information about the Preventive Services Rule Change, see the Center for Medicaid & CHIP Services (CMCS) Information Bulletin and a presentation prepared by CMS entitled, “Medicaid Preventive Services: Regulatory Change.”
Medicaid State Plan Examples
California
California submitted a SPA to CMS on December 26, 2018 to secure federal Medicaid matching funds for the National DPP lifestyle change program. The SPA was approved by CMS on October 24, 2019, with an effective date of January 1, 2019. The SPA creates a new provider type to allow CDC-recognized organizations to be reimbursed by Medicaid. To learn more about how California is covering the National DPP lifestyle change program in its Medicaid program (Medi-Cal), see the California State Story of Medicaid Coverage page of the Coverage Toolkit.
California’s SPA Language:
National DPP Lifestyle Change Program Description
“DPP services are a set of medically necessary services recommended by a physician or other licensed practitioner of the healing arts to prevent or delay the onset of type 2 diabetes for beneficiaries with indications of prediabetes, in accordance with 42 CFR 440.130(c).
DPP services provide a variety of behavioral and nutritional interventions identified as evidence-based by clinical research or studies and/or nationally recognized organizations specializing in disease control and prevention.
Medically necessary DPP services are provided during sessions that occur at regular, periodic intervals over the course of one year, and, if eligible based upon individual measurable health outcomes, additional ongoing maintenance sessions at regular, periodic intervals for another year. At these sessions, DPP services include:
- Individual or group nutrition or behavioral counseling.
- Physical activity and fitness assessments.
Comparable services are available to children under age 18, pursuant to the EPSDT.”
Lifestyle Coaches
“A DPP services provider must be an organization enrolled in Medi-Cal and must have either pending, preliminary, or full recognition by the Centers for Disease Control and Prevention (CDC) for DPP. DPP services providers use lifestyle coaches for delivery of DPP services.
DPP services are delivered by lifestyle coaches and must have completed nationally-recognized training for delivery of DPP services. Lifestyle coaches may be:
- Physicians
- Licensed nonphysician practitioners, such as nurses, and physical therapists.
- Unlicensed practitioners under the supervision of a DPP services provider or a licensed Medi-Cal practitioner.
For DPP services delivered by unlicensed lifestyle coaches, the supervising Medi-Cal practitioner will assume professional liability for care of that patient and furnish services within its scope of practice according to state law.
All lifestyle coaches must complete at least 12 hours of training in DPP services from an organization recognized by the CDC for DPP. All lifestyle coaches must be trained to the specific curriculum being used by the recognized organization before offering their first class.”
Reimbursement
“Effective January 1, 2019, the reimbursement rates for Diabetes Prevention Program (DPP) services will be set at no more than 80 percent of the corresponding Medicare rate for the same or similar service. Any rate reflected at or below 80 percent will not be decreased until federal approval is obtained.
Except as otherwise noted in the State plan, state-developed fee schedules are the same for both governmental and private providers of DPP services. The department’s fee schedule rates were set as of January 1, 2019 and are effective for services provided on or after that date.” Bolding added for emphasis.
Illinois
Illinois submitted a SPA to CMS on July 21, 2021 to secure federal Medicaid matching funds for the National DPP lifestyle change program. The SPA was approved by CMS on February 4, 2022, with an effective date of August 1, 2021.
A provider notice of coverage was published on July 29, 2022 describing billing updates for the National DPP lifestyle change program and Diabetes Self-Management Education and Support (DSMES) services in Illinois. The provider notice clarified that while health care providers and MCOs can recommend Medicaid beneficiaries to the program, a formal referral is not required to participate.
Illinois’ SPA Language:
“DPP services must be recommended by a physician or other licensed practitioner of the healing arts acting within the scope of authorized practice under State law to prevent diabetes or the progression of diabetes, prolong life, and/or promote the physical and mental health of the beneficiary. Services include counseling related to long-term behavior change, including diet, physical activity, and strategies for weight control. DPP services are provided during sessions that occur at regular, periodic intervals over the course of one year.
CDC-recognized organizations with type 2 diabetes prevention programs with active pending, preliminary or full recognition status are eligible to enroll as a Medicaid Diabetes Prevention Program (DPP) Provider type. DPP services are delivered by Lifestyle Coaches who have completed nationally recognized training for delivery of such services. Providers of these services include physicians, nonphysician licensed practitioners and unlicensed practitioners under the supervision of a DPP service provider or licensed practitioner.
For DPP services delivered by unlicensed Lifestyle Coaches, the supervising practitioner will assume professional liability for the care of the patient and furnish services with its scope of practice according to state law.”
To learn more about how Illinois is covering the National DPP lifestyle change program in its Medicaid program, see the Illinois State Story of Medicaid Coverage page of the Coverage Toolkit.
Maine
Maine submitted a SPA to CMS on December 6, 2023, to secure federal matching funds for the National DPP lifestyle change program. The SPA was approved by CMS on March 15, 2024, with an effective date of January 1, 2024. The SPA sets forth program standards and a reimbursement method, specifically a session-based rate and a performance-based payment.
MaineCare (Maine Medicaid) published a section on the National DPP lifestyle change program benefit in their MaineCare Benefits Manual in November 2023 describing member eligibility, provider requirements, covered services, policies and procedures, and reimbursement and billing instructions.
Maine SPA language:
“Session Rate:
The allowed amount for each National OPP LCP session is I 00% of Medicare’s current total reimbursement for all sessions in the Medicare Diabetes Prevention Program (MDPP), without reimbursement related to weight loss included, divided by the total number of sessions required by the most current version 0f the CDC Diabetes Prevention Recognition Program Standards and Operating Procedures (DPRP Standards).
Performance Payment:
Providers are also eligible for no more than two performance payments per member if the member achieves associated weight loss or HbA1C goals. The allowed amount for each performance payment is 100% of Medicare’s current maximum reimbursement for additional payments related to weight loss in the MDPP, divided by two (2).
- First Performance Payment. Providers may bill once for the first performance payment for each member who achieves one of the following:
- At least 5% weight loss from the first recorded weight compared to the weight recorded at any session during months seven (7) to eleven (11); or
- At least 0.2% reduction in HbA1C achieved at any points during months seven (7) to eleven (11) as compared to the HbA1C level indicated by a test taken no more than twelve (12) months prior to the date of the first session.
- Second Performance Payment. Providers may bill once for a second performance payment for each member who achieves one of the following.
- At least 5% weight loss from the first recorded weight compared to the weight recorded at the twelfth month session; or
- At least a 0.2% reduction in HbA1C achieved at any point during the twelfth month as compared to the HbA1C level indicated by a test taken no more than twelve (12) months prior to the date of the first session.
The twelfth month performance payment is billable regardless of whether the member met the minimum 5% weight loss or the minimum 0.2% reduction in HbA1C required for the first performance payment in months 7-11. Providers may bill both performance payments regardless of the number of sessions members attend, as long as the weight loss or HbA1C reduction is achieved during the applicable program month(s).”
Michigan
Michigan finalized a SPA, effective as of July 1, 2023, to secure federal Medicaid matching funds for the National DPP lifestyle change program (pages 442 and 915). The SPA creates a new provider type to allow CDC-recognized organizations to be reimbursed by Medicaid. To learn more about how Michigan is covering the National DPP lifestyle change program in its Medicaid program see the Michigan State Story of Medicaid Coverage page of the Coverage Toolkit and the MDHHS Michigan Medicaid Policy Bulletin.
Michigan’s Medicaid State Plan Language (see page 441):
“c. Preventive Services (Continued) – Diabetes Prevention Effective May 1, 2023, the program covers the Michigan Medicaid Diabetes Prevention Program (MiDPP) as a preventive service. MiDPP meets all requirements for the Centers for Disease Control and Prevention (CDC) National Diabetes Prevention Program (NDPP) and preventive service requirements in 42 CFR Section 440.130 (c). The NDPP is an evidence-based, educational support program designed to assist at-risk individuals from developing Type 2 diabetes.
The Public Health Administration (PHA) within the Michigan Department of Health and Human Services (MDHHS) ensures provider qualification utilizing CDC recognition requirements. MiDPP providers and lifestyle coaches must be approved by the MDHHS PHA before enrolling with the Michigan Medicaid program. All enrolled lifestyle coaches must be associated with an enrolled MiDPP provider. Services are recommended by a physician or other licensed practitioner of the healing arts within their scope of practice. MiDPP services include:
- Group sessions related to long-term dietary change, increased physical activity and behavior change strategies for weight control.
- Group support and skill building to facilitate the knowledge, skill, and ability necessary to prevent the onset of Type 2 diabetes.”
Minnesota
On January 1, 2016, Minnesota began offering the National DPP lifestyle change program as a covered benefit for Medicaid beneficiaries under existing Medicaid State Plan authority. The state was able to claim federal Medicaid matching funds for including the program without the submission of a new SPA, an 1115 demonstration waiver, or another mechanism. Minnesota’s Medicaid State Plan already included language defining preventive services that was broad enough to encompass the National DPP lifestyle change program and covered services provided by community health workers (CHWs).
Minnesota Medicaid requires the following of CHWs to deliver the National DPP lifestyle change program:
- CHWs must work under the supervision of a physician, dentist, advanced practice registered nurse (APRN), certified public health nurse (PHN), mental health professional, or registered nurse to provide patient education for health promotion and disease management services.
- CHWs cannot bill Medicaid directly (i.e., they are the rendering provider).
- CHWs must have a valid certificate from the Minnesota State Colleges and Universities (MnSCU), demonstrating that the applicant has completed an approved community health worker curriculum.
- CHWs must be affiliated with a CDC-recognized organization and trained as a lifestyle coach.
CHW services are diagnosis-related medical interventions, not social services. Medicaid coverage includes diagnosis-related patient education services, including diabetes prevention and pediatric obesity treatment under specified criteria, including:
- The service involves teaching the patient how to self-manage their health effectively in conjunction with the health care team; and
- The service is provided face-to-face with the recipient (individually or in a group) in an outpatient, home, clinic, or other community setting.
For more information about the Minnesota’s benefit see:
Missouri
Missouri submitted a SPA to CMS on March 2, 2020, to cover the National DPP lifestyle change program in Medicaid. The SPA was approved by CMS on August 7, 2020, with an effective date of September 1, 2020. To learn about Missouri’s reimbursement structure, visit the Reimbursement Models for Medicaid Agencies and MCOs page of the Coverage Toolkit.
Missouri’s SPA Language:
Diabetes Prevention Program Services
“Diabetes Prevention Program (DPP) services are a set of structured, medically necessary services recommended by a physician or other licensed practitioners of the healing arts to prevent or delay the onset of type 2 diabetes for participants ages twenty-one (21) years of age and older who are at risk for diabetes or have indications of prediabetes, in accordance with 42 CFR 440.130(c).
DPP services provide a variety of behavioral and nutritional interventions identified as evidence based by clinical research or studies and/or nationally recognized organizations specializing in disease control and prevention. DPP services are provided during sessions that occur at regular, periodic intervals over the course of one year, and, if eligible based upon individual measurable health-outcomes, additional ongoing maintenance sessions at regular, periodic intervals for another year. At these sessions, DPP services include:
- Ongoing nutrition or behavioral counseling focusing on weight reduction and lifestyle changes.
- Physical activity and fitness assessments.
Additional DPP service requests beyond the initial allocation shall be requested through the prior authorization process and be deemed medically necessary.”
Diabetes Prevention Program Services – Qualified Providers
“A DPP service provider must be enrolled as a MO HealthNet provider and must have either pending, preliminary, or full recognition by the Centers for Disease Control and Prevention (CDC) for DPP.
DPP service providers use lifestyle coaches for delivery of DPP services to participants. The lifestyle coaches must have completed nationally recognized training for delivery of DPP services. Lifestyle coaches may be:
- Physicians
- Licensed nonphysician practitioners, such as nurses, and physical therapists.
- Unlicensed practitioners under the supervision of a DPP services provider or a licensed MO HealthNet practitioner.
For DPP services delivered by unlicensed lifestyle coaches, the supervising MO HealthNet provider will assume professional liability for care of the patient and furnish services within its scope of practice according to state law.
All lifestyle coaches must complete a minimum of 12 hours of training in DPP services from an organization recognized by the CDC for DPP.”
Diabetes Prevention Program (DPP) Services for Adults
“Reimbursement for services is made on a fee-for-service basis. MHD has determined the maximum allowable fee for a unit of service as a reasonable fee, consistent with efficiency, economy, and quality of care. The state payment for each service will be lower of:
- The provider’s actual charge for the services; or
- The Medicaid maximum allowable amount per unit of service.
Reimbursement shall be only for services authorized by the state agency or its designee. Except as otherwise noted in the plan, state-developed fee schedule rates are the same for both governmental and private providers of DPP services. The agency’s fee schedule rate was set as of September 1, 2020 and is effective for services provided on or after that date. All rates are published on the fee schedule: https://dss.mo.gov/mhd/providers/pages/cptagree.htm.” Bolding added for emphasis.
Montana
Montana’s approved SPA allows the delivery of its type 2 diabetes prevention program through several provider types.
Montana’s SPA Language:
“A. Services to prevent diabetes and cardiovascular disease provided to people at risk for diabetes and cardiovascular disease:
- 1. Group nutrition counseling to prevent diabetes and cardiovascular disease
B. Providers
- 1. Physicians,
- 2. Mid-level practitioners,
- 3. Registered dieticians who also hold a current Montana license as a nutritionist,
- 4. Hospitals,
- 5. Federally Qualified Health Centers,
- 6. Rural Health Clinics,
- 7. Indian Health Services/Tribal Health Services,
- 8. Groups/Clinics, or
- 9. Public Health Departments.
Listed providers will provide services for reimbursement under the diabetes and cardiovascular disease prevention program. Services for the program are limited to group nutrition and lifestyle counseling to prevent diabetes and cardiovascular disease.
A physician or mid-level practitioner supervising a provider not listed above, such as a licensed nurse, a certified diabetes educator, or an exercise physiologist, will assume professional liability for care of the patient and will furnish services within his or her scope of practice under State law.”
For more information on Montana Medicaid’s implementation of the National DPP lifestyle change program, visit the Montana State Story of Medicaid Coverage page of the Coverage Toolkit.
New York
On April 12, 2019, the New York State (NYS) legislature amended its social services law to include the National DPP lifestyle change program within the definition of “standard coverage” for medical assistance for needy persons. Amending the social services law also authorized CDC-recognized organizations to enroll in NYS Medicaid and receive Medicaid reimbursement. To learn more, see the Role of the State Legislature in Medicaid Coverage page of the Coverage Toolkit.
To secure federal Medicaid matching funds for the program NYS Medicaid submitted a SPA on June 28, 2019, which was approved by CMS on September 4, 2019. Pre-SPA submission calls with NYS’s regional CMS representatives may have expedited its approval.
New York State’s SPA covers the National DPP lifestyle change program as a preventative service. Only organizations that have achieved CDC recognition can be enrolled in Medicaid to bill for providing the National DPP lifestyle change program to Medicaid members.
New York State’s SPA Language
“For dates of service on or after July 1, 2019. Medicaid will begin covering diabetes prevention services as outlined in the Centers for Disease Control and Prevention (CDC)-recognized National Diabetes Prevention Program (NDPP). The NDPP is an evidence-based, educational and support program designed to assist at-risk individuals from developing Type 2 diabetes. Diabetes services are provided as preventive services pursuant to 42 C.F.R. Section 440.130(c) and must be recommended by a physician or other licensed practitioner of the healing arts within his or her scope of practice under state law to prevent diabetes, prolong life, and promote the physical and mental health of the beneficiary.
The CDC grants NDPP recognition only to organizational entities. Therefore, only organizations that have achieved CDC recognition can be enrolled in Medicaid as an NDPP provider. Individuals who wish to participate in the Medicaid NDPP program may do so as a trained “Lifestyle Coach” once they meet the standards and guidelines specified in the CDC’s Diabetes Prevention Recognition Program (DPRP). Only the organizations that are enrolled in Medicaid as NDPP providers may bill for NDPP services. The CDC-recognized organization will supervise Lifestyle Coaches and must ensure that the individual Lifestyle Coaches providing NDPP services on behalf of the organization have been formally trained and have complied with the requirements outlined by the CDC.
A Lifestyle Coach may be a physician, non-physician practitioner, or an unlicensed person who has received formal training on a CDC-approved curriculum for at least 12 hours and is recognized as having met the NDPP requirements specified in the CDC’s Diabetes Prevention Recognition Program (DPRP) standards and guidelines.
Lifestyle Coaches will work with Medicaid members to provide them with a practical understanding of the positive impacts of healthier, sustained dietary habits; increased physical activity; and behavior change strategies for weight control; and will offer the following services with the goal to prevent Type 2 diabetes:
- Counseling related to long-term dietary change, increased physical activity, and behavior change strategies for weight control;
- Counseling and skill building to facilitate the knowledge, skill, and ability necessary to prevent the onset of Type 2 diabetes; and
- Nutritional counseling.
Reimbursement Methodology: Attachment 4.19-B Effective July 1, 2019, the Medicaid rate for NDPP services will be set at 80 percent of the corresponding 2019 Medicare NDPP rate for the same or similar service.” Bolding added for emphasis.
To learn more about coverage of the National DPP lifestyle change program in NYS, visit the New York State Story of Medicaid Coverage page of the Coverage Toolkit.
Wyoming
Beginning in January 2020, Wyoming Medicaid opened codes allowing registered dieticians to be reimbursed for delivering the National DPP lifestyle change program to Medicaid beneficiaries. Because registered dieticians offering dietician services were already included in Wyoming’s Medicaid State Plan, a SPA was not needed to claim federal Medicaid matching funds.
The registered dieticians do not need to be affiliated with a CDC-recognized organization to be reimbursed. To learn about Wyoming’s reimbursement structure, visit the Reimbursement Models for Medicaid Agencies and MCOs page of the Coverage Toolkit.
Enrolled providers can be reimbursed for delivering the program to Medicaid beneficiaries in-person, through distance learning, or through a combination approach, but the first session must be in-person. Wyoming Medicaid is allowing telephonic services for the duration of COVID-19 to help address the inability to meet in-person.
To be eligible to participate in the program, Medicaid beneficiaries in Wyoming must have received a blood test with a prediabetes diagnosis within the past year or have a previous gestational diabetes diagnosis. Eligible individuals under the age of 18 are permitted to enroll in the program. Medicaid beneficiaries in Wyoming can participate in the program twice per lifetime.
More information regarding the implementation of this benefit can be found in Chapter 17 of Wyoming’s Medicaid Policy Bulletin.
Ensuring Covered Services are Included in Medicaid Managed Care
Following the decision to cover the National DPP lifestyle change program and the approval of a SPA, states should also ensure the program is included in any relevant MCO regulations that outline required covered services in managed care. For example, Maryland has a Code of Maryland Regulations that outlines all required Maryland HealthChoice (Maryland’s managed care program) benefits. When the National DPP lifestyle change program was added as a covered benefit in Maryland Medicaid via a section 1115 demonstration waiver, these regulations were amended to include the program. Other states may not specify this level of program detail through regulation, but require that MCOs cover “all state plan services” or give their Medicaid agencies the discretion to determine what services to include in the MCO contracts and which ones to carve out.
States should seek to understand their unique regulatory environment to determine what steps, if any, are necessary to ensure coverage of the National DPP lifestyle change program in managed care once it becomes a state plan benefit.
Other Program Costs
It is important to note that other services and costs associated with the National DPP lifestyle change program will not qualify as preventive services and may or may not be eligible for drawing down federal Medicaid matching funds.
A list of additional services and costs associated with the National DPP lifestyle change program and whether they are eligible for federal Medicaid matching funds is provided below.
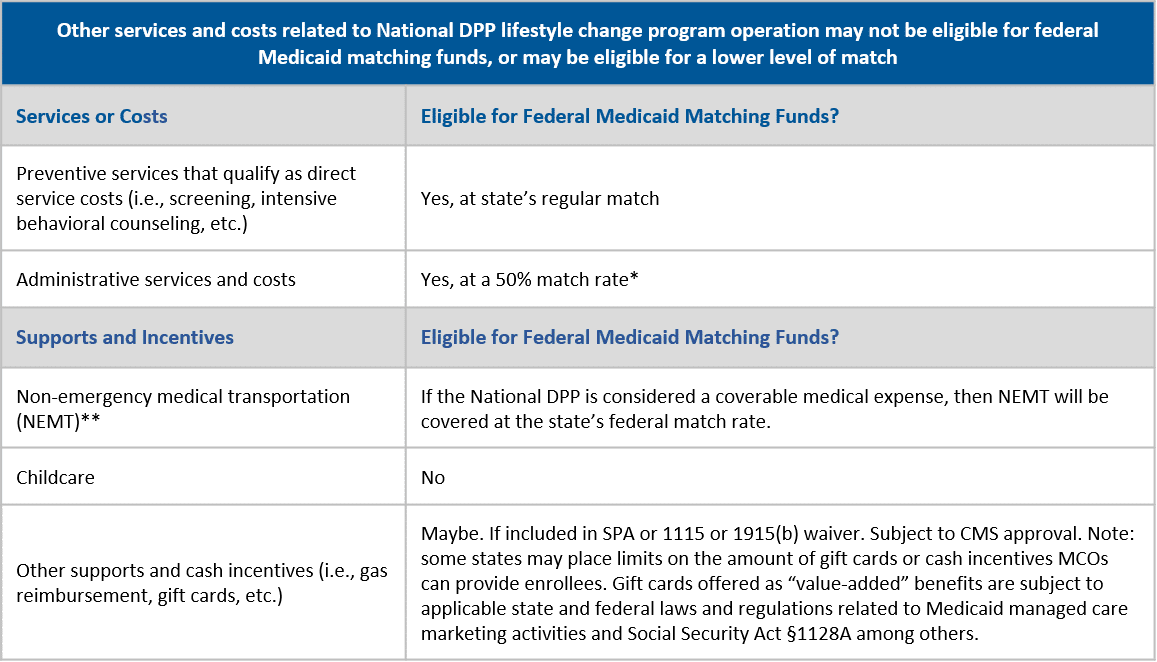
*In certain cases a higher administrative FMAP is allowed for medical professionals, which may be how a state chooses to administer the National DPP lifestyle change program. If a state contracts with Medicaid managed care organizations (MCOs) under a risk contract, amounts paid to the managed care plan to cover administrative functions are matched as a medical assistance cost at the applicable FMAP, not as an administrative cost (42 CFR 438.812). For more information, see MACPAC Federal Medical Assistance Percentage.
**Qualifying situations must follow federal regulations regarding NEMT.
Obtaining an Additional 1% Federal Medicaid Match: U.S. Preventive Services Task Force (USPSTF)
States can obtain a one percentage point federal match rate increase for covered preventive services when covering and reimbursing all USPSTF grade A and B preventive services and approved vaccines recommended by the Advisory Committee on Immunization Practices (ACIP), and their administration, without cost-sharing. If the state utilizes a managed care delivery system, it must also make these services available to those enrolled in managed care and the one percentage point increase will be applied to the managed care expenditures.
Covering the National DPP lifestyle change program at no cost to members may also aid states in securing this additional 1% federal Medicaid match. For states pursuing the one percentage point increase in their FMAP per Section 4106(b) of the ACA, the counseling requirements referenced in the following recommendations can be met through coverage of the National DPP lifestyle change program.
Prediabetes and Type 2 Diabetes: Screening
The USPSTF recommends screening for abnormal blood glucose in adults aged 35 to 70 years who are nonpregnant, overweight, or obese. Clinicians should offer or refer patients with abnormal blood glucose to effective preventive interventions.
The USPSTF recommends offering or referring adults who are overweight or obese and have additional cardiovascular disease (CVD) risk factors to intensive behavioral counseling interventions to promote a healthful diet and physical activity for CVD prevention. Impaired fasting glucose is listed as one such risk factor.
Coverage of the National DPP lifestyle change program is also indirectly related to two additional USPSTF grade A and B preventive services. These services reference National DPP lifestyle change program inclusion criteria.
Gestational Diabetes: Screening
The USPSTF recommends screening for gestational diabetes mellitus (GDM) in asymptomatic pregnant women after 24 weeks of gestation. Note: You cannot participate in the National DPP lifestyle change program if you are pregnant at the time of enrollment, but you are eligible if you were previously diagnosed with GDM (note that for Medicare DPP, a previous diagnosis of GDM is not sufficient for program eligibility).
Weight Loss to Prevent Obesity-Related Morbidity and Mortality in Adults: Behavioral Interventions
The USPSTF recommends screening all adults for obesity. Clinicians should offer or refer patients with a body mass index of 30 kg/m2 or higher to intensive, multicomponent behavioral interventions.
As stated in the Medicaid.gov Questions & Answers on ACA Section 4106 “All USPSTF grade A and B preventive services, Advisory Committee on Immunization Practices (ACIP) recommended vaccines, and their administration, must be covered without cost-sharing in order to be eligible for the one percentage point FMAP increase.”
In managed care environments, states will need to work with their MCOs to establish special codes and protocols to allow for an audit trail to determine the additional 1% is being properly claimed and that the costs are appropriately accounted for in rate setting for the MCOs.
For more information, see the quality metrics page or view the complete list of USPSTF grade A and B recommendations. Additionally, reference the USPSTF FAQ document housed under NACDD’s Diabetes Library. For more information and details about Section 4106(b), see CMCS State Medicaid Letter RE: Affordable Care Act Section 4106.